Developmental dysplasia of the hip is a common cause of disability among children. Early detection leads to better prognosis. There are some risk factors that increase the possibility of developing a dysplasia. But not every child with developmental dysplasia has them. This means that physical examination is still very useful to detect them. However, based on clinical findings, the amount of requested ultrasound seems higher than it would be necessary.
MethodsRetrospective cohort study of infants born in a single tertiary care centre. Babies in which hip ultrasound was performed were included. During the period of study, patients with diagnosis of developmental hip dysplasia were also included, as well as the amount of ultrasounds requested during this period, and their efficiency.
ResultsOut of the 456 newborns included, 530 hip ultrasounds were performed. Just 3 of the total 12 dysplasias had risk factors. The others were diagnosed through clinical examination.
ConclusionsScreening protocols are useful to detect hip dysplasia but clinical examination is very important to detect those cases without risk factors. However, the number of tests is higher than expected according to the diagnosed dysplasias.
La displasia del desarrollo de la cadera se trata de una patología relativamente frecuente y es una causa importante de discapacidad si no se trata de la forma adecuada. Existen una serie de factores de riesgo que aumentan la probabilidad de presentar una displasia de caderas, pero la mayoría de los afectados no los presentan. Por ello, la exploración física es fundamental para su diagnóstico. No obstante, el número de ecografías solicitadas parece ser muy superior al que sería necesario según los hallazgos clínicos.
Material y métodosEstudio observacional descriptivo retrospectivo de los recién nacidos pertenecientes al área de referencia de un hospital terciario. Se recogieron las ecografías de caderas realizadas en nuestro centro durante el periodo de estudio, así como los diagnósticos de displasia durante dicho periodo para comprobar la frecuencia de presentación de los factores de riesgo y los hallazgos clínicos, además del número de ecografías solicitadas en este periodo y su rendimiento.
ResultadosSe incluyeron un total de 456 recién nacidos a los que se realizaron un total de 530 ecografías de caderas. Tres de las 12 displasias detectadas en este tiempo presentaban factores de riesgo, el resto de los pacientes fue diagnosticado por la clínica.
ConclusionesLos protocolos de screening son implementados de forma adecuada en nuestro medio, aunque sin la exploración física detallada no sería posible la detección precoz de la dysplasia, evitando con ello secuelas a largo plazo. No obstante, el número de ecografías de caderas solicitadas es muy superior al que se esperaría, dado el bajo porcentaje de displasias halladas.
Developmental dysplasia of the hip (DDH) is a relatively frequent condition that may cause significant disability if it is not treated adequately. The incidence varies between published case series, and is estimated at 1–10 cases per 1000 live births. These differences stem from the inclusion criteria applied in different studies, the age of patients at the time of assessment and additional genetic factors, such as racial differences.1
The term DDH encompasses different conditions ranging from instability, luxation or subluxation to anomalies that can only be detected radiographically. In addition, there are different types of dysplasia based on the aetiology and timing of onset. Thus, DDH is classified into: teratologic hip dysplasia, associated with underlying disease in the patient and manifesting prenatally, and typical dysplasia, which may be congenital or have onset during childhood in patients with no underlying disease. In general, hip dysplasia develops in otherwise healthy infants. Many cases of hip dysplasia resolve without intervention within a few months, so it is important not to overtreat patients, but rather observe them closely. However, 90% of patients that do not receive adequate treatment present moderate to severe articular disease in adulthood, in some cases requiring hip replacement at an early age. This generates substantial health care costs in addition to causing disability in patients with a deleterious impact on the social environment.2–5
The aetiology of DDH is multifactorial and includes genetic and environmental factors. There are also known risk factors for its development, including female sex, breech presentation and positive family history of DDH. It is estimated that hip dysplasia is 8 times more frequent in girls. The footling breech position, which may be more likely in case of oligohydramnios or multiple pregnancy, seems to put pressure at the the hip level due to the abnormal foetal position. When it comes to the positive family history, the literature describes a 6% increase in risk in case a previous child had hip dysplasia, a 12% increase in case a parent had dysplasia and an increase of up to 36% in case both a parent and a sibling have a history of hip dysplasia. These are known as the classic risk factors. Thus, when 2 or more of these risk factors are present, an ultrasound examination is recommended for screening of DDH at 4–8 weeks post birth if the newborn infant appears normal in the physical examination. Needless to say, if the patient exhibits any compatible manifestations, management of DDH must start immediately.1,6–9
