The number of patients with complex chronic conditions (CCC) has increased in the last 20 years or so. There is limited data as regards the prevalence of CCC in the paediatric population and its impact on hospital admissions. The main objectives of this study are to determine the proportion of CCC in the paediatric hospital population and compare them with other groups of patients admitted (acute and chronic).
Patients and methodsA descriptive, retrospective study was carried out in a tertiary maternity-paediatric hospital (from December 2016 to November 2017). All patients admitted into the Paediatric Department were recruited with a fortnightly frequency. A series of demographic, clinical, and pregnancy data were collected. In order to identify the level of complexity of the patients, the Clinical Risk Group (CRG) was used, with 3 groups being created: acute, chronic, and CCC. Statistics analysis was performed using SPSS v24.
ResultsA total of 1433 patients were included. The proportion of CCC on the Paediatric Ward was 14.4%. The CCC were older patients, mainly admitted due to decompensation or progression of their underlying disease, had a longer admission time, and required support in the Paediatric Intensive Care Unit (PICU) more often than that of the other sub-groups. Just under half (44.7%) of the CCC were carriers of a technological device. Of the total of long stays (>1 month), 71.3% had CCC.
ConclusionsPatients with CCC require long hospital stays, a greater need of intensive care, and use of technology. New approaches to treatment and follow-up need to be established. They should be cost-effective, and at the same time decrease the impact of the disease on the children and their family.
En las últimas décadas se ha incrementado el número de pacientes crónicos complejos (PCC). Existen pocos datos referentes a la prevalencia de PCC en población pediátrica y su impacto en los ingresos hospitalarios. Los objetivos principales de este trabajo son determinar en nuestro medio la proporción de PCC en hospitalización pediátrica y compararlos con otros grupos de pacientes ingresados (agudos y crónicos).
Pacientes y métodosEstudio descriptivo retrospectivo realizado en un hospital materno-infantil terciario (de diciembre 2016 a noviembre 2017). Se reclutaron a todos los pacientes ingresados en el servicio de Pediatría con una periodicidad quincenal. Se recogieron una serie de variables demográficas, clínicas y de gestión. Para identificar el grado de complejidad de los pacientes se utilizó el sistema de clasificación Clinical Risk Group (CRG) y se crearon 3 grupos: agudos, crónicos y PCC. Para el análisis estadístico se usó SPSS v24.
ResultadosSe incluyeron 1.433 pacientes. La proporción de PCC en planta de Pediatría fue del 14,4%. Los PCC fueron pacientes de mayor edad, ingresaron principalmente por descompensación o progresión de su enfermedad de base, estuvieron ingresados más tiempo y precisaron soporte en la Unidad de Cuidados Intensivos Pediátricos (UCIP) con mayor frecuencia que los otros subgupos. Un 44,7% de los PCC era portador de dispositivos tecnológicos. Del total de largas estancias (>1 mes), el 71,3% fue de PCC.
ConclusionesLos PCC requieren de estancias hospitalarias largas, mayor necesidad de cuidados intensivos y uso de tecnología. Es necesario plantear nuevos enfoques de tratamiento y seguimiento que sean costo-eficientes a la vez que disminuyan el impacto de la enfermedad en el niño y su familia.
In recent decades, thanks to improvements in medical and surgical care and technological advances, survival has improved for many life-threatening diseases of childhood. As a result, there has been an increase in the number of children with chronic diseases, which are frequently associated with disability, medical fragility and complex health care needs.1,2
Children with special health care needs are those that have or are at increased risk for chronic physical, developmental, behavioural or emotional conditions and who require health and related services of a type or amount beyond that required by the general paediatric population.3,4 Within this group, there is a very specific subgroup of paediatric medically complex or complex chronic patients (CCPs). Complex chronic patients are those who have several chronic diseases that result in medical fragility, functional limitations and substantial health care needs.3,5–7
In the United States, CCPs account for 10% of total paediatric hospital admissions and 40%–80% of paediatric hospital charges.8,9 This huge proportion of the health care spending is explained by CCPs requiring hospitalisation and readmission more frequently, longer stays, more technology-assisted care, multiple treatments and follow-up by a larger number of medical specialists.4,8–11 The figure of the CCP is an emerging phenomenon that is very relevant to health care policy. In Spain, it has led to the establishment of specific hospital units that have experienced a growth in activity in recent years.12 Within CCPs, there is a category of patients with extremely severe illness or catastrophic chronic illness, patients with permanent technology dependence (dialysis, ventilation, parenteral nutrition) or very severe disease that dominates the clinical presentation (e.g. vegetative state).13,14 In addition, catastrophic chronic illness is associated with a high morbidity and mortality and severe functional impairment, which has a profound impact on family dynamics.15
Thus, CCPs are a subset of paediatric patients that interact frequently with the health care system, yet we still do not know the relative importance of this group in the overall population of paediatric inpatients in Spain.
