Constipation has classically been considered as a risk factor of enuresis, although there are increasingly more publications that report a similar prevalence of constipation in both enuretics and non-enuretics.
ObjectiveTo determine the influence of constipation in monosymptomatic and non-monosymptomatic enuresis, and to find out the prevalence of the three disorders, as well as the lower urinary tract dysfunction and bladder-bowel dysfunction in the population.
Material and methodA cross-sectional observational prevalence study on a representative population sample of 5–9 year-old school boys and girls of Galicia, Spain. A questionnaire was completed in the schools on urinary and bowel habits, which included questions from the Paediatric Lower Urinary Tract Scoring System (PLUTSS) diagnostic questionnaire and grading of the lower urinary tract dysfunctions. The enuresis was diagnosed using the International Children's Continence Society (ICSS), and if it was also associated with diurnal symptoms, it was also classified as non-monosymptomatic enuresis. The constipation was evaluated using the Rome III criteria and the adapted Bristol stool scale.
ResultsA total of 772 questionnaires were included in the study. The prevalence of constipation was 20% and that of enuresis was 9.1% (62.9% monosymptomatic enuresis and 37.1% non-monosymptomatic), with the prevalence of bladder-bowel dysfunction being 5.2%. It was observed that constipation had no influence on the presence of monosymptomatic enuresis, but it did have an influence on non-monosymptomatic enuresis and lower urinary tract dysfunctions, where it was a significant risk factor.
ConclusionsThe differential diagnosis between monosymptomatic and non-monosymptomatic enuresis is essential in the initial evaluation of the patient with enuresis, since the therapeutic management and the characteristics of both disorders are different, with constipation only being a risk factor in cases of non-monosymptomatic enuresis.
Clásicamente se ha considerado el estreñimiento como un factor de riesgo de la enuresis, aunque cada vez hay más publicaciones que reportan una prevalencia de estreñimiento similar en enuréticos y no enuréticos.
ObjetivoDeterminar la influencia del estreñimiento en la enuresis monosintomática y la no monosintomática y conocer la prevalencia de las 3 entidades así como de disfunciones del trato urinario inferior y disfunción vesicointestinal en la población.
Material y métodoEstudio observacional transversal de prevalencia sobre una muestra representativa de la población gallega de niños y niñas escolarizados de 5 a 9 años. Se realizó una encuesta en los colegios sobre hábitos miccionales e intestinales que incluía las preguntas del cuestionario Paediatric Lower Urinary Tract Scoring System (PLUTSS) de diagnóstico y graduación de las disfunciones del tracto urinario inferior. Se consideró la enuresis según los criterios de la Sociedad Internacional para la Continencia en Niños (ICSS), y si además asociaba sintomatología diurna, se clasificó como enuresis no monosintomática. El estreñimiento se valoró de acuerdo con los criterios Roma III y la escala de heces de Bristol adaptados.
ResultadosSe incluyeron 772 encuestas en el estudio. La prevalencia de estreñimiento fue del 20%, la de enuresis del 9,1% (enuresis monosintomática 62,9% y no monosintomática 37,1%) y la de disfunción vesicointestinal del 5,2%. Observamos que el estreñimiento no influye en la presencia de enuresis monosintomática, pero sí en la enuresis no monosintomática y las disfunciones del trato urinario inferior, donde constituye un importante factor de riesgo.
ConclusionesEs fundamental el diagnóstico diferencial entre enuresis monosintomática y no monosintomática en la valoración inicial de un paciente enurético, ya que el manejo terapéutico y las características de ambas entidades son diferentes, constituyendo el estreñimiento un factor de riesgo solamente en el caso de las enuresis no monosintomáticas.
