Poisonings by illegal drugs are rarely seen in paediatric emergency departments (PEDs) and constitute approximately 1.5% of the total cases of poisoning.1 They usually occur in older patients that are exposed to these drugs in a recreational context, and cannabis is the substance most frequently involved.2
However, on rare occasions, PEDs manage young children that have been exposed to illegal drugs. These cases usually involve unintentional drug exposure resulting from the drive to explore characteristic of this age group.
Although it has been described that the use of psychoactive substances in society at large carries the risk of minors being exposed to them, there are few published studies on the subject.3 It is likely that contact with health care services occurs in cases in which the minor exhibits significant symptoms,4 but the actual number of poisonings may exceed the documented number, as in some cases the symptoms may be minimal or short-lived.
This study analyses the prevalence of this type of poisonings in the PEDs, as well as their characteristics and the way in which they are managed in these settings, based on the data of a prospective register of poisoning cases made by the Toxicology Surveillance System of the Spanish Society of Paediatric Emergency Care (Observatorio Toxicológico de la Sociedad Española de Urgencias de Pediatría) between October 2008 and June 2015. The study was approved by the Committee on Ethics and Clinical Research of the Basque Country. Appendix A lists the participating hospitals.
The data collection protocol applied to each patient included the following variables: age and sex; toxic substance; poisoning setting; family history of substance abuse; potential for exposure to the substance; previous outpatient assessment and/or treatment; circumstances leading to transfer to the PED; signs and symptoms; diagnostic testing and/or treatments in the PED; patient destination after discharge and outcome.
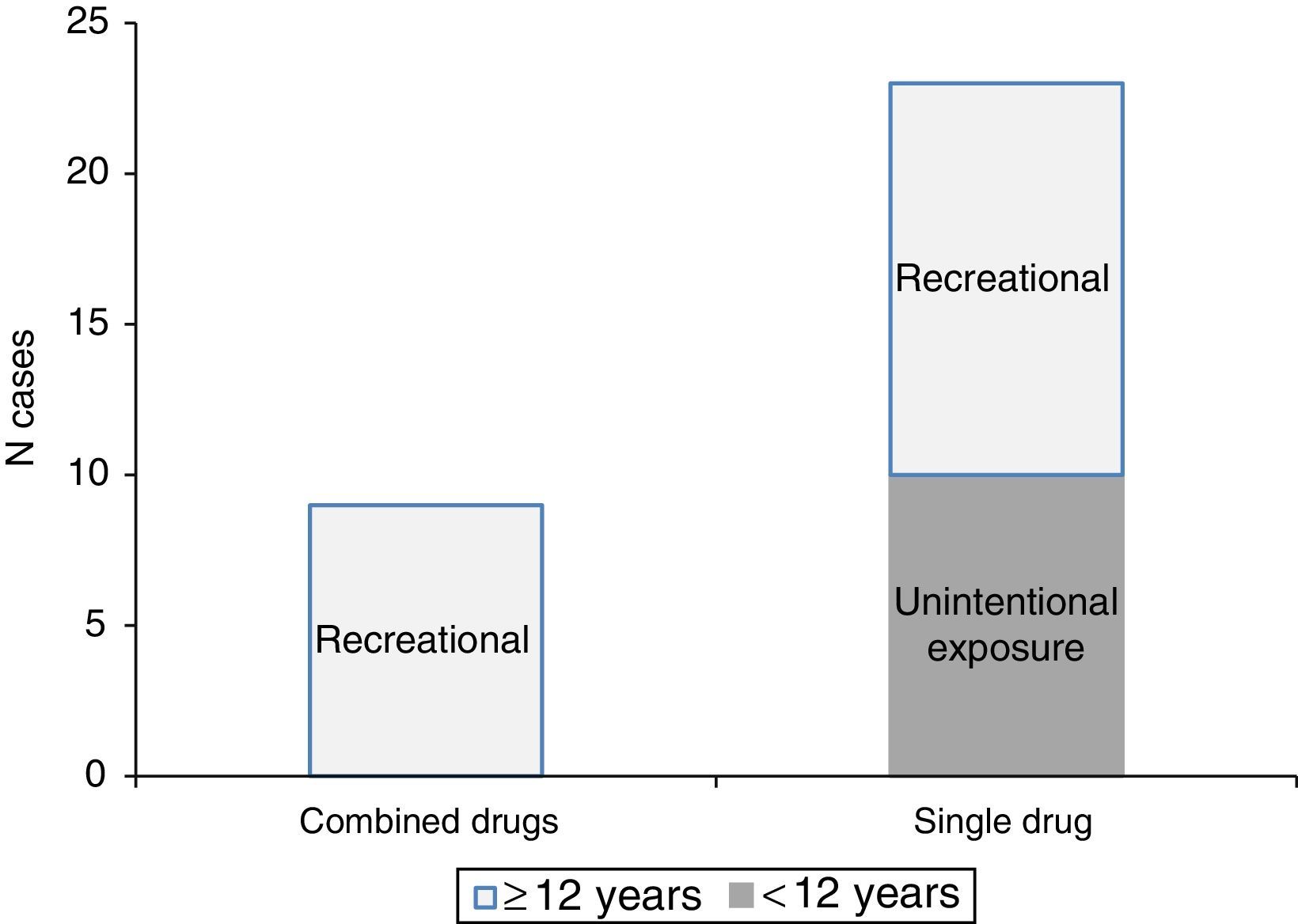
In the period under study, 413461 emergency visits were managed in the participating PEDs, of which 1139 corresponded to poisonings (0.27%). Of the latter, 32 cases (2.8%) corresponded to poisonings by illegal substances: 23 involving a single substance and 9 involving a combination of substances. Of the poisonings involving a single substance, 10 (43.5%) corresponded to unintentional exposures in children aged less than 3 years.