The primary objectives of our study were: (1) to determine the proportion of patients with chronic or complex chronic disease in the department of paediatric inpatient care of a hospital in Spain, and (2) to describe the main differences in the clinical characteristics and use of health care resources between patients with acute disease, chronic disease and complex chronic disease. The secondary objectives were to describe the proportion of CCPs with catastrophic illness and the proportion of patients that had prolonged hospital stays per year.
Material and methodsWe conducted a single-centre retrospective and descriptive study. We collected data every 15 days from December 2016 through November 2017 for every patient admitted to the department of paediatric inpatient care of a tertiary care women’s and children’s hospital in Barcelona, the Hospital Sant Joan de Déu. This hospital serves women and children in a catchment area with a population of 964 000 inhabitants as well as paediatric patients who require highly specialised and level III medical care from the entire autonomous community of Catalonia. The department where the study was conducted fits the definition of a paediatric internal medicine inpatient ward by the Sociedad Española de Pediatría Interna Hospitalaria (SEPHO)16 and serves patients aged 0–18 years requiring urgent or elective hospitalisation. It does not admit surgical or oncological patients or patients requiring care in the subspecialities of neurology, nephrology or endocrinology if the reason for admission is to provide specific treatment for a known disease in these subspecialities, although it does admit patients requiring care in these 3 subspecialities if they present with other diseases, such as infection, respiratory illness or symptoms with an elusive diagnosis. We collected data for 3 types of variables: (1) demographic variables: age, immigrant origin (parents born outside the European Union); (2) clinical variables: underlying disease, reason for admission (intercurrent illness, decompensation/progression of underlying disease, or planned admission for performance of diagnostic tests or surgical intervention), use of supportive care devices after discharge (invasive and non-invasive ventilation devices, gastrostomy, long-term intravenous access lines [port-a-cath, Broviac catheter, Hickman catheter], other devices [baclofen pump, cerebrospinal fluid drain, tracheostomy tube, implantable cardioverter-defibrillator…]), number of drugs prescribed at discharge, and (3) management variables: length of stay, need of admission to intensive care unit and number of appointments in specialty clinics scheduled at discharge. We encoded the data and entered them in an electronic database developed specifically for the study.
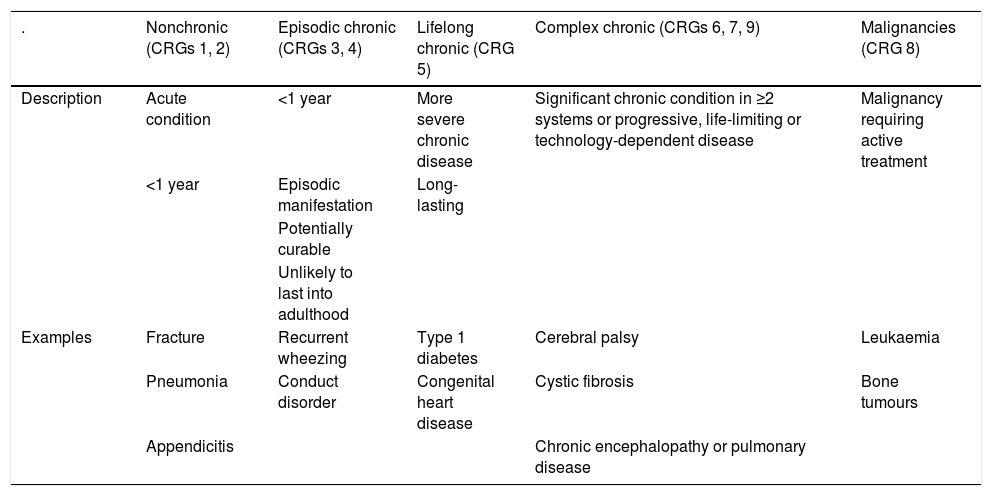
To establish the medical complexity of the patients, we used the Clinical Risk Group (CRG) classification13 (Table 1). This system provides an exhaustive classification into 9 mutually exclusive groups of increasing complexity based on the medical condition of the patient. To assign patients to CRGs, we manually reviewed electronic health records and hospital discharge summaries and used the discharge diagnosis code to define risk. We classified patients in the sample into 3 groups based on the assigned CRG: acute (CRGs 1 and 2), chronic (CRGs 3–5) and complex chronic (CRGs 6, 7 and 9). In the CCP group, we also differentiated the subset of patients with catastrophic complex chronic (CCC) illness, corresponding to CRG 9, patients with very severe chronic disease or technology-dependent in the long term. We did not include patients in CRG 8 in the study, as these are oncological patients with clinical characteristics that differ significantly from the rest of paediatric patients and that are not hospitalised in the paediatric inpatient ward in the Hospital Sant Joan de Déu.
