The objective of this article was to estimate the type 1 diabetes mellitus (T1DM) incidence in the child population of the Community of Madrid (CM) and its evolution between 1997 and 2016, using the medical-administrative data of the regional registry of T1DM.
MethodsT1DM cases of children under 15 years of age, reported to the regional registry or collected from secondary sources were included: Spanish Diabetics Association (1997−2013), and from 2014 on the Basic Minimum Data Set (BMDS). Annual incidence rates were estimated per 100 000 person-years. The comparison of the rates was analysed using Poisson regression models using incidence ratios (IR).
ResultsA total of 2658 cases were identified as new diagnoses of T1DM. The mean incidence rate for 1997−2013 was 13.7 cases per 100 000 person-years. In the 2014−2016 period, 20 cases per 100 000 persons-years were registered using the BMDS. The age group with the highest incidence was 10−14 years in the two periods (16.6 vs. 25.5). In boys, the age with the highest incidence was 10–14 years in both periods (17.9 vs 30.4), and in girls, the age of 5–9 years (17.0 vs 25.1). Incidence rates decreased slightly in both genders until 2013 (from 15.0 to 11.6). In 2014−2016, the annual incidence rate varied between 18.4 and 21.1 cases (IR: 1.77). The incidence remained stable in children under 5 years old and increased from 5 to 14 years old.
ConclusionsThe CM is among the regions with a high incidence of T1DM. In its first phase, the regional registry underestimated the incidence of T1DM, and with the incorporation of the MBDS as a source of information, the estimates for the second period (2014−2016) are possibly closer to the actual incidence of T1DM. The data presented suggests the need to know the real evolution of the incidence of the disease by incorporating computerised health records.
El objetivo fue estimar la incidencia de diabetes mellitus tipo 1 (DM1) en la población infantil de la Comunidad de Madrid (CM) y su evolución entre 1997 y 2016, a partir de los datos médicos-administrativos del registro regional de DM1.
MétodosFueron incluidos los casos de DM1 de menores de 15 años, notificados al registro regional o captados de fuentes secundarias: Asociación Diabéticos Españoles (1997−2013) y a partir de 2014 del Conjunto Mínimo Básico de Datos hospitalario (CMBDS). Se estimaron tasas de incidencia anual por 100.000 personas-año. La comparación de las tasas se analizó mediante modelos de regresión de Poisson a través de razones de incidencia (RI).
ResultadosUn total de 2658 casos fueron identificados como nuevos diagnósticos de DM1. La tasa de incidencia media de 1997−2013 fue de 13,7 casos por 100.000 personas-año. En el periodo 2014−2016, utilizando el CMBDS se registraron 20,0 casos por 100.000. El grupo de edad con mayor incidencia fue el de 10−14 años en los dos periodos (16,6 vs 25,5). En los niños, la edad de mayor incidencia fue de 10 a 14 años en ambos periodos (17,9 vs 30,4) y en las niñas el de 5 a 9 años (17,0 vs 25,1). Las tasas de incidencia descendieron ligeramente en ambos sexos hasta 2013 (de 15,0 a 11,6); en 2014–2016 la tasa de incidencia anual varió entre 18,4 y 21,1 casos (RI: 1,77). La incidencia permaneció estable en menores de 5 años y aumentó de 5 a 14 años.
ConclusionesLa CM se sitúa entre las regiones de alta incidencia de DM1. En su primera fase, el registro regional infraestimaba la incidencia de DM1. Con la incorporación del CMBDS como fuente de información, las estimaciones del segundo periodo (2014−2016) son posiblemente más próximas a la incidencia real de DM1. Los datos que presentamos sugieren la necesidad de conocer la evolución real de la incidencia de la enfermedad incorporando los registros digitales sanitarios.