The presence of constipation, faecal incontinence (FI) or both is defined as bowel dysfunction (BD). Constipation accounts for 3–5% of paediatric visits and 25% of paediatric gastroenterology visits.1 Children with gastrointestinal disease manifesting as constipation or FI often experience lower urinary tract (LUT) symptoms in association (22–34%).1,2 Thirty percent develop urinary incontinence and 10% urinary tract infections (UTIs).3–6 Even if they do not report symptoms, children with constipation have abnormal urine flow patterns.7
On the other hand, it is estimated that more than half of children with LUT dysfunction have associated BD; of these children, 30% present to the first visit with faecal impaction and 80% also present with FI secondary to faecal retention.5,8 Thus, the incidence of this association is high. In many cases, patients that visit the gastroenterologist for the first time on account of constipation present with the same symptoms as patients that visit the urologist for the first time due to LUT dysfunction.2
This association in children with no known neurological abnormalities is currently known as bladder and bowel dysfunction (BBD).9–12
The Paediatric Lower Urinary Tract Scoring System (PLUTSS) is a questionnaire developed for the purpose of diagnosing and establishing the severity of LUT dysfunction with a non-invasive approach and to monitor the response to treatment.10 A score of 8.5 or greater in the PLUTSS offers a sensitivity of 100% and a specificity of 95% in establishing the presence of LUT dysfunction.13
Faecal incontinence is defined as the involuntary passing of stools in an inappropriate setting at least once a month in children aged more than 4 years. It can be secondary to constipation or present in isolation. The form associated with constipation, caused by faecal overflowing, is the most prevalent (80%) and is known as retentive FI. The form that is not associated with constipation FI is less prevalent (20%) and is known as non-retentive FI.
The International Children's Continence Society (ICCS) recommends applying the Rome IV criteria for diagnosis of functional bowel disorders in children.3,14 Due to the importance of the evaluation and management of bowel movements in patients with LUT symptoms, in 2013 the ICCS published guidelines for the management of BD in patients with urinary symptoms.10
The anatomical proximity of both systems and their shared innervation facilitate that abnormalities in one system impact the other.15 The association of constipation and urinary tract disorders, such as urinary incontinence, urgency, increased frequency and recurrent UTIs, has been well documented for years. Broadly speaking, constipation can affect both bladder voiding and filling, as the mechanical compression exerted by the rectum full of faeces on the posterior wall of the bladder and the trigone decreases the capacity of the bladder, giving rise to urgency, incontinence and increased voiding urgency, but may also change the physiology and neural stimuli on the bladder and pelvic floor, which result in a progressive reduction in the urgency to urinate, detrusor overactivity, dysfunctional voiding and a significant increase in the post-void residual volume.2 The compression by the rectum of the trigone and bladder neck can result in obstruction of the lower urinary tract, which results in additional increases in the post-void residual and a risk of vesicoureteral reflux. On the other hand, the fullness of the rectum induces the contraction of external anal sphincter, which in turn inhibits the relaxation of the external urethral sphincter and the pelvic floor. This suggests that the anal and urethral sphincters are a functional unit with shared access to the sacral reflexes of the bowel, bladder and proximal urethra.13,16
Enuresis is defined as urinary incontinence during sleep starting from age 5 years with a minimum frequency of 4 times per month. Paediatric patients with LUT symptoms differ in terms of clinical presentation, pathogenesis and management from patients that do not have daytime symptoms, so it is important to differentiate between these 2 problems. Enuresis in absence of LUT symptoms and without bladder dysfunction is known as monosymptomatic enuresis (ME); children with both enuresis and LUT symptoms instead have nonmonosymptomatic enuresis (NME),9,11 which requires specific treatment different from that of monosymptomatic cases.
The aim of our study was to assess the impact of constipation on ME and NME and to establish the prevalence of these 3 disorders, LUT dysfunction and BBD in the population.
Material and methodsWe conducted an observational cross-sectional prevalence study. We studied a representative sample of male and female schoolchildren aged 5–9 years in the autonomous community of Galicia.