Clinical Risk Group classification.10
| . | Nonchronic (CRGs 1, 2) | Episodic chronic (CRGs 3, 4) | Lifelong chronic (CRG 5) | Complex chronic (CRGs 6, 7, 9) | Malignancies (CRG 8) |
|---|---|---|---|---|---|
| Description | Acute condition | <1 year | More severe chronic disease | Significant chronic condition in ≥2 systems or progressive, life-limiting or technology-dependent disease | Malignancy requiring active treatment |
| <1 year | Episodic manifestation | Long-lasting | |||
| Potentially curable | |||||
| Unlikely to last into adulthood | |||||
| Examples | Fracture | Recurrent wheezing | Type 1 diabetes | Cerebral palsy | Leukaemia |
| Pneumonia | Conduct disorder | Congenital heart disease | Cystic fibrosis | Bone tumours | |
| Appendicitis | Chronic encephalopathy or pulmonary disease |
CRG, clinical risk group.
To calculate the proportions of acute, chronic and complex chronic patients in each 15-day period, we only took into account the patients newly admitted in that period. We excluded patients that were readmitted as well as patients with stays that spanned more than one 15-day period from the final sample.
Since there is no international consensus on the definition of prolonged length of stay, we chose to define it as hospitalisation lasting more than 1 month. To calculate the number of prolonged stays that occurred in a year, we did take into account all the admissions and readmissions of paediatric patients to ensure that the analysis included every stay in the 12-month period.
The statistical analysis was performed with the software SPSS version 24.0. We have summarised quantitative data as mean and standard deviation (SD) in case of a normal distribution and otherwise as median and interquartile range (IQR), and qualitative data as percentages. We compared variables using the χ2 test and analysis of variance. We considered p-values of less than 0.05 statistically significant.
The study was approved by the Clinical Research Ethics Committee of the hospital.
ResultsProportion of patients with chronic disease and complex chronic diseaseIn the period under study (12 months) we collected data for 1515 hospitalisation events, which corresponded to 1433 patients, as some patients had stays that extended past a single timepoint or experienced readmissions.
Based on the established definitions, the reason for admission was acute disease in 57.1% of cases (n = 818) and chronic disease in 28.5% (n = 408). We identified 207 CCPs, who amounted to 14.4% of total paediatric inpatients.
Patient characteristicsThe mean age of the patients included in the study was 3.6 years (SD, 4.6; range, 0–19.6). The median length of stay was 5 days (IQR, 3.0–8.0; range, 0–767). The most frequent reason for admission was respiratory disease (50.4%; n = 722), followed by infectious disease (27.4%; n = 392) and gastrointestinal disease (8%; n = 114). Nearly all patients (97.9%; n = 1403) were admitted through the emergency department of the Hospital Sant Joan de Déu. Most patients were admitted for management of acute intercurrent diseases (72.8%; n = 1043). Another 25.4% (n = 364) were admitted due to decompensation or progression of an underlying disease, while 1.7% (n = 25) had planned admissions. Only 7.3% of the patients (n = 104) used medical devices: 66 had a long-term nasogastric or gastrostomy tube, 33 required mechanical ventilation, 5 carried a central catheter and 19 used other medical devices (several patients used more than 1 device). Out of all patients, 21.6% (n = 309) were of immigrant origin. A total of 10.5% (n = 150) required admission to the paediatric intensive care unit (PICU) during the study period.