Type 1 diabetes mellitus (T1DM) is a common autoimmune disease in the child and adolescent population that requires life-long treatment with insulin from diagnosis.1,2 When it comes to its natural history, children and adolescents with T1DM may develop renal disease, retinopathy, peripheral neuropathy, high blood pressure or coronary disease during adolescence or in adulthood.1 The mortality of patients with T1DM is greater compared to the general population due to acute complications like ketoacidosis or hypoglycaemic episodes.3
In the Community of Madrid (CM), treatment with insulin is usually initiated in hospital, where patients and their families receive education on diabetes and its management during the stay, and the follow-up is generally carried out at the primary care level.4
Globally, the incidence of T1DM varies widely between countries. It is estimated that approximately 500 000 children under 15 years had T1DM and approximately 80 000 first received a diagnosis of T1DM in 2013 worldwide.5 Based on data from the 1990s, the World Health Organization grouped countries by incidence category (very low, <1 per 100 000/year; low, 1–4.99 per 100 000/year; intermediate, 5−9.99 per 100 000/year; high, 10–19.99 per 100 000/year, and very high, ≥20 per 100 000/year). The highest incidence rates were found in Europe and the United States.6
In 1996, the Working Group on Epidemiology of the Sociedad Española de Diabetes (Spanish Society of Diabetes) published methodological guidelines for studying the incidence of T1DM in Spain.7 At present, there are numerous registers of T1DM in children under 15 years that apply heterogeneous methods and report incidence values that differ substantially between autonomous communities, from 11.5 cases per 100 000 inhabitants per year in to 27.6 in Castilla La Mancha. The mean estimated incidence in Spain in 2013 was of 17.69 cases per 100 000 inhabitants per year.8
The aim of our stud was to estimate the incidence of T1DM in the under-15 population in the CM and analyse time trends in incidence in the 1997−2013 and 2014−2016 periods based on the clinical and administrative records of the regional T1DM register.
Materials and methodsData sources: we gathered data from the T1DM register of the CM created in 1997. We included every case of type 1 diabetes diagnosed between January 1, 1997 and December 31, 2016 in children aged less than 15 years residing in the CM. The primary sources of the data were the paediatric endocrinology units of all the public and private hospitals in the CM. New cases were notified by fax and electronic mail to the Department of Epidemiology of the Directorate General of Public Health, where the register data entry, scrubbing and analysis took place; each year, case data from secondary sources were added to the register.
To improve the completeness of the register, from January 1, 2014, new secondary sources of data were added. Our report includes an analysis of 2 periods, 1997−2013 and 2014−2016, established based on the different secondary sources.
In the first period (1997−2013), the secondary data consisted of cases reported by the Asociación de Diabéticos Española (Spanish association of individuals with diabetes). In the second period (2014−2016), the register included cases with a diagnostic code of diabetes mellitus in the minimum basic dataset (CMBDS) records of hospital discharge reports, which were verified by consulting the HORUS centralised information system that includes health care records from the primary care system of Madrid (APMADRID) and public medical speciality clinics in the entire CM. The T1DM incidence register of the CM is not anonymous and requires personally identifiable information. Thus, cases identified through the CMBDS of discharge reports of private hospitals were only included in the register if the patient could be identified through the documentation of personal health care card data. These cases were verified by finding documentation of the onset of diabetes and prescription of insulin in the HORUS database.
The register applies the case definition and age group criteria established by the Multinational Project for Childhood Diabetes Research Group.6 Cases of T1DM eligible for inclusion in the register were those diagnosed by a medical professional in individuals aged less than 15 years that began insulin injections before their 15th birthday and were residing in the CM at the time of the first insulin administration.6 We excluded cases of other types of diabetes (maturity-onset diabetes of the young [MODY], diabetes secondary to endocrine or infectious diseases or type 2 diabetes).
Statistical analysis: we present the distribution of newly diagnosed cases by age group (0−4, 5−9 and 10−14 years) and by sex for each year and for the 20-year period under study. We estimated annual incidence values and the mean incidence expressed as cases per 100 000 individuals per year, for the entire period under study. We obtained the value for the denominator from updated CM census data for the corresponding age group and sex. We estimated 95% confidence intervals (CIs) assuming an underlying Poisson distribution. To compare and estimate incidence trends in different age groups and by sex, we estimated the incidence rate ratio (IRR) using Poisson regression.