Based on population data reported by the Instituto Galego de Estadística, we calculated the sample size required for our study. We obtained a representative sample from each province by randomised sampling in towns stratified by size. In each town, we randomly selected public, private and privately owned publicly funded early childhood education and primary schools in both rural and urban settings using the Epidat software, version 3.1.
We submitted the questionnaire to the selected schools for their distribution in classes of different years. The questionnaires were filled out on a voluntary and anonymous basis, and we received a total of 3675 responses, of which we selected 772 in strict order of arrival, which allowed us to analyse the data with a precision of 3% and a 97% confidence level.
We designed a questionnaire (Appendix B) assessing urination and defecation patterns and specific symptoms of BBD that included the items on LUT symptoms of the PLUTSS. This questionnaire has been translated to Spanish and validated in this version by our research group.17 We distributed the questionnaires in the schools after obtaining permission from the corresponding administrations, accompanied by a sheet that provided information about the study to the parents, whom we asked to complete the questionnaire.
We defined constipation as fulfilment of 2 or more of the modified Rome III criteria, which were the current criteria used at the time of the study.14
We defined BD as presence of constipation, FI or both. We defined BBD as presence of BD in a child that also experienced urinary symptoms or had a positive PLUTSS result (score≥8.5).
We performed a descriptive study of the variables under study. We analysed the association between qualitative variables by means of the chi square test or the Fisher exact test. We compared the means in independent samples using the Student t test or the Mann–Whitney U test as applicable based on the results of the Kolmogorov–Smirnov test for normality. We assessed the association between quantitative variables with the Pearson or Spearman correlation coefficient depending on the distribution of the variables. Logistic regression models were fitted to determine which variables were independently associated with a positive PLUTSS, ME, NME, constipation and FI.
ResultsWe analysed 772 responses for children aged 5–9 years, 52.8% male and 47.2% female.
The prevalence of enuresis was 9.1%, with ME accounting for 62.9% of the cases and NME for the remaining 37.1% (Table 1).
Distribution of enuresis by sex.
| Female | Male | OR (ref: female) | CI | P | |
|---|---|---|---|---|---|
| n (%) | n (%) | ||||
| Enuresis | |||||
| Yes | 31 (7.6) | 39 (10.7) | 1.459 | (0.890–2.393) | .132 |
| No | 377 (92.4) | 325 (89.3) | |||
| ME | |||||
| Yes | 18 (4.4) | 26 (7.1) | 1.667 | (0.898–3.093) | .102 |
| No | 390 (95.6) | 338 (92.9) | |||
| NME | |||||
| Yes | 13 (3.2) | 13 (3.6) | 1.125 | (0.515–2.460) | .767 |
| No | 395 (96.8) | 351 (96.4) | |||
ME, monosymptomatic enuresis; NME, nonmonosymptomatic enuresis.
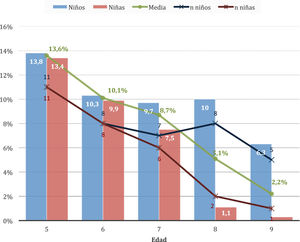
The prevalence of enuresis decreased with age, as can be seen in Fig. 1.
The prevalence of constipation was 20.0%, corresponding to a total of 154 children with the condition. Faecal incontinence was reported in 22 children for a prevalence of 2.8% in the case series; 60% of them only experienced staining of their underwear and 40% passed larger amounts of stool. Most of these children had retentive FI (2.1% of the total sample); and only 6 patients had non-retentive FI. Overall, 160 children (20.8%) had some form of BD, and most patients with FI had constipation. There were 40 children with BBD (5.2%). Both FI and BBD were more frequent in boys, a difference that was statistically significant (Table 2).