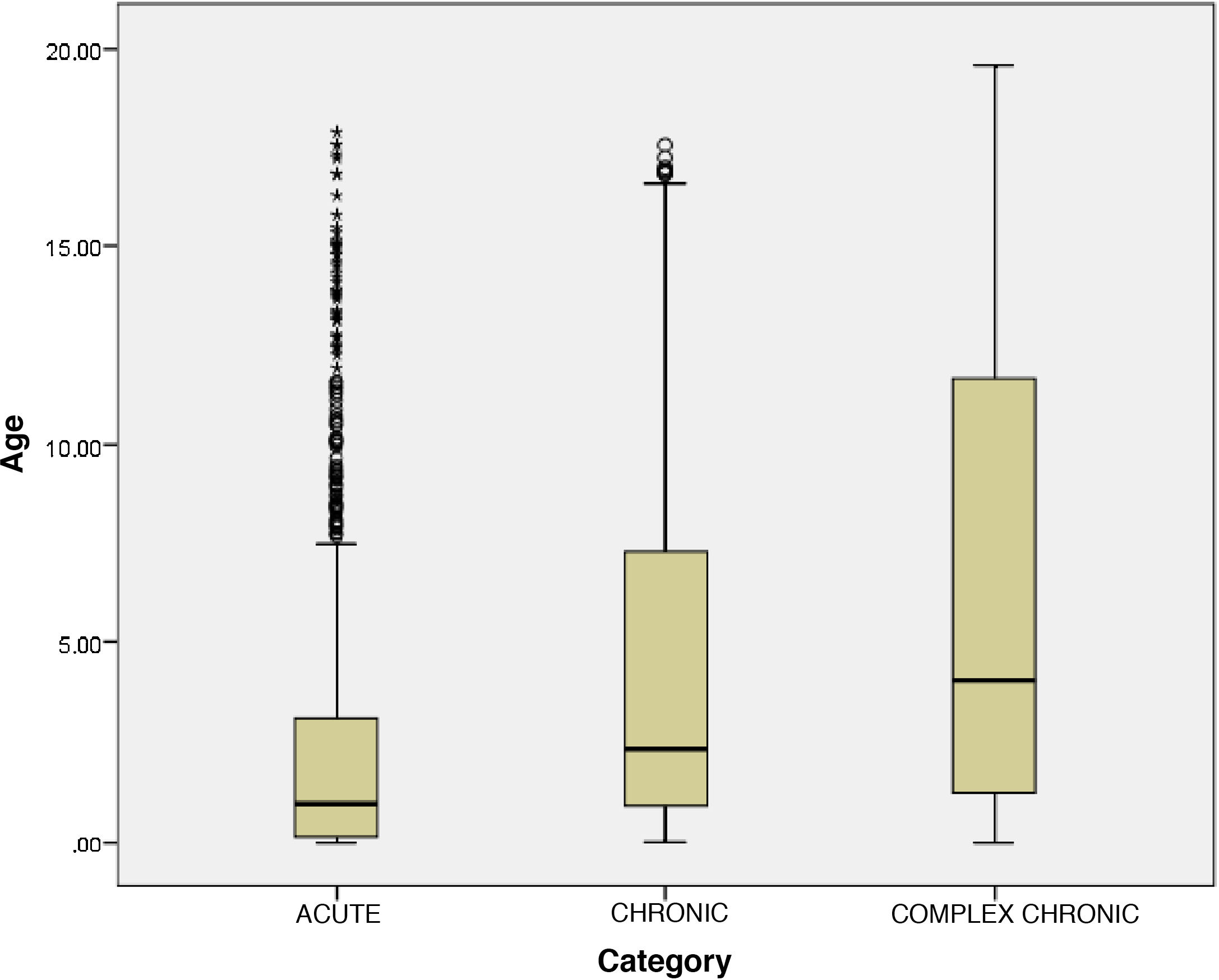
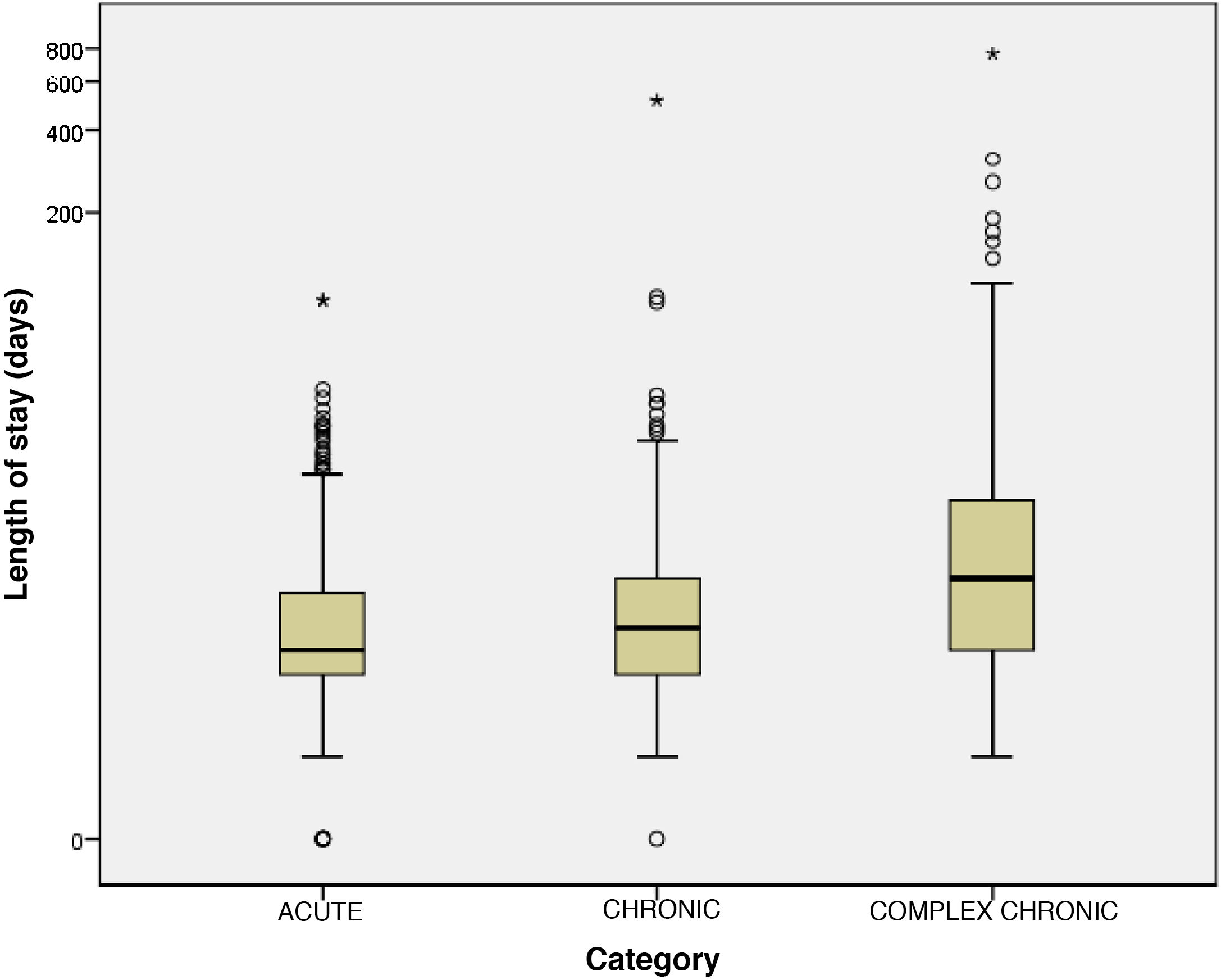
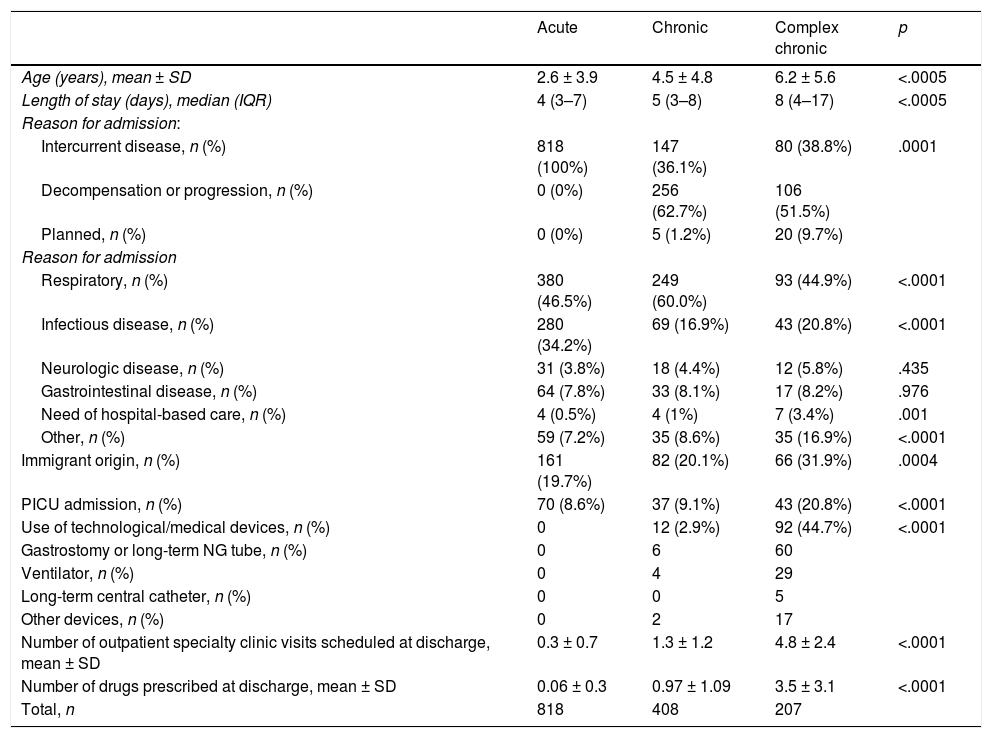
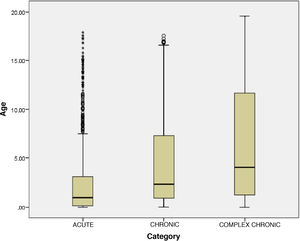
Comparative analysis of patient groups (acute, chronic or complex chronic disease)Fig. 1 presents the age distribution of patients in the different groups. Fig. 2 presents the distribution of patients in each group by length of stay. Table 2 summarises the main clinical differences between groups. We found a significantly lower mean age in patients with acute disease compared to patients with chronic and complex chronic disease. The median length of stay was higher in CCPs compared to the chronic and acute groups. In patients with chronic or complex chronic disease, the most frequent reason for admission was decompensation or progression of underlying disease, and CCPs required admission to the PICU more frequently than other patients. Planned admission was also significantly more frequent in CCPs. In the CCP group, 44.7% of patients depended permanently on medical devices to sustain vital functions. In the CCP group, there was a higher proportion of children of immigrant origin, and more drugs were prescribed and more follow-up visits to outpatient clinics scheduled at discharge compared to the other groups.
