Unilateral pulmonary artery agenesis (UPAA) is a rare malformation that may present in isolation or being associated with cardiovascular malformations such as tetralogy of Fallot, transposition of the great vessels, septal defects and aortic arch malformations.1 Its prevalence in the absence of congenital cardiovascular malformations is of one in 200000–300000 individuals, and it is usually underdiagnosed in the paediatric age group.
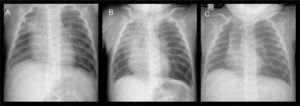
We present the case of a male infant aged 4 months with no relevant medical history and normal prenatal ultrasound findings that was admitted for acute bronchiolitis caused by human parainfluenza virus type 3, with evidence of lung contraction in the right hemithorax and increased density in the anterior segment of the upper right lobe on chest X-ray. The patient was admitted two more times, at 5 and 8 months, due to obstructive bronchiolitis manifesting with cough, hypoxaemia, wheezing and laboured breathing. In the second hospitalization, respiratory syncytial virus was isolated from a nasopharyngeal aspirate sample. The chest X-rays performed during these episodes showed progressive compression of the right hemithorax with ipsilateral mediastinal shift and hyperinflation of the left lung with herniation of the left upper lobe towards the right lung (Fig. 1). These findings led to the performance of a computed tomography (TC) scan with contrast, which revealed the absence of the proximal section of the right pulmonary artery with mild hypoplasia of the ipsilateral lung and the presence of two collateral vessels originating in the descending aorta (Fig. 2) and supplying the right lung, with a tortuous trajectory and extensive branching. The findings were compatible with right UPAA. The cardiologic workup was completed with an echocardiographic examination that ruled out the presence of other congenital malformations. The clinical manifestations of the patient included recurrent episodes of obstructive bronchitis of mild to moderate severity with absence of symptoms between episodes and normal findings in physical examination. The patient's growth and development have been normal and he is not receiving specific treatment for this condition due to the absence of complications and severe symptoms until present.
(A) Chest helical CT with contrast revealing right pulmonary artery agenesis and right pulmonary hypoplasia. (B) Chest helical CT with 3D image reconstruction. (B.1) Detail of right pulmonary artery agenesis. (B.2) Collateral vessels originating in the descending aorta that supply the right lung parenchyma. (B.3) Right pulmonary hypoplasia.
Unilateral pulmonary artery agenesis results from the intrauterine involution of the proximal sixth aortic arch, which leads to the absence of the proximal pulmonary artery. The foetal development of the lungs and the associated bronchovascular anatomy are usually normal, since the hilar and distal pulmonary arteries and their branches are supplied by an ipsilateral patent ductus arteriosus, although they are not connected to the pulmonary trunk. After birth, closure of the ductus arteriosus leads to a reduction in blood flow that in turn results in pulmonary hypoplasia and the development of aortopulmonary collateral vessels.2 We believe that these are the reasons why no anomalies were detected in our patient in prenatal ultrasounds and pulmonary and vascular manifestations developed after birth.
Patients with isolated UPAA may be asymptomatic, with the disease being detected by chance when chest radiography is performed. Other patients may present with respiratory distress and heart failure, recurrent respiratory disease, exercise limitation, haemoptysis and/or pulmonary hypertension (PHTN).3 In infants aged less than one year, there is a predominance of respiratory distress symptoms (56%) associated with PHTN with subsequent heart failure. After one year of age, children may present with recurrent respiratory infections (23–37%) and/or haemoptysis (14–20%) due to increased aortopulmonary collateral circulation. In adulthood, UPAA is also associated with exercise limitation (18–45%). Physical examination findings may be normal, and abnormal findings on auscultation may include detection of a heart murmur and/or hypoventilation with or without abnormal lung sounds in the hypoplastic hemithorax.
The final diagnosis is based on imaging tests.4 Chest X-rays show an ipsilateral contracted lung with ipsilateral mediastinal shift and hyperinflation of the contralateral lung that may be accompanied by herniation towards the affected side.5 The diagnosis is confirmed by chest CT and/or MRI with contrast, and the diagnostic workup is completed with echocardiography.
At present, the most widely accepted approach to the management of isolated UPAA is conservative treatment of asymptomatic forms and surgical intervention in cases of severe disease or with severe complications.4 The first-line approach in the surgical treatment of UPAA is two-stage repair with stenting of the ductus arteriosus followed by surgical anastomosis. Some studies report the use of surgery even in asymptomatic cases, but surgical intervention in these patients is very controversial because there is a high probability of reintervention due to postoperative complications such as thrombosis of primary surgical anastomosis.6 The associated PHTN can be treated with antihypertensive drugs, and haemoptysis can be treated by collateral artery embolization. Lobectomy or pneumonectomy can be considered in cases with haemoptysis that does not respond to embolization or with recurrent respiratory infections that result in complications such as bronchiectasis.
Please cite this article as: Adán Lanceta V, Jiménez Olmos A, Martín de Vicente C, García Íñiguez JP. Agenesia aislada de la arteria pulmonar derecha. An Pediatr (Barc). 2017;86:45–46.