Distribution by sex of bowel dysfunction and bladder and bowel dysfunction.
| Female | Male | OR (ref: female) | CI | P | |
|---|---|---|---|---|---|
| n (%) | n (%) | ||||
| Constipation | |||||
| Yes | 86 (21.0) | 68 (19.0) | 0.879 | (0.651–1.187) | .222 |
| No | 322 (79.0) | 295 (81.0) | |||
| FI | |||||
| Yes | 7 (1.6) | 15 (4.0) | 2.506 | (1.137–5.523) | .019 |
| No | 401 (98.4) | 349 (96.0) | |||
| BD | |||||
| Yes | 86 (21.2) | 74 (20.3) | 0.947 | (0.704–1.273) | .717 |
| No | 322 (78.8) | 290 (79.7) | |||
| BBD | |||||
| Yes | 15 (3.7) | 25 (6.9) | 1.952 | (1.115–3.418) | .017 |
| No | 393 (96.3) | 339 (93.1) | |||
BBD, bladder and bowel dysfunction; BD, bowel dysfunction; FI, faecal incontinence.
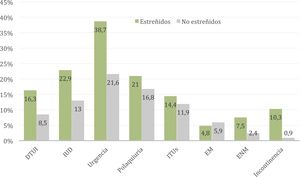
We conducted a bivariate analysis to determine which clinical signs were associated with the presence of constipation (Table 3). We found a significant association of constipation with the following variables: PLUTSS score, LUT dysfunction, daytime urinary incontinence (DUI), LUT symptoms, urinary urgency, urge incontinence, NME and FI.
Bivariate analysis of clinical features associated with the presence of constipation.
| With constipation (mean±SD) | Without constipation (mean±SD) | P | |
|---|---|---|---|
| PLUTSS | 4.8±4.3 | 2.7±3.2 | <.001 |
| With constipation | Without constipation | OR | IC | P | |
|---|---|---|---|---|---|
| n (%) | n (%) | ||||
| LUTD | |||||
| Yes | 25 (16.3) | 52 (8.5) | 2.095 | (1.356–3.234) | .001 |
| No | 129 (83.7) | 566 (91.5) | |||
| DUI | |||||
| Yes | 35 (22.9) | 80 (13.0) | 1.990 | (1.367–2.899) | <.001 |
| No | 119 (77.1) | 538 (87.0) | |||
| Daytime urinary symptoms | |||||
| Yes | 104 (67.8) | 295 (47.7) | 2.302 | (1.678–3.160) | <.001 |
| No | 50 (32.2) | 323 (52.3) | |||
| Urinary urgency | |||||
| Yes | 60 (38.7) | 133 (21.6) | 2.295 | (1.667–2.899) | <.001 |
| No | 94 (61.3) | 485 (78.4) | |||
| Polyuria | |||||
| Yes | 32 (21.0) | 104 (16.8) | 1.315 | (0.904–1.912) | .151 |
| No | 122 (79.0) | 514 (83.2) | |||
| Painful urination | |||||
| Yes | 1 (0.5) | 4 (0.6) | 0.798 | (0.093–6.867) | .655 |
| No | 153 (99.5) | 614 (99.4) | |||
| Urinary hesitancy | |||||
| Yes | 7 (4.7) | 22 (3.6) | 1.303 | (0.628–2.701) | .476 |
| No | 147 (95.3) | 596 (96.4) | |||
| Urge incontinence | |||||
| Yes | 17 (11.2) | 29 (4.7) | 2.508 | (1.479–4.252) | <.001 |
| No | 137 (88.8) | 589 (95.3) | |||
| Increased urinary urgency | |||||
| Yes | 6 (4.2) | 16 (2.6) | 1.662 | (0.754–3.664) | .203 |
| No | 148 (95.8) | 602 (97.4) | |||
| UTI | |||||
| Yes | 22 (14.4) | 74 (11.9) | 1.251 | (0.811–1.929) | .311 |
| No | 132 (85.6) | 544 (88.1) | |||
| Enuresis | |||||
| Yes | 19 (12.2) | 52 (8.3) | 1.538 | (0.870–2.716) | .136 |
| No | 135 (87.8) | 566 (91.7) | |||
| ME | |||||
| Yes | 7 (4.8) | 37 (5.9) | 0.795 | (0.347–1.820) | .586 |
| No | 147 (95.2) | 581 (94.1) | |||
| NME | |||||
| Yes | 11 (7.5) | 15 (2.4) | 3.289 | (1.478–7.320) | .005 |
| No | 136 (92.5) | 603 (97.6) | |||
| FI | |||||
| Yes | 16 (10.3) | 6 (0.9) | 12.132 | (5.321–27.661) | <.001 |
| No | 138 (89.7) | 612 (99.1) | |||
DUI: daytime urinary incontinence; FI, faecal incontinence; LUTD, lower urinary tract dysfunction; ME, monosymptomatic enuresis; NME: nonmonosymptomatic enuresis; PLUTSS, Paediatric Lower Urinary Tract Scoring System; UTI, urinary tract infection.