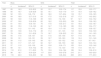
ResultsTable 1 presents the mean annual incidence by age and sex in the 1997−2013 period, with new cases diagnosed in a total of 2046 individuals. Fifty-one percent were male, with a mean age of 8.2 years and a median of 8.7 years. The mean age in boys was 8.4 years compared to 8.1 years in girls, values that remained stable throughout the follow-up.
Mean annual incidence of type 1 diabetes mellitus by sex and age group, 1997–2013 period. Community of Madrid.
| Age | Boys | Girls | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Incidencea | 95% CI | n | Incidencea | 95% CI | n | Incidencea | 95% CI | |
| 0−4 years | 268 | 10.0 | 8.8−11.2 | 249 | 9.9 | 8.6−11.1 | 517 | 10.0 | 9.1−10.8 |
| 5−9 years | 339 | 12.7 | 11.3−14.1 | 397 | 17.0 | 15.3−18.6 | 736 | 15.3 | 14.2−16.4 |
| 10−14 years | 439 | 17.9 | 16.2−19.6 | 354 | 15.2 | 16.1−24.1 | 793 | 16.6 | 15.4−17.8 |
| Total | 1046 | 13.4 | 12.6-14.2 | 1000 | 13.9 | 13.0-14.8 | 2046 | 13.7 | 13.2-14.6 |
CI, confidence interval.
The overall mean annual incidence of T1DM was 13.7 cases per 100 000 inhabitants (95% CI, 13.2−14.6); 13.4 in boys and 13.9 in girls.
The annual incidence by age group (expressed as cases per 100 000 inhabitants) was 10.0 (95% CI, 9.1−10.8) in children aged 0–4 years, 15.3 (95% CI, 14.2−16.4) in children aged 5–9 years and 16.6 (95% CI, 15.4−17.8) in children aged 10–14 years. Using Poisson regression, the incidence was highest in the 10−14 years group, with an IRR of 1.65 relative to the 0−4 years group (P < .001), followed by the 5−9 years group, with an IRR of 1.54 (95% CI, 1.47–1.84; P < .001).
The analysis by sex revealed that in the 0−4 years age group, the incidence was similar in boys and girls. In boys, the incidence peaked at 10–14 years with 17.9 cases (IRR, 1.76 relative to 0−4 years group; P < .001), and in girls it peaked at 5–9 years with 17.0 cases (IRR, 1.72; P < .001) per 100 000 inhabitants per year.
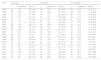
Table 2 presents the mean incidence for the 2014−2016 period. A total of 612 new cases were identified (52.9% in boys) for an overall mean incidence of 20 cases per 100 000 inhabitants per year. Based on age, as occurred in the previous period, the incidence peaked at age 10–14 years with a mean of 25.5 cases per year (IRR, 2.2 relative to the 0−4 years group; P < .001). By sex, in boys incidence peaked at age 10–15 years with 30.4 cases (IRR, 2.82; 95% CI, 2.1–3.8; P < .001) and in girls at age 5–9 years with 25.5 cases (IRR, 2.05; 95% CI, 1.5–2.8, P < .001) per 100 000 inhabitants per year.
Mean annual incidence of type 1 diabetes mellitus by sex and age group, 2014–2016 period. Community of Madrid.
| Age | Boys | Girls | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Incidencea | 95% CI | n | Incidencea | 95% CI | n | Incidencea | 95% CI | |
| 0−4 years | 54 | 10.8 | 7.9−13.6 | 58 | 12.2 | 9.1−15.4 | 112 | 11.3 | 9.2−13.4 |
| 5−9 years | 116 | 23.2 | 18.9−27.4 | 133 | 25.1 | 20.8−29.3 | 249 | 22.8 | 20.0−25.6 |
| 10−14 years | 154 | 30.4 | 25.6−35.2 | 97 | 20.1 | 16.1−24.1 | 251 | 25.5 | 22.3−28.6 |
| Total | 324 | 21.5 | 19.1−23.8 | 288 | 19.3 | 17.1−21.6 | 612 | 20.0 | 18.4−21.6 |
CI, confidence interval.
