Nocturnal enuresis (NE) is a common disorder that affects both children and their families. The objective is to determine its prevalence in an extensive sample of children considering different diagnostic criteria.
Patients and methodsCross-sectional descriptive study using a survey of parents of a selection of primary and secondary school Asturian children (6, 10 and 13 years). The questionnaire consisted of 80 or 55 questions (10 of which were answered by the children) for those who urinated or not in bed, respectively. NE was registered as primary or secondary, and the presence or not of enuresis as the only symptom. In addition, the prevalence was compared according to the different diagnostic criteria.
ResultsOf the 3548 questionnaires distributed, 56.6% were answered completed correctly. A total of 102 children urinated in bed (5.52%), which corresponds to a prevalence of 2.82% according to the DSM-IV-TR/5 and the (International Continence Society) ICC, 3.7% with the DSM-III and ICD-10. It was more frequent in boys than in girls (2.8:1), with a predominance of primary forms (81.2%), and non-monosymptomatic (68.66%). The spontaneous resolution in the older age group was higher in boys than in girls, with the different prevalences of previous ages being equal to 13 years.
ConclusionsThe prevalence of NE in the studied region coincides with that observed in some other studies. There are differences according to the criteria used, which should draw attention to the need to unify the methodology of the studies and the criteria used in its diagnosis.
La enuresis nocturna (EN) es un trastorno frecuente que afecta tanto a los niños como a sus familias. El objetivo es determinar la prevalencia en una extensa muestra de niños considerando diferentes criterios diagnósticos.
Pacientes y métodosEstudio descriptivo transversal mediante encuesta a padres de niños asturianos seleccionados aleatoriamente entre los escolares de enseñanza primaria y secundaria (6, 10 y 13 años). El cuestionario constaba de 80/55 preguntas para los que se orinasen o no en la cama, respectivamente; 10 fueron respondidas por los niños. Se registró la EN como primaria o secundaria y la presencia o no de enuresis como único síntoma. Además, comparamos la prevalencia según los diferentes criterios diagnósticos.
ResultadosDe los 3548 cuestionarios distribuidos fueron respondidos correctamente el 56,6%. 102 escolares se orinaban en la cama (5,52%), lo que corresponde a una prevalencia del 2,82% según el DSM-IV-TR/5 y la ICCS, 3,7% con el DSM-III y CIE-10. Fue más frecuente en niños que en niñas (2,8:1), con gran predominio de las formas primarias (81,2%) y no monosintomáticas (68,66%). La resolución espontánea en el grupo de mayor edad es superior en niños que en niñas, igualándose a los 13 años las diferentes prevalencias de edades previas.
ConclusionesLa prevalencia de la EN en nuestra región coincide con la observada en algunos estudios. Existen diferencias según los criterios utilizados, lo que debe llamar la atención sobre la necesidad de unificar la metodología de los estudios y los criterios utilizados en su diagnóstico.
Nocturnal enuresis (NE) is a common childhood disorder that is usually associated with psychological symptoms and has an impact on the social, academic and family life of the child.1 The prevalence reported by published case series focused on the diagnosis of NE varies widely (from 2.3% to 25%),2–4 which can be explained by disparities in the inclusion criteria applied. The fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV and DSM-IV-TR)5 defined it as involuntary or intentional voiding of urine in bed at least twice a week in children aged more than 5 years, having ruled out congenital or acquired diseases of the central nervous system. This definition is maintained in the DSM-56 and is stricter in the severity required for diagnosis compared to previous editions (DSM-III and DSM-III-TR),7 which considered more than 1 episode a month abnormal and allowed the diagnosis from age 6 years. The 10th revision of the International Classification of Diseases (ICD-10) of the World Health Organization (WHO)8 also maintains the frequency of at least 1 episode per month for more than 3 months in children aged more than 5 years. On the other hand, the International Children’s Continence Society (ICCS)9 defines enuresis as incontinence while asleep at a “socially unacceptable” age with a frequency of more than 1 episode per month and sets age 5 years as the limit of normal. When it comes to the subtypes of NE, the DSM III-TR7 a previous period of 12 months of nocturnal dryness to define secondary enuresis, while the DSM IV-TR5 and DSM-56 and the ICD-108 do not establish a specific length for that period and the ICCS9 and most clinical practice guidelines require a period of at least 6 months. The DSM III-TR,7 DSM-IV-TR5 and ICD-108 do not differentiate between monosymptomatic and nonmonosymptomatic enuresis, while the DSM-56 and ICCS9 consider NE nonmonosymptomatic when there is evidence of concomitant lower urinary tract dysfunction.