Fig. 2 presents the most relevant results of Table 3. It is apparent that the prevalence of all LUT symptoms or disorders is greater in patients with constipation with the exception of ME, which is the only disorder under study that is not associated with LUT dysfunction.
DiscussionBladder and bowel dysfunction encompasses a broad spectrum of disorders, including abnormal urination or defecation patterns.18 The ICCS defines the presence of LUT dysfunction from age 5 years, as bladder control is expected to have been achieved by this age.10 Similarly, enuresis may be considered in a patient from age 5 years.10 In contrast, the ICCS defines BD from age 4 years.10,11
To determine the prevalence of functional bowel and bladder disorders, most epidemiological studies analyse the frequency of daytime urinary incontinence and especially enuresis, and, in some cases, they analyse the presence of LUT symptoms according to varying criteria, rarely using validated questionnaires to assess the severity of urinary symptoms to establish the criteria for the definition of LUT dysfunction. Intestinal disorders are most frequently analysed based on the Rome III criteria (in many cases, modified criteria) or different criteria defined in the context of the study.
The PLUTSS questionnaire is an instrument used for diagnosis and follow-up of patients with LUT dysfunction. Since 2017, this questionnaire has been translated and culturally adapted to Spanish, so we recommend its use in the assessment of patients with LUT symptoms, which would make it possible to compare data across series and studies.17
The prevalence of enuresis in our study was 9.1%, 5.7% corresponding to ME and 3.4% to NME. Age is an important factor in the prevalence of enuresis. Fig. 1 presents the prevalence by sex and age in our sample, evincing a decrease with increasing age, which was in strong agreement with previous studies in different populations,19–21 with a prevalence of about 14% at 5 years gradually decreasing to 2% by age 9 years.
Enuresis is more frequent in male individuals,20,22–25 as observed in our study, with a greater risk of enuresis in boys (OR=1.72), especially of ME (OR=1.91). We found a stronger association compared to the association reported in other cultures, for example, in studies by Ozkan et al.20 (OR=1.60) or Esezobor et al.25 (OR=1.56), but lower compared to studies conducted in Spain in similar populations, like the one conducted by Martínez Agulló et al.23 (OR=2.34) or the one by Gutiérrez et al.22 (OR=2.52), although the latter highlighted that the difference between the sexes narrows with increasing age. In our case series, we found a much higher frequency of resolution at age 8–9 years in girls, so that differences in prevalence based on sex were significant once again (8.2% in boys vs 0.7% in girls); this difference is likely related to the earlier maturation of girls compared to boys.
The prevalence of constipation was 20.0%, equal to the percentage reported in the recent study on the epidemiology of constipation by Fujitani et al.26 A study similar to ours conducted in Korea by Chung et al.27 in a sample of 19,240 children aged 5–13 years used less stringent criteria, defining constipation as fewer than 3 bowel movements per week or Bristol stool types I or II, but found a similar prevalence of constipation (18.5%). Our findings are also similar to those of Loening-Baucke1 (22.6%), who applied the Iowa criteria (similar to the Rome III criteria). A systematic review covering a period of 11 years published in 2018 reported a prevalence of constipation ranging from 0.5% to 32.2%, with a mean prevalence of 9.5% (95% confidence interval [CI], 7.5–12.1%), in 35 studies that applied the Rome III or IV criteria.28 We ought to note that a high percentage of the studies included in this review were conducted in Asia (46%), with only 2 conduced in Europe and another 2 in North America, and that it is in the latter region where the prevalence of constipation was found to be highest.