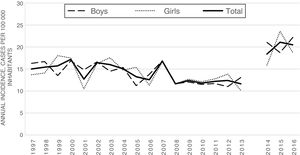
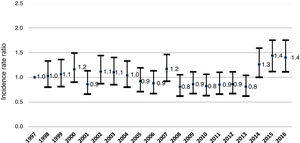
Table 3 and Fig. 1 present the incidence of T1DM by age group and sex in the 1997–2016 period.
Annual incidence of type 1 diabetes mellitus by sex, 1997–2016. Community of Madrid.
| Year | Boys | Girls | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Incidencea | 95% CI | n | Incidencea | 95% CI | n | Incidencea | 95% CI | |
| 1997 | 65 | 16.3 | 12.3−20.2 | 52 | 13.7 | 10.0−17.4 | 117 | 15.0 | 12.3−17.7 |
| 1998 | 65 | 16.7 | 12.6–20.8 | 52 | 14.1 | 10.3–17.9 | 117 | 15.4 | 12.6–18.2 |
| 1999 | 52 | 13.5 | 9.8−17.2 | 66 | 18.0 | 13.7−22.4 | 118 | 15.7 | 12.9−18.5 |
| 2000 | 64 | 16.9 | 12.7−21.0 | 63 | 17.5 | 13.2−21.8 | 127 | 17.2 | 14.2−20.2 |
| 2001 | 58 | 14.8 | 11.0−18.6 | 39 | 10.5 | 7.2−13.8 | 97 | 12.7 | 10.2−15.2 |
| 2002 | 67 | 16.6 | 12.6−20.6 | 62 | 16.2 | 12.2−20.3 | 129 | 16.4 | 13.6−19.3 |
| 2003 | 61 | 14.5 | 10.9−18.1 | 70 | 17.6 | 13.5−21.7 | 131 | 16.0 | 13.3−18.7 |
| 2004 | 66 | 15.3 | 11.6−19.0 | 60 | 14.7 | 11.0−18.5 | 126 | 15.0 | 12.4−17.7 |
| 2005 | 50 | 11.2 | 8.1−14.3 | 65 | 15.4 | 11.7−19.1 | 115 | 13.3 | 10.8−15.7 |
| 2006 | 63 | 13.8 | 10.4−17.2 | 49 | 11.3 | 8.1−14.5 | 112 | 12.6 | 10.2−14.9 |
| 2007 | 78 | 16.9 | 13.1−20.6 | 73 | 16.7 | 12.8−20.5 | 151 | 16.8 | 14.1−19.5 |
| 2008 | 55 | 11.6 | 8.6−14.7 | 52 | 11.6 | 8.5−14.8 | 107 | 11.6 | 9.4−13.8 |
| 2009 | 59 | 12.1 | 9.0−15.1 | 59 | 12.7 | 9.5−16.0 | 118 | 12.4 | 10.1−14.6 |
| 2010 | 58 | 11.5 | 8.5−14.5 | 58 | 12.1 | 9.0−15.2 | 116 | 11.8 | 9.7−14.0 |
| 2011 | 60 | 11.7 | 8.7−14.7 | 62 | 12.7 | 9.6−15.9 | 122 | 12.2 | 10.0−14.4 |
| 2012 | 57 | 11.0 | 8.2−13.9 | 68 | 13.8 | 10.6−17.1 | 125 | 12.4 | 10.2−14.6 |
| 2013 | 68 | 13.1 | 10.0−16.2 | 50 | 10.1 | 7.3−12.9 | 118 | 11.6 | 9.5−13.7 |
| 2014 | 110 | 21.0 | 17.1−25.0 | 79 | 15.9 | 12.4−19.4 | 189 | 18.4 | 15.8−21.0 |
| 2015 | 98 | 18.7 | 15.0–22.4 | 117 | 23.6 | 19.3–27.8 | 215 | 21.1 | 18.3–23.9 |
| 2016 | 116 | 22.3 | 18.2−26.3 | 92 | 18.6 | 14.8−22.4 | 208 | 20.5 | 17.7−23.3 |
CI, confidence interval.