Fig. 1 shows the distribution of poisonings by illegal drugs by reason for exposure and patient age. There is a gap in this distribution between ages 3 and 11 years, probably due to an overall decline in the frequency of unintentional exposures at these ages, which at the same time are below the usual age band at which intoxications are due to recreational drug use.
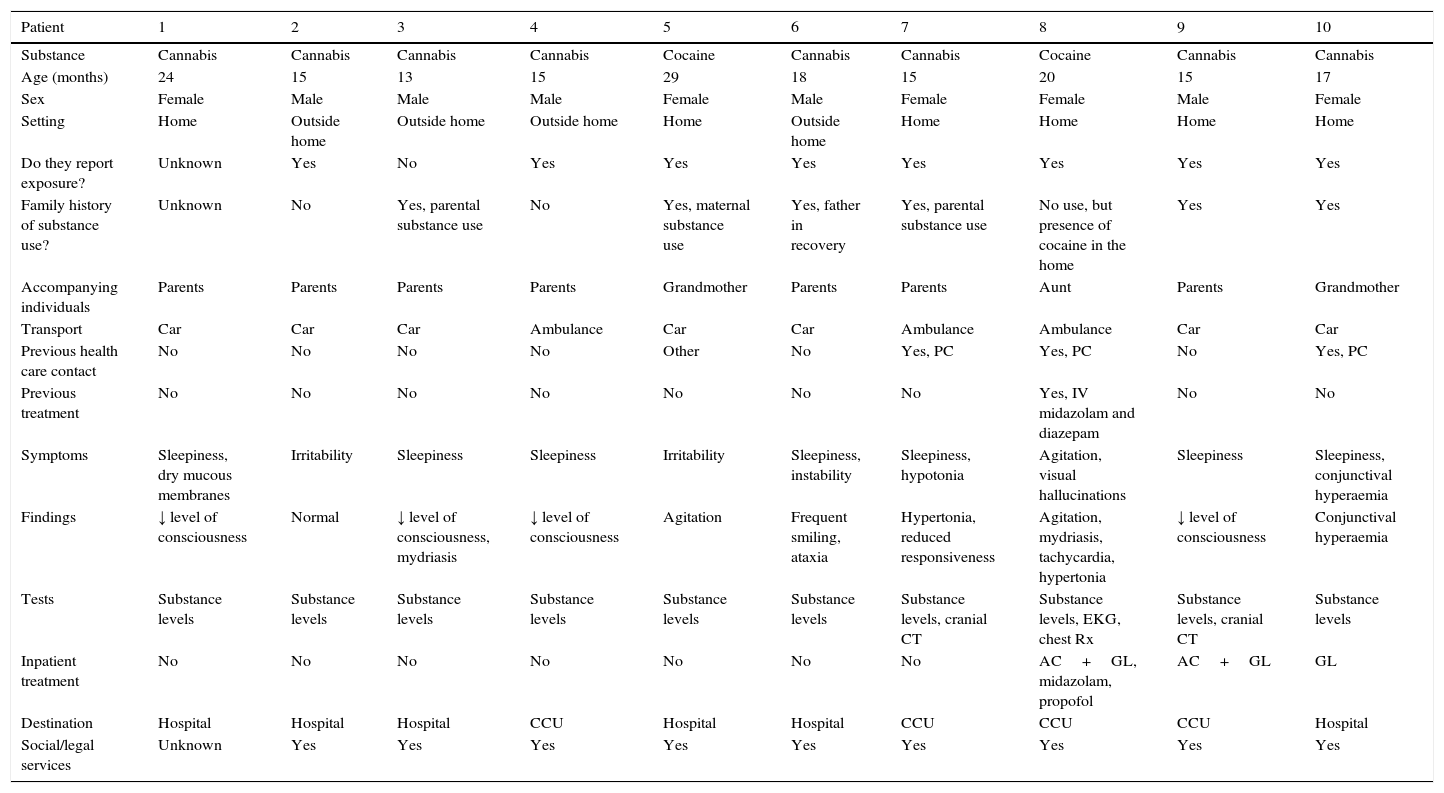
Table 1 summarises the characteristics of unintentional poisonings. The ten cases of unintentional poisoning in minors involved cannabis and cocaine, and the clinically significant manifestations consisted of central nervous system symptoms, as reported in the literature.4 There are studies in the literature that report that accompanying individuals fail to provide information regarding the exposure to the substance.5 However, in our case series this information was provided by a significant number, which facilitated the management of the child's presenting problem and prevented the performance of unnecessary tests. In three cases, ancillary tests other than those used for detecting the toxic substance were performed due to the severity of the clinical manifestations and/or to assess for potential complications. Management in the PEDs mainly consisted of supportive measures and/or gastrointestinal decontamination, in adherence with clinical practice guidelines.6 All of these patients were admitted to the hospital, and while the final outcome was good in all, 40% were initially admitted to critical care units. In addition, with the exception of one case in which this datum was not documented, local social services and legal authorities were notified in all cases.
Characteristics and management of patients with unintentional illegal drug poisoning.
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Substance | Cannabis | Cannabis | Cannabis | Cannabis | Cocaine | Cannabis | Cannabis | Cocaine | Cannabis | Cannabis |
| Age (months) | 24 | 15 | 13 | 15 | 29 | 18 | 15 | 20 | 15 | 17 |
| Sex | Female | Male | Male | Male | Female | Male | Female | Female | Male | Female |
| Setting | Home | Outside home | Outside home | Outside home | Home | Outside home | Home | Home | Home | Home |
