Lumbar puncture (LP) is a frequent procedure during the neonatal period. Correctly performing this technique can avoid many of its complications.
ObjectiveTo evaluate the LP procedure in neonates in Spanish hospitals, studying the type of material and the sedation-analgesia used.
Material and methodsCross-sectional study conducted in Spain gathering data through a survey research distributed by email through the Segurneo-SEN Hospital Network and the Spanish Neonatal Society. Data on the LP technique in neonates were collected.
ResultsA total of 301 participants were analysed. Most professionals used a trocar needle with a stylet as the first option (89.7%); however, when the LP failed or was blood-stained, 32.2% changed the type of needle. A total of 143 doctors gave their subjective feeling about the type of needle: they only use trocar needles with stylet (41.3%), the technique is easier using scalp-vein needles (32.2%), there is less probability of a blood-stained LP, or failed using scalp-vein needles (7.7%), they choose the type of needle depending on the size of the newborn (10.5%), indifference when using one type or another needle (8.4%). Almost all (99%) of the surveyed doctors used some type of analgesia. The most widely used measures were topical anaesthetics (90.3%) and sucrose (82.2%).
ConclusionsCurrently, the LP procedure in the neonatal period is mainly performed with a trocar needle with a stylet and with the widespread use of different analgesic measures.
La punción lumbar (PL) es un procedimiento que se realiza con frecuencia durante el período neonatal. Efectuar correctamente esta técnica puede evitar gran parte de sus complicaciones.
ObjetivoEvaluar el procedimiento de PL en neonatos en los hospitales españoles, estudiando el tipo de material empleado y la sedoanalgesia utilizada.
Material y métodosEstudio transversal basado en una encuesta escrita distribuida por correo electrónico a través de la Red de Hospitales Segurneo-SEN y la Sociedad Española de Neonatología, que recogía datos sobre la técnica de PL en neonatos.
ResultadosSe analizaron 301 encuestas respondidas. La mayoría de profesionales utilizaban aguja tipo trócar con estilete como primera opción (89,7%). No obstante, cuando la PL era fallida o hemática el 32,2% cambiaban el tipo de aguja. De total de médicos, 143 reflejaron su sensación subjetiva sobre el tipo de aguja: el 41,3% sólo empleaban agujas tipo trócar, al 32,2% la técnica les resultaba más fácil empleando agujas de tipo «palomilla», para el 7,7% existía menor probabilidad de PL hemática o fallida usando agujas de tipo «palomilla», el 10,5% elegían aguja dependiendo del tamaño del neonato, y un 8,4% eran indiferentes a utilizar un tipo u otro de aguja. El 99% de los encuestados usaban algún tipo de analgesia. Las medidas más utilizadas fueron anestésicos tópicos (90,3%) y sacarosa (82,2%).
ConclusionesActualmente, el procedimiento de PL en neonatos se realiza de forma mayoritaria utilizando agujas tipo trócar con estilete y con un uso extendido de diferentes medidas analgésicas para llevar a cabo la técnica.