In 2016, the annual incidence was 20.5 cases per 100 000 inhabitants, compared to 10.5 cases in 1997. When we compared the annual incidence from 1997 to 2013, we observed a decreasing trend with an IRR of 0.98 (95% CI, 0.97−0.99; P < .05). In the 2014−2016 period, the annual incidence was higher and remained stable through time (IRR, 1.05; 95% CI, 0.95–1.16).
When we compared the incidence based on age group (Table 4), we found that the incidence remained stable or slightly declined in the 0–4 years group in both the 1997−2013 and 2014−2016 periods. In the 5–9 years and 10–14 years groups, the incidence was stable or declined slightly through 2013, while in the 2014−2016 period the incidence increased compared to the initial period (Fig. 2).
Annual incidence of type 1 diabetes mellitus by age group, 1997–2016. Community of Madrid.
| Year | 0−4 years | 5−9 years | 10−14 years | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Incidencea | 95% CI | n | Incidencea | 95% CI | n | Incidencea | 95% CI | |
| 1997 | 32 | 14.1 | 9.2−19.0 | 35 | 14.0 | 9.3−18.6 | 50 | 16.5 | 11.9−21.1 |
| 1998 | 30 | 13.3 | 8.5−18.0 | 41 | 16.6 | 11.5−21.6 | 46 | 16.1 | 11.5−20.8 |
| 1999 | 28 | 12.0 | 7.5-16.4 | 42 | 17.2 | 12.0−22.4 | 48 | 17.6 | 12.6−22.5 |
| 2000 | 33 | 14.1 | 9.3−18.9 | 46 | 19.1 | 13.6−24.3 | 48 | 18.1 | 13.0−23.3 |
| 2001 | 19 | 7.5 | 4.1−10.8 | 37 | 15.0 | 10.2−19.9 | 41 | 15.6 | 10.8−20.3 |
| 2002 | 30 | 11.2 | 7.2−15.2 | 50 | 19.8 | 14.3−25.3 | 49 | 18.4 | 13.3−23.6 |
| 2003 | 39 | 13.6 | 9.4−17.9 | 48 | 18.4 | 13.2−23.7 | 44 | 16.1 | 11.4−20.9 |
| 2004 | 38 | 12.5 | 8.4−16.5 | 48 | 18.4 | 13.2−23.6 | 40 | 14.6 | 10.1−19.2 |
| 2005 | 34 | 10.5 | 7.0−14.1 | 39 | 14.5 | 9.9−19.0 | 42 | 15.2 | 10.6−19.8 |
| 2006 | 34 | 9.9 | 6.6−13.2 | 32 | 11.6 | 7.6−15.7 | 46 | 16.8 | 12.0−21.7 |
| 2007 | 38 | 11.2 | 7.6−14.7 | 47 | 16.4 | 11.7−21.1 | 66 | 24.1 | 18.3−30.0 |
| 2008 | 22 | 6.5 | 3.8−9.2 | 46 | 15.3 | 10.9−19.7 | 39 | 13.9 | 9.6−18.3 |
| 2009 | 26 | 7.3 | 4.5–10.2 | 53 | 16.8 | 12.5−21.3 | 39 | 13.8 | 9.4−18.1 |
| 2010 | 24 | 6.6 | 3.9−9.2 | 47 | 14.3 | 10.2−18.4 | 45 | 15.6 | 11.0−20.1 |
| 2011 | 31 | 8.4 | 5.4−11.4 | 41 | 12.2 | 8.5–15.9 | 50 | 16.9 | 12.2−21.6 |
| 2012 | 22 | 6.0 | 3.5−8.5 | 46 | 13.5 | 9.6−17.4 | 57 | 19.0 | 14.1−23.9 |
| 2013 | 37 | 10.2 | 6.9–13.5 | 38 | 10.9 | 7.4−14.4 | 43 | 14.1 | 9.9−18.3 |
| 2014 | 40 | 12.0 | 8.3−15.7 | 67 | 18.2 | 13.8−22.6 | 82 | 25.1 | 19.7−30.6 |
| 2015 | 30 | 9.3 | 6.0−12.6 | 93 | 25.3 | 20.2−30.5 | 92 | 27.8 | 22.1−33.5 |
| 2016 | 42 | 12.7 | 8.8−16.5 | 89 | 25.0 | 19.8−30.2 | 77 | 23.4 | 18.2−28.7 |
CI, confidence interval.