At any rate, it is estimated that these risk factors are only found in 10%–27% of patients with hip dysplasia, and therefore the physical examination continues to be key in its detection. There is no pathognomonic feature that could be detected in the physical examination, but adequate examinations performed at different time points continue to be of the essence. Given the developmental nature of dysplasia, different manifestations may emerge from month to month. Thus, in the newborn infant, the Ortolani test and Barlow manoeuvre and the development of asymmetric gluteus folds or an apparent limb-length inequality are signs that should alert clinicians to the potential presence of dysplasia. Later on, limited hip abduction or the Galeazzi sign help make the diagnosis.6,8 We ought to underscore that gluteal fold asymmetry or hip clicks are of little value for diagnosis of DDH and are a frequent reason for referral to hospital and ordering ultrasound examinations.6 However, development of these signs indicates re-evaluation of these patients, as their persistence through time may be an indirect sign of dysplasia.10
The gold standard for diagnosis is a hip ultrasound in the first months of life, a non-invasive technique that does not involve irradiation. In some countries, this test is performed routinely in all newborn infants, but its diagnostic yield remains unclear. There is observer-dependent variability in this test, and detection of DDH requires performance by an experienced sonographer. Also, the importance of sonographic findings that will never lead to dysplasia may also be overestimated (high frequency of false positives), which increases the health care costs generated by routine performance of hip ultrasound examination due to the additional tests performed in case of a false positive.
In Spain, current recommendations include screening of patients with 2 or more of the classic risk factors described above and an exhaustive physical examination for detection of dysplasia in patients without risk factors.3,6,7
Our hospital implements the national protocol based on the physical examination of the newborn in the first hours of life, with a positive result of screening defined as a positive Ortolani and/or Barlow test.7 In addition, performance of a hip ultrasound examination is indicated in patients with 2 or more risk factors based on the Previnfad guidelines (female sex, positive family history of DDH and/or breech presentation).
All the ultrasound examinations ordered in our catchment area are performed in the department of radiology of our hospital, so we were able to determine the number of orders for hip ultrasound examinations and, in most cases, the reason for the request and/or referral.
Material and methodsWe conducted a retrospective observational and descriptive study of neonates in the catchment area of our hospital, a level IIIB facility, between January 2017 and December 2018.
We collected data on the hip ultrasound examinations performed in our hospital between January 2017 and May 2019 ordered from the hospital as well as from primary care centres in the same catchment area. We extended the period of data collection from health records through May 2019 to include patients born at the end of the year that underwent hip ultrasound examinations and/or were in follow-up as a result of this test. This prevented the loss of data for patients born in November and December 2018.
The case definition of hip dysplasia was diagnosis of DDH by a traumatologist, regardless of the management required by the patient.
In addition to collecting data on risk factors for DDH described above, we collected data on variables such as gestational age, sex, foetal presentation, type of delivery and birth weight from the health records of the patients.
We excluded patients with skeletal malformations, congenital malformations or other diseases associated with an increased incidence of hip dysplasia.
We requested information on the cost of hip ultrasound examinations in our health area for years 2017 and 2018, and found a mean cost of approximately 22 euro. Reviewing data for other hospitals and health areas in Spain that is freely accessed online, we found that the costs of ultrasound can be as high as 40 euro per examination. We also requested data for our health area on the cost of visits at the primary care level, with a mean cost of 16 euro per visit, and visits to specialists in paediatrics or traumatology, with costs that ranged from 50 to 100 euro per visit.
The aim of our study was to analyse the reasons for requesting hip ultrasound examinations, determine the incidence of hip dysplasia in otherwise healthy infants in our region and assess whether screening protocols are implemented correctly.
The Clinical Research Ethics Committee of our hospital approved the review of health records and the data collection protocol.