Boxplot of the distribution by length of stay (in days) of the different patient groups: acute (CRGs 1 and 2), chronic (CRGs 3–5) and complex chronic (CRGs 6, 7 and 9). Due to the skewed distribution of the data, with extreme value differences, we transformed data on the y-axis to a logarithmic scale (Log [length of stay]) to facilitate their visual representation.
Comparison of clinical characteristics of different patient subsets.
| Acute | Chronic | Complex chronic | p | |
|---|---|---|---|---|
| Age (years), mean ± SD | 2.6 ± 3.9 | 4.5 ± 4.8 | 6.2 ± 5.6 | <.0005 |
| Length of stay (days), median (IQR) | 4 (3–7) | 5 (3–8) | 8 (4–17) | <.0005 |
| Reason for admission: | ||||
| Intercurrent disease, n (%) | 818 (100%) | 147 (36.1%) | 80 (38.8%) | .0001 |
| Decompensation or progression, n (%) | 0 (0%) | 256 (62.7%) | 106 (51.5%) | |
| Planned, n (%) | 0 (0%) | 5 (1.2%) | 20 (9.7%) | |
| Reason for admission | ||||
| Respiratory, n (%) | 380 (46.5%) | 249 (60.0%) | 93 (44.9%) | <.0001 |
| Infectious disease, n (%) | 280 (34.2%) | 69 (16.9%) | 43 (20.8%) | <.0001 |
| Neurologic disease, n (%) | 31 (3.8%) | 18 (4.4%) | 12 (5.8%) | .435 |
| Gastrointestinal disease, n (%) | 64 (7.8%) | 33 (8.1%) | 17 (8.2%) | .976 |
| Need of hospital-based care, n (%) | 4 (0.5%) | 4 (1%) | 7 (3.4%) | .001 |
| Other, n (%) | 59 (7.2%) | 35 (8.6%) | 35 (16.9%) | <.0001 |
| Immigrant origin, n (%) | 161 (19.7%) | 82 (20.1%) | 66 (31.9%) | .0004 |
| PICU admission, n (%) | 70 (8.6%) | 37 (9.1%) | 43 (20.8%) | <.0001 |
| Use of technological/medical devices, n (%) | 0 | 12 (2.9%) | 92 (44.7%) | <.0001 |
| Gastrostomy or long-term NG tube, n (%) | 0 | 6 | 60 | |
| Ventilator, n (%) | 0 | 4 | 29 | |
| Long-term central catheter, n (%) | 0 | 0 | 5 | |
| Other devices, n (%) | 0 | 2 | 17 | |
| Number of outpatient specialty clinic visits scheduled at discharge, mean ± SD | 0.3 ± 0.7 | 1.3 ± 1.2 | 4.8 ± 2.4 | <.0001 |
| Number of drugs prescribed at discharge, mean ± SD | 0.06 ± 0.3 | 0.97 ± 1.09 | 3.5 ± 3.1 | <.0001 |
| Total, n | 818 | 408 | 207 | |
IQR, interquartile range; NG, nasogastric; PICU, paediatric intensive care unit; SD, standard deviation.