As regards the completeness of the register, Table 5 presents the sources of the incidence data based on the reporting institution. In the 1997−2013 period, 94.92% of cases were reported by hospitals, while in the 2014−2016 this category amounted to 55.7% of the total. In the 2014−2016 period, data for 44.28% of cases were obtained from secondary sources (CMBDS). The time trends in incidence by age group and sex in the period under study are summarised in Table 6, which can be found in Appendix B (Supplemental material).
Source of data on cases of type 1 diabetes mellitus by reporting institution, 1997–2016.
| 1997−2013 | 2014−2016 | Total | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Hospitals | 1942 | 94.9 | 341 | 55.7 | 2283 | 85.9 |
| ADE | 81 | 4.0 | 0 | 0.00 | 81 | 3.0 |
| MBDS | 23 | 1.1 | 271 | 44.3 | 294 | 11.1 |
| Total | 2046 | 100 | 612 | 100 | 2658 | 100 |
ADE, Asociación de Diabéticos Españoles; MBDS, minimum basic data set (discharge report).
The incidence of T1DM recorded in the CM in 1997 was of 15.0 cases per 100 000 inhabitants, compared to 20.0 cases in 2016. Between 1997 and 2013, the incidence of T1DM exhibited a mildly decreasing trend reaching approximately 14 cases per 100 000 inhabitants. In the 2014−2016 period, with the incorporation of data from the MBDS of discharge reports as a secondary source, the documented incidence increased to approximately 20 cases per 100 000 inhabitants. The risk of developing T1DM was similar in boys and girls and higher at ages 5–9 years and 10–14 years compared to 0–4 years. In boys, the risk peaked at age 10–14 years in girls at age 5–9 years.
It is well known that the incidence of childhood diabetes varies widely between countries and regions worldwide.6 In China, the incidence was 0.1 cases per 100 000 inhabitants per year in the 1990–1994 period, and in Finland it was 62.4 cases in the 2006–2011 period.9 In Spain, the reported incidence varies between autonomous communities, with a mean nationwide incidence of 17.7 cases per 100 000 inhabitants per year.8 The incidence in the CM found in our study, of approximately 20 cases per 100 000 inhabitants, is in the midrange relative to the rest of autonomous community.
Zorrilla Torras et al. (2009) estimated that the completeness of the regional T1DM register in the 1997–2005 period was of 82.2% using the capture-recapture method and based on the 2 sources of data used at the time, which would correspond to an actual mean annual incidence of approximately 20.0 cases per 100 000 inhabitants.10 There was evidence that in the later years, reporting of cases from hospitals decreased due to the manual notification process and the move of some of the reporting paediatricians to different hospitals. The progressive decline in completeness encouraged us to use the MBDS as a secondary source.
With the incorporation of the MBDS as a secondary source in 2014, the completeness of the register has improved substantially; thus, in the 2014−2016 period, 44.28% of cases were identified through the use of the MBDS as a secondary source. In fact, we verified that every case in the register reported directly by hospitals was documented in the MBDS database, which leads us to believe that this is a good source to pursue the exhaustive identification of newly diagnosed cases.