| Do they report exposure? | Unknown | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Family history of substance use? | Unknown | No | Yes, parental substance use | No | Yes, maternal substance use | Yes, father in recovery | Yes, parental substance use | No use, but presence of cocaine in the home | Yes | Yes |
| Accompanying individuals | Parents | Parents | Parents | Parents | Grandmother | Parents | Parents | Aunt | Parents | Grandmother |
| Transport | Car | Car | Car | Ambulance | Car | Car | Ambulance | Ambulance | Car | Car |
| Previous health care contact | No | No | No | No | Other | No | Yes, PC | Yes, PC | No | Yes, PC |
| Previous treatment | No | No | No | No | No | No | No | Yes, IV midazolam and diazepam | No | No |
| Symptoms | Sleepiness, dry mucous membranes | Irritability | Sleepiness | Sleepiness | Irritability | Sleepiness, instability | Sleepiness, hypotonia | Agitation, visual hallucinations | Sleepiness | Sleepiness, conjunctival hyperaemia |
| Findings | ↓ level of consciousness | Normal | ↓ level of consciousness, mydriasis | ↓ level of consciousness | Agitation | Frequent smiling, ataxia | Hypertonia, reduced responsiveness | Agitation, mydriasis, tachycardia, hypertonia | ↓ level of consciousness | Conjunctival hyperaemia |
| Tests | Substance levels | Substance levels | Substance levels | Substance levels | Substance levels | Substance levels | Substance levels, cranial CT | Substance levels, EKG, chest Rx | Substance levels, cranial CT | Substance levels |
| Inpatient treatment | No | No | No | No | No | No | No | AC+GL, midazolam, propofol | AC+GL | GL |
| Destination | Hospital | Hospital | Hospital | CCU | Hospital | Hospital | CCU | CCU | CCU | Hospital |
| Social/legal services | Unknown | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
AC, activated charcoal; CCU, critical care unit; CT, axial computed tomography scan; EKG, electrocardiograph; GL, gastric lavage; PC, primary care; Rx, radiograph.
Based on this case series, nearly half of poisoning cases in Spanish PEDs involving illegal drugs as the only detected substances corresponded to young children, and usually involved cannabis. Although outcomes are generally good, these children are generally unstable on arrival at the PED and at times require treatment and follow-up care in critical care units.