In our series, we found an overall incidence of FI of 2.8%; the prevalence was practically the same as the prevalence reported in other studies.1 The prevalence of FI ranges from 0.8 to 4.1% in Western countries29,30 and from 2% to 7.8%27,31 in Asian countries. A study in the Netherlands described a greater risk in children aged 5–6 years (4.1%) compared to children aged 11–12 years (1.6%), which suggests that maturation may play a role in this difference30; the authors also found an increased risk of psychiatric disorders, in spite of which only 27–37% sought medical care for the BD. The ICCS recommends conducting a mental health and/or psychiatric assessment in the initial evaluation of all children with non-retentive FI on account of the high prevalence of psychiatric comorbidities found in this subset of patients. In our series, constipation was the main risk factor for FI (OR=11.249), but we identified other predisposing factors: male sex (OR=2.407), enrolment in school before achievement of full bladder control (OR=3.609) and presence of LUT dysfunction (OR=3.271).
We found the association of bladder and bowel dysfunction in 5.2% of cases in our study, with a higher frequency in boys (OR=1.952). We found that 75% of cases of BBD corresponded to children with voiding postponement, that is, who delayed urination and/or defecation. We applied stringent criteria for the definition of BBD, which required a positive PLUTSS score and presence of constipation or FI.
Classically, constipation has been considered a risk factor for enuresis, but one of the main studies in the literature in support of this hypothesis was conducted in only 30 children with enuresis,32 too small a case series to draw firm conclusions on specific clinical and pathophysiological features. A growing number of studies have failed to find this association and report a similar prevalence of constipation in children with and without enuresis.24,33 Our study did not detect statistically significant differences either; especially when considering children with ME alone, as we found that the prevalence of ME was lower in children with constipation than in children without (4.8% vs 5.9%). The proportion of children with NME that had constipation was significantly greater compared to the rest of the children in the case series (NME, 36.5% vs no NME, 19.2%; OR=1.9).
In our series, in opposition to ME, LUT dysfunction and NME were clearly associated with constipation, which led us to conclude that the association between ME and constipation previously postulated in the literature does not exist and may have been perceived due to the lack of clear discrimination between ME and NME, as the association with the latter is indeed frequent. Thus, constipation is not a risk factor for ME, but is a risk factor for LUT dysfunction and therefore for NME, too.
In our series, we observed an association between the presence of constipation and the score in the PLUTSS (R2=0.088), as previously described in the study by Loening-Baucke.1 We also found that the presence of constipation was associated with an increased risk of LUT symptoms (OR=1.523), urinary urgency (OR=2.295) and especially FI (OR=12.132). All these symptoms are probably secondary to incomplete rectal or vesical voiding and the resulting contraction of the pelvic floor to avoid them. Potential explanations of this association between constipation and LUT dysfunction have focused on the anatomical proximity of the rectum and bladder, the shared innervation at the level of the sacrum and CNS neural centres and the contraction of the striated muscle adjacent to both structures and used in holding or postponing voiding of urine or faeces, which could account for the significant relationship between these manoeuvres and the risk of bladder or bowel dysfunction.15
ConclusionsThe differential diagnosis of ME and NME is essential in the initial evaluation of patients with enuresis. Constipation is not associated with the prevalence of ME, but it is a significant risk factor for LUT dysfunction and NME.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Rodríguez-Ruiz M, Mendez-Gallart R, García Mérida M, Somoza-Argibay I. Influencia del estreñimiento en la enuresis. An Pediatr (Barc). 2021;95:108–115.