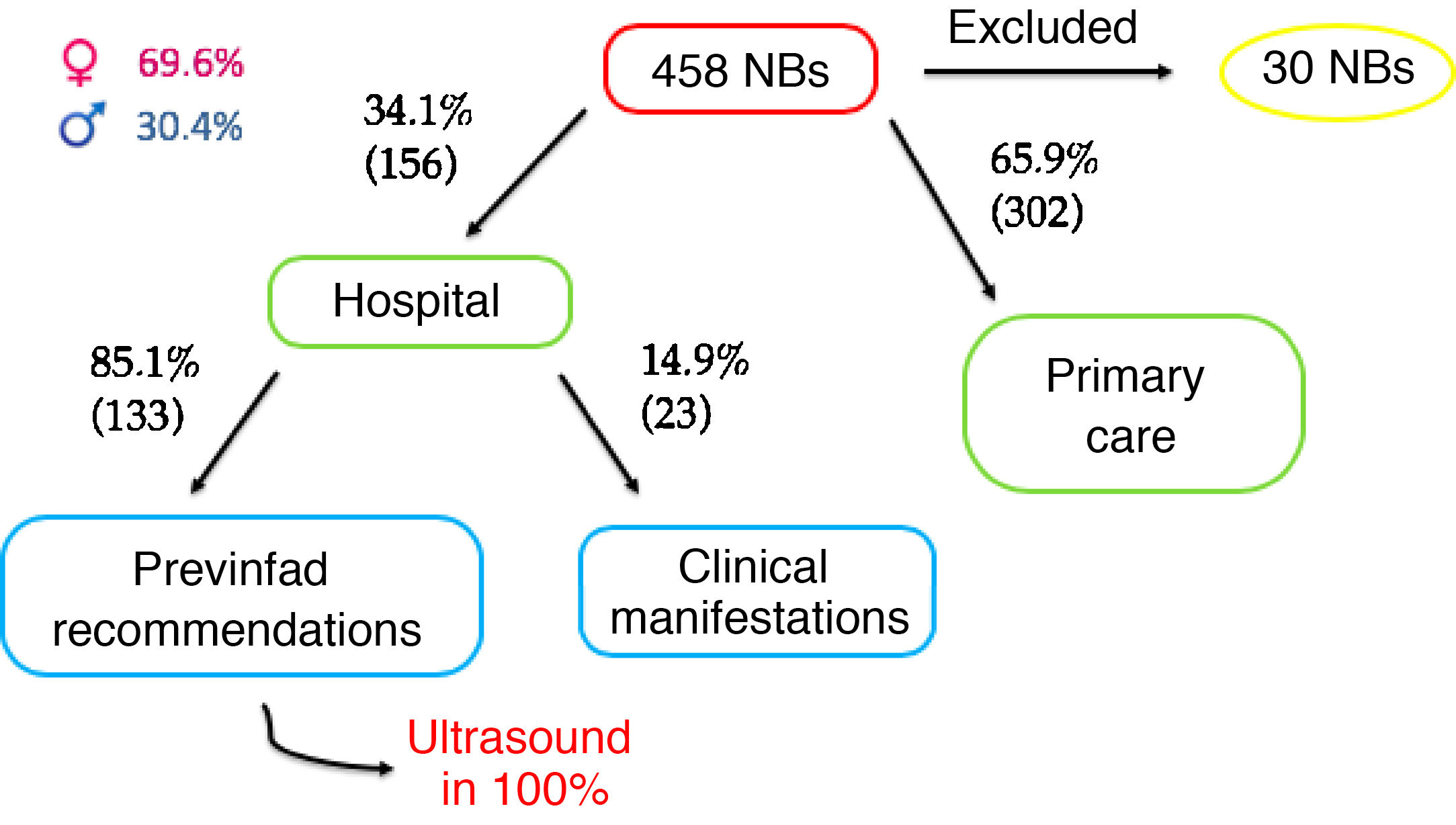
ResultsA total of 456 neonates underwent at least one hip ultrasound examination in the period under study. We excluded 30 because they either met an exclusion criterion or the reason for ordering the ultrasound was not documented. In any case, we reviewed the health records of the excluded patients and found that none received a diagnosis of hip dysplasia.
The total number of hip ultrasound examinations performed in the remaining patients for the indication of interest was 530. Seventy-seven children underwent 2 ultrasound examinations, ten children underwent 3 and one child, 6; 10 children received a diagnosis of hip dysplasia, and 30 children that had at least 1 follow-up ultrasound had risk factors for dysplasia.
Of the total orders, 69.6% were made in female patients, and the mean gestational age of the patients was 39.1 weeks (standard deviation, ±1.98). Also, 34.1% of the ultrasound examinations were ordered at the hospital level, of which 85.1% were indicated based on the Previnfad recommendations. None of the patients that met the criteria of the Previnfad guidelines was discharged from hospital without an order for a hip ultrasound by 6 weeks post birth, which indicates 100% adherence on this aspect of care (Fig. 1).