Cerebrospinal fluid (CSF) analysis is a procedure that is performed frequently in the neonatal period as part of the diagnostic evaluation of newborn infants with suspected sepsis or for treatment purposes. Samples of CSF are obtained by lumbar puncture (LP), gaining access to the subarachnoid space at the level of the cauda equina through a needle. The technique was first described by Quincke in 1891.1,2
There are few contraindications for LP: raised intracranial pressure, bleeding diathesis, soft tissue infection at the site of puncture and cardiorespiratory instability. However, it is an invasive procedure that carries a risk of complications, some of which are due to inadequate technique. The most frequent complications are back pain at the level of the puncture site and post-puncture headache. Other complications that are less frequent but have been described in neonatal patients include transient neurologic manifestations (dysesthesias, nerve palsies), local infection and bleeding, cerebral herniation, CSF leaks into the epidural space, spinal epidermoid tumours (associated with insertion of the needle without a stylet) or neonatal hypoxia (resulting from airway obstruction caused by maintenance of a flexed position during the procedure). Most adverse events are mild and resolve spontaneously without intervention, but some require urgent diagnosis and treatment.1–9
In recent years, medical providers have been using two types of needles to perform LP in the neonatal period: atraumatic pencil-point needles inserted with a stylet and venepuncture butterfly needles inserted without a stylet.10,11 Although the use of needles without a stylet is currently contraindicated in LP, it is a surprisingly widespread practice in neonatal care, especially in small infants. A systematic review published in 2004 found that nearly 1/3 of members of the Section on Pediatric Emergency Medicine of the American Academy of Pediatrics advanced the needle in LP without the stylet in place.12 In Spain, a review published in 2012 found that the type of needle used most frequently for LP in newborn patients in different Spanish hospitals was the butterfly needle.13 A more recent study from 2020 found that the use of smaller-gauge needles (22G vs 25G Quincke needle) was associated with a lower incidence of traumatic PL in newborn infants, which suggested that a smaller gauge would be preferable for LP in this age group.14
In addition to the variations in the equipment used to perform LP, there are also differences in the use of sedation and analgesia during the procedure. Pain management is a human right, and physicians are increasingly aware of this need. Advances in neurobiology and clinical medicine made it possible to establish that foetuses and neonates can perceive pain, both acute and chronic.15 Neonatal units must introduce and implement pain management protocols including both pharmacological and nonpharmacological measures to alleviate pain.16
In the past, health care providers were extremely reluctant to use anaesthetic or analgesic drugs in neonates for different reasons, either based on the conviction that neonates could not feel pain due to incomplete myelination or on the potential risk of instability associated with their use in some infants. It was not until 1987 that the American Academy of Pediatrics, the Sections of Anaesthesiology and Surgery and the Committee on Fetus and Newborn recommended pain management in newborn infants.17 If we analyse analgesia in newborn infants specifically for performance of LP, we must take into account that the use of topical anaesthetics, which is now a standard of care, was strongly opposed by significant stakeholders in the late 1990s. It was believed that infiltration of local anaesthetics could obscure anatomical landmarks, making the procedure difficult and therefore increasing the risk of traumatic LP.18 There were also concerns about their use in neonates due to a hypothetical risk of methaemoglobinaemia derived from the ability of prilocaine metabolites to oxidise haemoglobin.19,20 In a few years, the evidence demonstrated that use of local anaesthesia during LP was not only advisable but was also associated with an increased success rate for the procedure.18,21–23 Yet, many of the current clinical guidelines on the prevention and management of pain in neonates during performance of LP only mention the use of topical anaesthetics, which numb the skin but not the subcutaneous tissue, and/or sucrose administration, measures that may be insufficient.24–26 Some authors advocate for local infiltration of lidocaine for performance of LP in neonates and infants.18,27 Other studies focused on the performance of LP in the fields of anaesthesia and oncology support the use of intravenous analgesics and anaesthetics for the procedure.28–31
In this context, and in the framework of a broader research project conducted in newborn infants that required performance of a LP, we decided to perform this study.
Material and methodsWe conducted a cross-sectional study with the aim of evaluating the performance of LP in the neonatal period, analysing the equipment and analgesia used to perform the procedure. To do so, we developed a self-report questionnaire to be filled out anonymously by paediatricians and residents in paediatrics that worked in Spanish hospitals between May and July 2019. We distributed the questionnaire by email through the Sociedad Española de Neonatología (Spanish Society of Neonatology, SEN) and the Segurneo-SEN hospital network. Participation was voluntary.
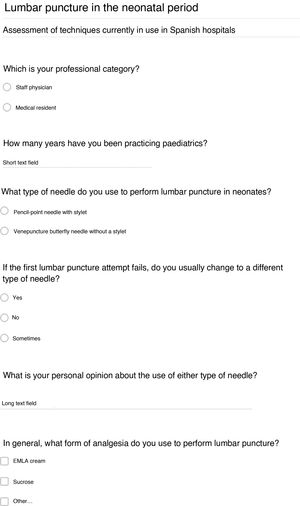
The questionnaire included 6 items (Fig. 1). The first 2 collected data regarding professional experience (professional category and years of experience). The following 2 items concerned the type of needle used to perform LP in neonates, which was used as the first choice and whether a different type of needle was used in case the first attempt failed. The fifth item evaluated the personal opinion of the provider regarding the use of either type of needle, and an open text field was provided for the answer. The sixth item asked about the use of analgesia for performance of LP.