Based on the established definitions, 31 patients had CCC illness, which amounted to 15% of all CCPs and 2.16% of the sample. The median age of these patients was 3.6 years (IQR, 1.4–8.5; range, 0–19.6), and the median length of stay was 11 days (IQR, 5.0–19.0; range, 2–767).
Disease decompensation or progression was the reason for admission in 67.7% of patients with CCC illness (n = 21). Nearly half of these patients were of immigrant origin (51.6%; n = 16) and a high proportion were technology-dependent (80.6%; n = 25). In addition, 19.4% (n = 6) required admission to the PICU. These patients took a mean of 5 different drugs a day and were followed up by a mean of 6.5 medical or surgical specialists.
Proportion of prolonged hospitalisationsIn the period under study, there were a total of 101 hospital stays that lasted more than 1 month, with durations ranging from 1 month to 2.1 years (767 days). These stays corresponded to 50 patients (3.5% of the sample). Chronic complex patients accounted for 71.3% of prolonged stays. Of the 50 patients with prolonged stays, 29 (58%) had CCC illness.
DiscussionWe conducted a descriptive study of the proportion of CCPs in our setting. To our knowledge, this is the first study in Spain describing the importance of these patients in a large sample of hospitalised children and adolescents. We found that CCPs amounted to 14.4% of admissions to the department of paediatric internal medicine of a tertiary care hospital. This was significantly higher compared to the proportion reported in previous studies in the United States (10%).5,8,9 These differences may be explained by the difficulty in clearly establishing what may constitute complex chronic disease, as there are multiple definitions of the term and studies on the subject apply heterogeneous inclusion criteria. Nevertheless, most authors use the definition proposed by Cohen et al.5 and the CRG classification system,13 as we did in our study. The CRG classification divides the population into categories based on clinical characteristics and the complexity of health care needs. The advantage of using this system is that it takes multimorbidity into account, a factor associated with increased medical complexity. Classifying patients into clearly defined and mutually exclusive categories minimises the risk of bias in the definition of chronic complex patients.
Among the limitations of the study, we ought to highlight that it was conducted in a single tertiary care referral hospital that has a specific programme for the management of CCPs, and therefore the analysis may have overestimated the proportion of children with complex chronic disease in paediatric wards.
In the sample under study, we found that CCPs had longer hospitalisations, required PICU admission more frequently, were more likely to use medical devices and multiple drugs and required follow-up by a larger number of specialists. We also found a higher frequency of planned hospital admission in this group. Thus, as described in the previous literature,4,8–11 these patients consumed more health care resources, and therefore generated higher health care costs.
It is worth noting that although the hospital where the study was conducted has a specific programme for the management of paediatric CCPs, most hospitalisations in these group were due to decompensation or progression of chronic diseases. This may reflect the inherent medical fragility of CCPs, whose multiple needs may not be adequately met by the existing care model. Therefore, new and cost-effective approaches to treatment and follow-up are required to decrease the impact of disease on children and their families. In this regard, there is evidence that hospital at home programmes in coordination with primary care services reduce the use of inpatient care resources by CCPs.17–19 To date, few such programmes have been implemented in Spain, and other authors have already voiced the need to develop a specific care model for paediatric CCPs in our country.20 At present, there is a national consensus document that defines a framework for delivery of palliative care in children who require it, which would be applicable to some patients with complex chronic disease.21 However, the consensus has not resulted in a standardised care model for these patients and there are still regional differences in their management within Spain. Recently, it has been proposed that paediatric complex chronic disease units in tertiary care hospitals would be an appropriate model for management of this population in Spain, as it would improve the quality of life of patients and their families as well as the efficiency of the health care system.12
Another significant finding of the study was the high percentage of children of immigrant origin in the CCP group compared to the other 2 groups (a percentage that is even higher in the CCC subset, reaching 51.6%). To date, this phenomenon had not been described in Spain. Multiple factors that converge in specific immigrant populations (a higher frequency of consanguinity, lower frequency of prenatal care, deficient care in the country of origin, lower frequency of voluntary termination of pregnancy in case of severe foetal disease, etc.), combined with the increase in the survival of infants born with severe disease, may explain the greater prevalence of complex chronic disease in immigrant families.