Of all hip ultrasound examinations performed due to patients meeting the Previnfad criteria, 23.7% corresponded to girls with a history of breech presentation, 5.7% to girls with a positive family history, 0.2% to boys with a breech presentation and a positive family history and 0.2% to girls with all 3 risk factors. The remaining ultrasound examinations were ordered, in decreasing frequency, due to the presence of a hip click (35.3%), asymmetric gluteal folds (18.6%), positive Ortolani and/or Barlow test in the physical examination (3.7%) and the combination of a hip click and asymmetric folds (1.09%). Of all the ultrasound examinations performed to evaluate a hip click, 47.9% were ordered from primary care.
All patients in which there was a high clinical suspicion or with ultrasound findings compatible with DDH were referred for evaluation by a traumatologist, who was ultimately responsible for confirming or ruling out the diagnosis.
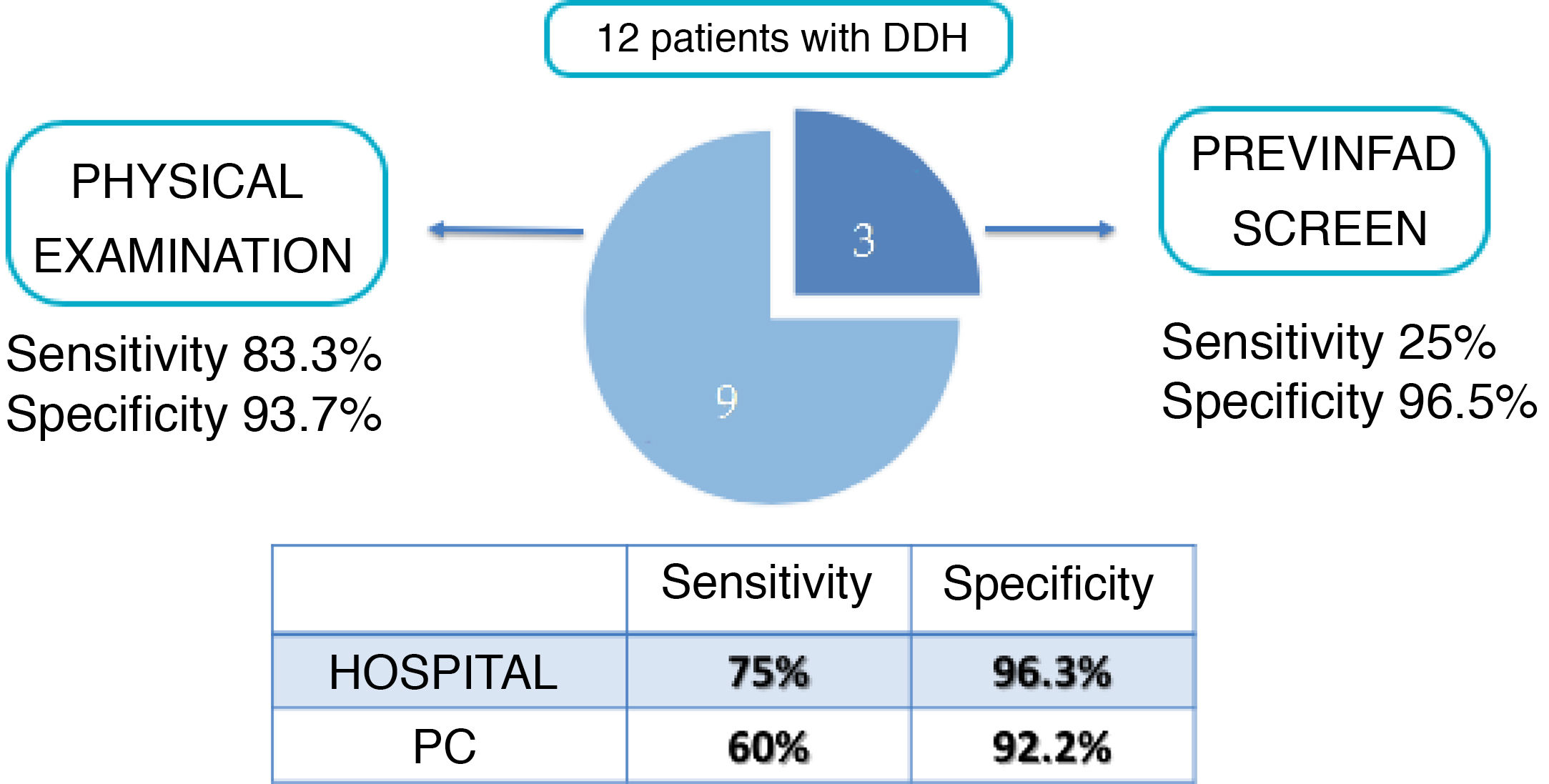
In the period under study, 15 children received a diagnosis of DDH, of which we excluded 3 because they had other skeletal anomalies or diseases associated with the development of hip dysplasia. Of these 12 cases, 3 were detected through and the remaining 9 were diagnosed due to the presence of clinical manifestations (Sen, 83.3%; Spe, 93.7%). These manifestations were gluteal fold asymmetry in 3 cases, a hip click in 1 and a positive Ortolani and/or Barlow test in 5. We ought to highlight, as we consider it relevant, that 4 of the 5 children with a positive Ortolani and/or Barlow test, which was the reason for performing the hip ultrasound examination, also had risk factors for DDH. Thus, if dysplasia had not been detected in the physical examination of these patients, it would have been detected by the ultrasound performed at age 4–6 weeks, although the diagnosis would have been delayed and therefore the risk of sequelae would have been greater. Seventy-five percent of dysplasia cases were diagnosed in the hospital, and only one was diagnosed after a hip click prompted ordering of the hip ultrasound examination from primary care (Fig. 2).