The statistical analysis was performed with the software SPSS version 24.0. We summarised qualitative data as absolute frequency and percentage distributions and quantitative variables as mean and standard deviation (SD) in case of a normal distribution and otherwise as median and interquartile range. We compared the LP technique based on the number of years of professional experience, and considered p-values of less than 0.05 statistically significant. We assessed the association between continuous quantitative and qualitative variables by means of the Student t test for independent samples. Prior to this comparison, we used the Levene test to assess the homogeneity of variance in case of a normal distribution, and otherwise the non-parametric Mann–Whitney U test. To assess the association between qualitative variables, we used the χ2 test or the Fisher exact test as applicable.
ResultsWe received responses to the questionnaire from 301 clinicians in different Spanish hospitals (Table 1). Of this total, 2 (0.7%) did not respond to the item asking about their position in the hospital, 290 (96.3%) were paediatricians and 9 (3%) were medical residents in paediatrics and its subspecialities. There were no clinicians from other specialities. The years of experience of respondents did not follow a normal distribution, with a median experience of 14 years and an interquartile range of 8–20 years.
Overall results.
| N = 301 (100%) | |
|---|---|
| Years of experience, median (IQR) | 14 (8−20) |
| Doctor | 14.5 (9−20) |
| Medical resident | 3.0 (1.5−3.5) |
| Professional category | n = 299 |
| Doctor | 290 (96.3%) |
| Medical resident | 9 (3.0%) |
| Needle used | n = 301 |
| Butterfly | 31 (10.3%) |
| Atraumatic | 270 (89.7%) |
| Change to different needle | n = 301 |
| No | 204 (67.8%) |
| Yes | 43 (14.3%) |
| Sometimes | 54 (17.9%) |
| Personal opinion of practitioner | n = 143 |
| Only used atraumatic needles | 59 (41.3%) |
| Easier with butterfly needle | 46 (32.2%) |
| Higher success rate with butterfly needle | 11 (7.7%) |
| Depended on size of newborn | 15 (10.5%) |
| No preference for either needle type | 12 (8.4%) |
| Analgesia during procedure | n = 301 |
| No | 3 (1%) |
| Yes | 297 (99%) |
| Sucrose | n = 301 |
| No | 56 (18.6%) |
| Yes | 245 (81.4%) |
| Other nonpharmacological measures | n = 301 |
| No | 280 (93%) |
| Yes | 21 (7%) |
| Topical anaesthetic cream | n = 301 |
| No | 32 (10.6%) |
| Yes | 269 (89.4%) |
| Systemic drugs | n = 301 |
| No | 289 (96%) |
| Yes | 12 (4%) |
IQR, interquartile range.
The type of needle used most frequently for performance of LP in the neonatal period was the atraumatic pencil-point needle with a stylet (89.7%). If the first attempt of LP failed or the sample had traces of blood, 32.2% of respondents changed to a different type of needle (14.3% routinely, and 17.9% sometimes).
When it came to the text field provided for the open-ended question on the subjective opinion of the clinician regarding the use of either type of needle, we obtained 143 answers that could be grouped as follows:
- •
59 respondents (41.3%) reported only using atraumatic needles with stylets.
- •
46 respondents (32.2%) stated that the procedure was easier to perform with a butterfly needle, arguing that this type of needle allows more control during its handling and that it was easier to identify the subarachnoid space during needle insertion.
- •
11 respondents (7.7%) reported that the probability of LP failure or obtaining a sample contaminated with blood was lower with the butterfly needle.
- •
15 respondents (10.5%) chose the type of needle based on the size of the neonate, using a butterfly needle without a stylet in low-weight and preterm infants.
- •
12 respondents (8.4%) did not have a preference for either type of needle for performance of the procedure.
Concerning the type of anaesthesia used to perform LP in neonates, 99% of clinicians used some form of analgesia. The most widely used measures were the following:
- •
Topical anaesthetic cream (lidocaine with or without prilocaine): 269 (89.4%).
- •
Sucrose: 245 (81.4%).
- •
Other nonpharmacological interventions (suction, comfort measures, breastfeeding): 21 (7%).