We want to thank the Working Group on Poisonings of the Spanish Society of Paediatric Emergency Medicine (Sociedad Española de Urgencias de Pediatría) (Appendix A).
Hospital (H.) Alto Deba: Agustín Rodríguez; H. del Tajo, Aranjuez: Carlos García-Vao; H.U. Arnau de Vilanova, Lleida: Neus Pociello; H.U. Basurto: Javier Humayor; H. Cabueñes: Ramón Fernández; H. Regional de Málaga: Silvia Oliva Rodríguez-Pastor; Complejo (C.) Hospitalario de Jaén: Tomás del Campo; C. Asistencial Universitario de Léon: Ana Gloria Andrés; Corporación Sanitaria Parc Taulí, Sabadell: Mireia Pérez; Hospital Universitario (H.U.) Cruces: Santiago Mintegi, Paula Santiago, Nerea Bilbao; H.U. Doce de Octubre: Sofía Mesa; H.U. Donostia: José Angel Muñoz Bernal; H.U. Dr. Peset. Valencia: J. Rafael Bretón Martínez; H.U. Fuenlabrada: Rocío Rodríguez; H. Francesc de Borja de Gandía: Carlos Miguel Angelats; Fundació Sant Hospital de la Seu d’Urgell: Pablo Javier Ercoli; H. Universitario Fundación Alcorcón: Alberto Barasoain; H. General Universitario de Alicante: Olga Gómez Pérez; H.U. Gregorio Marañón: Paula Vázquez; H. Infanta Cristina, Parla, Madrid: Begoña de Miguel; H. Infanta Elena, Valdemoro: Carmen Gómez; H. de Terrassa: Judit Barrena; H. Laredo: Ana Jorda; H.U. Lucus Augusti: Sandra Yáñez; H. Mendaro: Laura Herrero; H.U. Mutua Terrassa: Elena May Llanas; H.U. Niño Jesús: Juan Carlos Molina; H. Materno-Infantil de Las Palmas de Gran Canaria: Lily Mangione; H. Materno-Infantil de Badajoz: Paz Hurtado; H. Ntra. Sra. de Sonsoles, Ávila: Helvia Benito; H. Montepríncipe, H. Sanchinarro, H. Torrelodones, Madrid: Silvina Natalini; H. Príncipe de Asturias, Alcalá de Henares: M. Ángeles García Herrero; H.U. Puerta de Hierro-Majadahonda: Consuelo Benito Caldés; H. Rey Juan Carlos: Pablo Bello Gutiérrez; H.U. San Agustín: Juan Cózar Olmo; H.U. Río Hortega, Valladolid: Roberto Velasco; H. Sant Joan de Déu, Xarxa Hospitalaria i Universitaria de Manresa, Fundació Althaia: Eva Botifoll García; H.U. Sant Joan de Déu: Lidia Martínez Sánchez; H. San Pedro: Laura Martínez; H. Miguel Servet: Carmen Campos Calleja; H.U. Son Espases, Palma de Mallorca: Victoria López Corominas; H. Son Llàtzer: Carmen Vidal Palacios; H.U. Central de Asturias, Oviedo: Julián Rodríguez; H. Universitario de Salamanca: Javier López Ávila; H.U. Virgen de la Arrixaca: Carlos Pérez; H. Virgen de la Salud, Toledo: Esther Crespo Rupérez; Complejo Hospitalario de Navarra: Miriam Palacios; H. Zumarraga: Amalia Pérez; H. Quirón, Bizkaia: Itziar Iturralde; H. Clínico U. Lozano Blesa: Gonzalo González García; H.U. Puerta del Mar, Cádiz: Arturo Hernández; H. Clínico U. de Valladolid: Elena Urbaneja Rodríguez; Complejo Asistencial de Segovia: H. General: Rebeca Garrote; H.U. y Politécnico La Fe de Valencia: Rafael Señer; Hospital de Mataró: Joaquim Martorell Aymerich; H.U. Marqués de Valdecilla: José Lorenzo Guerra; H. Sierrallana: José Lorenzo Guerra; H. Gernika-Lumo: Alicia Gutiérrez and Complexo Hospitalario Universitario de A Coruña: Alicia Herrera.
Please cite this article as: Azkunaga B, Crespo E, Oliva S, Humayor J, Mangione L. Intoxicaciones por droga ilegal en niños de corta edad en los servicios de urgencias pediátricos españoles. An Pediatr (Barc). 2017;86:47–49.