Of the total hip ultrasound orders, 29% were indicated based on the screening criteria. This means that 71% of ultrasound examinations were ordered on account of clinical manifestations, and of those cases, only 2.8% turned out to be cases of DDH.
All cases were diagnosed in girls, a difference that was statistically significant (P = .004).
DiscussionOur hospital does not have a universal screening protocol, in adherence with the current Previnfad guidelines in Spain.
The literature regarding screening is contradictory, with some authors recommending universal screening and others selective screening in patients with risk factors or compatible manifestations. Proponents of either approach support their position on different arguments. Proponents of universal screening argue that it detects all cases of developmental dysplasia present at birth and therefore early initiation of treatment, which reduces the risk of long-term sequelae. In contrast, those who advocate for selective screening argue that routine screening tends to overestimate the importance of abnormalities that have favourable outcomes without intervention, exposing these patients to unnecessary interventions and procedures. It is estimated that nearly 90% of infants that exhibit hip instability at birth have good outcomes within 8 weeks and that up to 96% of abnormal sonographic findings resolve spontaneously in the first month and a half. Therefore, performance of ultrasound at birth can help detect true cases of dysplasia early, but it also increases the risk of unnecessary treatments or tests in patients that would have had favourable outcomes without them.11
On the other hand, those who propose screening in patients with risk factors highlight the importance of repeated physical examinations for diagnosis. One of the reasons they emphasise physical examinations is that hip dysplasia may develop after the neonatal period. Therefore, in populations where universal screening is performed at birth, cases that manifest in the neonatal period are identified, but cases that develop later in the first year post birth may go undetected if attention is not paid to potential clinical manifestations. Thus, there is a risk of delayed diagnosis with both approaches.12,13 This is why it seems reasonable to emphasize the need to screen patients with risk factors but also to performed appropriate and repeated physical examinations.
Our hospital, as we described above, applies the Previnfad recommendations for performance of hip ultrasound based on the presence of risk factors and the examination of newborn infants in the first 48–72 h post birth. The subsequent follow-up of these patients is conducted at the primary care level.6,7
Based on the findings of our study, the screening of at-risk patients offers a low sensitivity of approximately 25%, but it is important to interpret these results in context and considering that they are consistent with the previous literature. First of all, the low number of dysplasia cases identified in the population, to which we must add an even smaller number of cases detected through screening. Second, the low sensitivity of this approach is due to screening not being universal, but performed exclusively in patients with risk factors, so that some cases in the population go undetected. Therefore, repeated physical examinations in the first year of life are essential for detection of dysplasia. We also found a high specificity, another aspect that supports screening of at-risk patients, as a normal ultrasound in infants with risk factors practically rules out the presence of hip dysplasia at birth. However, due to the risk of dysplasia with a later onset, performance of ultrasound in the neonatal period does not eliminate the need for serial physical examinations in the first year of life. At any rate, our data corroborated what has been previously described, that only 10%–27% of patients with dysplasia present risk factors.6
We verified that screening of infants with risk factors in our catchment area was performed as indicated and in 100% of infants that required it. Whether it should be recommended or not, scientific societies and cost-effectiveness analysis support its performance despite its low diagnostic yield on account of the high cost associated with delayed initiation of treatment of dysplasia compared to the cost of one ultrasound examination.14 Nevertheless, we must qualify this recommendation, as performance of that one ultrasound in the absence of compatible manifestations should not be performed before 6 weeks post birth to minimise potential abnormal findings associated with immaturity or unlikely to progress to hip dysplasia, thereby avoiding both overdiagnosis and overtreatment.13,15 In our study we did not collect data on the precise timing of the ultrasound examination, but on whether it was performed in the timeframe recommended by the Previnfad guidelines, between 4 and 8 weeks post birth.