- •
Intravenous systemic drugs (fentanyl, remifentanil, morphine, midazolam, nitrous oxide, paracetamol): 12 (4%).
Clinicians that used butterfly needles had a mean of 17.7 years of professional experience (SD, ±10.26), compared to 14.8 years (SD, 8.51) for clinicians that used atraumatic needles, although the difference was not statistically significant (P = .08).
Clinicians that used nonpharmacological pain management measures during the procedure had a mean of 14.8 years of professional experience (SD, 8.41), while clinicians that did not use these measures had been practicing for a mean of 16.3 years (SD, 9.59), a difference that was not statistically significant (P = .28).
Clinicians that used intravenous analgesics for pain management during the procedure had a mean of 16.5 years (SD, 6.58) of professional experience, compared to 15.8 years (SD, 8.78) in the group that did not use them, a difference that was not statistically significant (P = .55).
We established cut-off points to define 3 professional experience categories (10, 20 and 30 years) and compared the type of needle, nonpharmacological pain management measures and intravenous sedation and analgesia used by each group of clinicians (Tables 2–4). We did not find statistically significant differences, although clinicians with more than 30 years’ experience tended to use butterfly needles more frequently (P = .069) and nonpharmacological pain management measures less frequently (P = .085).
Type of needle used for performance of lumbar puncture in neonatal patients by years of professional experience.
| Years of experience | Type of needle | P | |
|---|---|---|---|
| Atraumatic | Butterfly | ||
| ≤10 years of experience (n = 109) | 99 (90.8%) | 10 (9.2%) | .629 |
| >10 years of experience (n = 192) | 171 (89.1%) | 21 (10.9%) | |
| ≤20 years of experience (n = 229) | 208 (90.8%) | 21 (9.2%) | .251 |
| >20 years of experience (n = 72) | 62 (86.1%) | 10 (13.9%) | |
| ≤30 years of experience (n = 285) | 258 (90.5%) | 27 (9.5%) | .069 |
| >30 years of experience (n = 16) | 12 (75%) | 4 (25%) | |
Use of nonpharmacological pain management measures during lumbar puncture in neonatal patients by years of professional experience.
| Years of experience | Nonpharmacological measures | P | |
|---|---|---|---|
| Yes | No | ||
| ≤10 years of experience (n = 109) | 90 (82.6%) | 19 (17.4%) | .903 |
| >10 years of experience (n = 189) | 155 (82.0%) | 34 (18.0%) | |
| ≤20 years of experience (n = 228) | 192 (82.4%) | 36 (15.8%) | .104 |
| >20 years of experience (n = 70) | 53 (75.7%) | 17 (24.3%) | |
| ≤30 years of experience (n = 282) | 235 (83.3%) | 47 (16.7%) | .085 |
| > 0 years of experience (n = 16) | 10 (62.5%) | 6 (37.5%) |
Use of pharmacological sedation and analgesia for pain management during lumbar puncture in neonatal patients by years of professional experience.
| Years of experience | IV sedation/analgesia | P | |
|---|---|---|---|
| Yes | No | ||
| ≤10 years of experience (n = 109) | 3 (2.8%) | 106 (97.2%) | .546 |
| >10 years of experience (n = 189) | 9 (4.8%) | 180 (95.2%) | |
| ≤20 years of experience (n = 228) | 9 (3.9%) | 219 (96.1%) | 1.000 |
| >20 years of experience (n = 70) | 3 (4.3%) | 67 (95.7%) | |
| ≤30 years of experience (n = 282) | 12 (4.3%) | 270 (95.7%) | 1.000 |
| >30 years of experience (n = 16) | 0 (0%) | 16 (100%) | |
The complexity of neonatal units and the characteristics of their patients are factors that contribute to a greater concern about patient safety in clinicians working in these settings. In recent years, there have been significant advances in the prevention of medical errors and the control of nosocomial infections.32,33 However, adverse events associated with medical procedures and techniques used in neonatal units should be considered just as important, as they may have serious effects in this group of highly vulnerable patients.34
Lumbar puncture is one of the procedures used most frequently in neonatology for diagnosis and treatment purposes. At present, most clinical guidelines discourage the use of venepuncture needles in LP,13 yet their use has been widespread in neonatal units until a few years ago.12,13 As our data show, and compared to the results of the systematic review of Spanish studies published in 2012, in recent years there has been a significant reduction in the use of venepuncture needles as the first choice for performance of LP in neonates in Spanish hospitals (40% vs 10.3%).13 However, the significant proportion of clinicians that still use butterfly needles as an alternative when the first attempt of PL fails (32.2%) is concerning. A possible explanation of this practice is that some clinicians were accustomed to using butterfly needles during their medical training, when the use of needles with a stylet was not yet widespread. Some paediatricians reported feeling that they had greater control with butterfly needles when performing LP. Our study showed that practitioners that had more years of professional experience tended to use butterfly needles more frequently, probably because they were more skilled in the use of this type of needle, although the difference was not statistically significant.