Lastly, we ought to highlight that the presence of children considered to have CCC illness in Spain is now a demonstrated fact in Spain and that the use of health care resources by this subset of CCPs is even greater: in our study, 80.6% of these patients were technology-dependent, 19.4% required admission to the PICU and more than 46% had lengths of stay exceeding 1 month. It is likely that the existence of a hospital at home programme for CCPs in our hospital led to underestimation of prolonged hospitalisation in this population, as it makes early discharge possible during the subacute phase of disease through delivery of intensive follow-up care. Our findings on the high use of health care resources by patients with CCC illness were consistent with the data reported by hospitals in the United States22 on annual health care spending in children with chronic disease by CRG (including categories CRG 5–9), which reveal that patients with CCC (CRG 9), while amounting to less than one third of the total, account for 50% of total annual expenditures. These hospitals found that patients with cerebral palsy, followed in importance by patients that required mechanical ventilation and parenteral nutrition at home, accounted for 82% of the total health care costs in highly complex chronic patients.22 In light of the above, the need to devise a nationwide care delivery model for the management of these patients seems all the more urgent.
Our findings suggest that the proportion of CCPs out of all hospitalised paediatric patients is, in fact, substantial. This study paves the way for future research on the prevalence of paediatric complex chronic disease. Determining the actual frequency of CCPs in the general paediatric population would require collaborative studies with participation of different hospitals and primary care centres. In this regard, the identification of medical complexity at the level of the general paediatric population poses a series of challenges. First, there is a broad range of paediatric diseases that may be medically complex (including many rare diseases), contrary to the adult population, in which a small number of diseases accounts for a large proportion of CCPs. Second, the data that are available and can be analysed at the population level (mainly diagnostic and procedure codes) may not suffice to establish the level of complexity, as in the paediatric population, an accurate diagnosis may yet not have been established in many cases, or a given diagnosis may result in vastly different degrees of functional impairment and therefore of medical complexity. For this reason, in recent years multiple strategies have been explored to determine medical complexity in paediatrics, and the best approach is probably to use a combination of tools (administrative data, questionnaires, etc.).23 For the purpose of future research, it is necessary to develop and validate an instrument to establish the prevalence of paediatric patients with complex chronic disease in Spain. We ought to mention that the National Health System of Spain uses the diagnosis-related group (DRG) classification. This classification system groups patients into categories based on the cost and duration of hospitalisation. Since this classification is already in use in our region,24 it may be useful for identification of CCPs in different care settings and for comparing the proportion of patients with complex chronic disease in different facilities and different years.
In conclusion, our study evinced the importance of paediatric patients with chronic complex disease in the hospital care setting. Its findings can probably be generalised to other hospitals or health districts, but further research is required on the subject. This study provides a starting point in the investigation of the current situation of paediatric complex chronic illness in Spain and the characteristics of these patients. A debate at the national level is required to develop an integral health care model with the ultimate goals of improving quality of life in these patients and their families and optimising the efficiency of the health care system.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Penela-Sánchez D, Ricart S, Vidiella N, García-García JJ. Estudio de los pacientes pediátricos crónicos complejos ingresados en un servicio de pediatría a lo largo de 12 meses. An Pediatr (Barc). 2021;95:233–239.


![Boxplot of the distribution by length of stay (in days) of the different patient groups: acute (CRGs 1 and 2), chronic (CRGs 3–5) and complex chronic (CRGs 6, 7 and 9). Due to the skewed distribution of the data, with extreme value differences, we transformed data on the y-axis to a logarithmic scale (Log [length of stay]) to facilitate their visual representation. Boxplot of the distribution by length of stay (in days) of the different patient groups: acute (CRGs 1 and 2), chronic (CRGs 3–5) and complex chronic (CRGs 6, 7 and 9). Due to the skewed distribution of the data, with extreme value differences, we transformed data on the y-axis to a logarithmic scale (Log [length of stay]) to facilitate their visual representation.](https://static.elsevier.es/multimedia/23412879/0000009500000004/v1_202110020718/S2341287921001423/v1_202110020718/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w95erwEulN6Tmh1xJpRhO+VE=)