Due to the above, we think that the increase in the number of registered cases in the 2014−2016 period to an observed incidence that was also approximately 20 cases per 100 000 inhabitants was probably due not to an increase in the actual incidence of T1DM, but to an improvement in the completeness of the register thanks to the automatic inclusion in the register of cases recorded in the MBDS system from 2014, along with the verification of cases through the review of primary care and specialty clinic health records. The incidence values obtained in the latter period under study are probably closer to the actual incidence of disease in the CM, assuming that the incidence remained stable with small variations throughout the study period. However, due to changes in the completeness of the register we cannot determine whether the incidence has remained stable or varied throughout the study period. Automatic reporting systems need to be incorporated into the register at some point in the future to guarantee its completeness.
In agreement with the previous literature, the incidence of diabetes in the under-15 population was similar in both sexes. We found the overall incidence peak irrespective of sex is, as reported in most published studies, in the 10–14 years group, and the lowest incidence in the 0–4 years group.11,12 Our data is also consistent with previous studies in finding an incidence peak in boys at age 10–14 years compared to 5–9 years in girls.11 In girls, the incidence of T1DM was lower compared to boys at 10–14 years and higher at age 5–9 years.
There are limitations to our study, starting with the fact that every governmental epidemiological register tends to underestimate incidence due to lack of completeness. The register may also include cases in children from other autonomous communities that registered in the health care system of the CM for follow-up and were treated as residents, but these cases are probably few as T1DM is a disease with an abrupt onset that in most cases requires hospital admission at the time of diagnosis. The problems associated with the lack of completeness of the register in the early years have been partially controlled through the incorporation of more complete secondary sources. On the other hand, cases of other types of diabetes, such as MODY, iatrogenic diabetes or even type 2 diabetes, may have been included in the register by mistake.
The greatest strength of our study is that it was conducted at the population level and that we confirmed cases applying standardised criteria through the review of health records. The incorporation of MBDS discharge data as a secondary source resulted in a more exhaustive identification of cases, as this system includes data from public and private hospitals, thus covering the entire population.
In conclusion, our study produced estimates of the annual incidence of T1DM in the entire paediatric population under 15 years of the CM, overall and by sex and age group (0−4, 5−9, 10−14 years). In order to improve the validity and completeness of the data, we need to increase reporting by paediatric endocrinologists and incorporate electronic record systems, such as the primary care (APMADRID) and hospital discharge report (MBDS) systems. The existence in the CM of a universal electronic medical records system in primary care with a standardised patient record format that uses the International Classification of Primary Care, 2nd edition (ICPC-2), which assigns a specific code to insulin-dependent diabetes mellitus (T89), would allow the identification of new cases diagnosed in children under 15 years and their inclusion in the register quicker and without adding to the workload of health care professionals. The automatic capture of cases from hospital discharge reports allows a more exhaustive retrieval of clinical data, given the greater specificity of the applied coding system (ICD-9-CM through 2016, ICD-10, Spanish edition, from 2017), although with greater delay, but advances in the digitalization of health records, both in inpatient care and emergency and outpatient care settings, would allow consideration of other strategies of automatic capture of public health system data in the medium term.
FundingThis study was fully by the Department of Health of the Community of Madrid.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank all reporting paediatricians for their altruistic participation. We also thank Luis Miguel Blanco Ancos for the design and maintenance of the database and Vicenta María Blasco Mejía, Begoña García Moles and Guadalupe Otero Blanco, for entering the data and communicating with reporters.
Please cite this article as: Ortiz-Marrón H, del Pino Valero V, Esteban-Vasallo M, Zorrilla Torras B, Ordobás Gavín M. Evolución de la incidencia de diabetes mellitus tipo 1 (0–14 años) en la Comunidad de Madrid, 1997–2016. An Pediatr (Barc). 2021;95:253–259.