As for pain management, it has now become a crucial element in neonatal care, as evidence has emerged that insufficient pain management during critical stages of neuronal maturation can have important physiological repercussions and cause neurodevelopmental sequelae.35–37 The review published in the United States in 2004 showed that 2/3 of physicians in the Section on Pediatric Emergency Medicine of the American Academy of Pediatrics did not use analgesia routinely when performing LP in newborn infants.12 Our study shows that nearly all surveyed practitioners (99%) used some form of analgesia to manage pain during LP. The most experienced clinicians tended to use nonpharmacological pain management measures less frequently, although this difference was not statistically significant. Anaesthetic creams and sucrose were the most widely used measures, in adherence with most current clinical guidelines on the prevention and management of pain in neonates.24–26 It is worth noting that only 7% of respondents used 2 or more nonpharmacological measures in combination, a strategy that is more effective for pain management than using a single measure in isolation.38 In any case, nonpharmacological measures may not be sufficient for an invasive, stressful and painful procedure like LP. In recent years, several studies in the fields of paediatric anaesthesia and oncology have supported the use of intravenous analgesia and anaesthesia for performance of LP.28–31 Some guidelines suggest the use of systemic sedation and analgesia for performance of LP in neonates, especially those who are mechanically ventilated.16,39 In our survey, only 4% of clinicians used anything other than topical sedatives or analgesics, in most cases opiates. One possible reason is the concern regarding the potential adverse effects of using systemic sedatives or analgesics in the neonatal period. Thus, we think that these drugs may not be considered safe enough for use in neonatal care.
One of the limitations of the study is that we did not know which hospital and autonomous community respondents worked in, as we did not collect data on these aspects through the questionnaire. Although the channels used to distribute the questionnaire were of national scope, we are not able to determine whether the sample is representative of clinical practice nationwide. Another limitation is that the vast majority of respondents were licensed paediatricians (96.3%), and only 3% medical residents in paediatrics. This uneven distribution may be due to the channels we used to disseminate the questionnaire (Segurneo-SEN Hospital Network and the Sociedad Española de Neonatología), institutions whose members have usually completed their training and are already licensed to practice.
Another limitation of our study was that we did not ask about the existence of specific protocols for performance of LP and the use of sedation and analgesia specifically for this procedure in the unit. It would have been interesting to analyse this aspect to determine whether the supplies used in LP or the widespread use of specific pain management measures could be influenced by the implementation of such protocols.
The findings of our study reflect the knowledge of Spanish paediatric practitioners regarding the correct technique for performance of LP in the neonatal period and suggest that they are increasingly aware of the potential complications of the procedure and the need to manage the resulting pain in newborn infants. Still, we found opportunities for improvement in completely abandoning the use of butterfly needles for this procedure and optimization of analgesic measures. The use of written protocols and specific checklists for performance of each technique, optimal pain management with appropriate use of sedation and analgesia and patient monitoring, along with simulation-based practical training, constitute the most comprehensive approach to improve the safety of this and other procedures in neonatal clinical practice.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank every health professional that has contributed to the study by completing and/or disseminating the questionnaire.
Please cite this article as: Jimeno Ruiz S, Riaza Gómez M, Cárdenas Rebollo JM, López-Escobar A. Material y sedoanalgesia en el procedimiento de punción lumbar neonatal. An Pediatr (Barc). 2020. https://doi.org/10.1016/j.anpedi.2020.07.026