A little less than one third of the performed ultrasound examinations were indicated based on the screening criteria, which means that a large number of ultrasound scans were ordered based on the presence of clinical manifestations, with a detection rate of less than 2%.
In our study, 30 children with risk factors were evaluated with ultrasound more than once, and 7 received a final diagnosis of dysplasia, but in the remaining 23 cases the sonographic evaluation was a health care expenditure that ultimately proved unnecessary. The total cost of all performed hip ultrasound scans added up to nearly 12 000 euro. In these 2 years, the cost of screening amounted to approximately 3000 euro based solely on the performance of hip ultrasound scans. If we added the anamnesis and physical examinations performed in in-person primary care and speciality clinic visits, the full cost would amount to a few more thousand euro. Still, the objective of our study was not to assess the costs associated with screening or the indication for performance of hip ultrasound based on clinical features. We only sought to reflect on whether the indications for diagnostic ultrasound could be improved in order to reduce costs.
In our sample, every patient with a diagnosis of dysplasia that required some form of intervention was female. The literature describes female sex in association with a higher probability of developing hip dysplasia, although it is not a necessary condition. The fact that only girls received a diagnosis of DDH in our study is probably due to the small sample size. However, our study did corroborate the higher incidence in female patients.1
When it came to ultrasound examination orders stemming from clinical features, we found that hip clicks were the main reason for ordering the test in patients without risk factors. A study published by Nie et al. in 2017 found that an isolated hip click was not a risk factor for dysplasia. It is usually due to joint hypermobility and can be associated with clicks in the shoulders or knees that are not pathological. The authors also noted that onset or persistence of the click past age 6 weeks is usually associated with other signs, such as limited hip abduction, that have been found to be strongly associated with dysplasia. Therefore, it is important to remember that a hip click in isolation should not be considered an indication for hip ultrasound examination unless it persists past 6 weeks post birth and is associated with another relevant sign or symptom.10,16 The study also reflected the progressive increase of referrals from primary care for assessment of a hip click, reaching up to 70% of the overall referrals due to hip clicks, although in our study primary care referrals amounted to less than 50% of the total.
Reflecting on the findings of our study, it is fair to conclude, first of all, that the number of ultrasound examinations that are being ordered commonly exceed the number of examinations that are actually indicated. Thus, among other measures for improvement, it seems necessary to create resources to support the appropriate interpretation of the clinical signs associated with hip dysplasia. However, attempting to analyse this aspect in our study was challenging because the variability was observer-dependent and test order records do not always include an exhaustive account of the detected signs.
Secondly, in case of a normal physical examination, postponing the hip ultrasound in patients with risk factors to 6–8 weeks post birth could reduce the number of ultrasound examinations that have to be repeated due to detection of nonspecific abnormal features, which are usually signs of immaturity.
Third, adjusting the indications for hip ultrasound would reduce health care costs as well as the number of ensuing medical visits and the anxiety experienced by families.
In conclusion, we recommend not only screening for DDH, but also a periodic review of the clinical criteria used to determine the indication of hip ultrasound examination and performance of repeated physical examinations in the first year of life or even until the child starts walking.9
FundingThis study was not supported by any form of funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Escribano García C, Bachiller Carnicero L, Marín Urueña SI, del Mar Montejo Vicente M, Izquierdo Caballero R, Morales Luengo F, et al. Displasia evolutiva de caderas: más allá del cribado. La exploración, nuestra asignatura pendiente. An Pediatr (Barc). 2021;95:240–245.
Previous presentations: The study was presented at the XXVII Congreso de Neonatología y Medicina Perinatal, October 2–4, 2019, Madrid, Spain, and the XXXII Memorial Guillermo Arce y Ernesto Sánchez-Villares, October 15–16, 2019, Oviedo, Spain.