This lack of consensus is an important limitation when it comes to analysing different studies and comparing their findings.10 In addition to applying the same major diagnostic criteria, prevalence studies should collect data on the sex of patients and the classification of NE as primary (PNE) or secondary (SNE).2,11 There is substantial variation in the age of acquisition of bladder control, which ranges between age 2 and 6 years10 and is generally achieved earlier in girls compared to boys.7 Most epidemiological studies do not distinguish between primary and secondary forms of enuresis or cases of monosymptomatic enuresis (MSE) versus nonmonosymptomatic enuresis (NMSE). Previous studies also often have samples that are too small to obtain findings with sufficient statistical power. Another interesting aspect is the proportion of cases that resolve spontaneously with age, which also varies between studies.
There is broad agreement that questionnaires completed by parents are an adequate source for data regarding nocturnal episodes, although they may not be adequate for assessment of daytime manifestations. The prevalence of mental health problems reported by parents is consistent with the reports of children themselves,12 but the children or their teachers should also be involved in the evaluation.
The aim of our study was to compare the different definitions and estimate the proportion of children with NE at ages 6, 10 and 13 years and to attempt to define the profile of cases with spontaneous resolution.
Sample and methodsWe performed a cross-sectional descriptive study by means of an anonymous questionnaire completed by parents of children enrolled in years 2 and 4 of primary education and year 1 of compulsory secondary education in Asturias, Spain. The sampling frame was the list of schools in the Principality of Asturias provided by the Directorate General of Planning, Centres and Resources of the Department of Education and Science. The sample was selected by multistage sampling, selecting schools in a first stage and classrooms in a second stage, selecting every student in the selected classrooms to participate in the survey. We calculated the necessary sample size (n = 3600) to achieve a precision of 1.1% with a 95% confidence level for an expected proportion of 6% and assuming losses to follow-up of 18%.
The parents of selected students received the questionnaire and were asked to complete it and submit it to the classroom teacher the following week. The questionnaire consisted of 80 items in case of children with NE and 55 in case of children that stayed dry through the night. It included a series of questions that parents had to ask their children directly to obtain information on daytime symptoms and how they perceived the problem. We used one filter question, “Does your child void urine during sleep?”, to classify children as having or not having enuresis. Most items were closed-ended dichotomous or multiple choice questions. The survey, which was part of a broader study, can be found in the following link: Encuesta Enuresis Asturias. For the study presented here, we used the items regarding age and sex, presence and frequency of nocturnal unintentional voiding, previous history of nocturnal dryness lasting more than 6 months, daytime urinary signs or symptoms, upper airway obstruction symptoms and constipation/encopresis.
Due to the lack of validated questionnaires and the disparities in the criteria used for the definition of NE, we chose to develop a custom questionnaire, which we tested in a pilot study in 4 schools of Oviedo and Gijón that, based on information from the Department of Education, served populations of low socioeconomic status. The goal of the pilot study was to assess the comprehension of all questionnaire items, the level of difficulty of the questionnaire and the time required for completion, and to ensure readiness to perform the survey using the questionnaire.
The primary outcome was the presence of enuresis based on the DSM-IV-TR/DSM-5 diagnostic criteria (age ≥ 5 years and at least 2 episodes of bedwetting a week). Based on the ICCS criteria, we classified cases into 2 subtypes: secondary (SNE) if NE had been preceded by a period of nocturnal dryness lasting at least 6 months, and primary (PNE) otherwise. We also classified cases into the nonmonosymptomatic (NMSE) and monosymptomatic (MSE) subtypes based on whether NE was associated with daytime manifestations of lower urinary tract dysfunction or occurred in isolation, respectively.
In addition, we considered the diagnosis of enuresis in the sample using older criteria, like the DSM-III-TR, or current criteria differing on the frequency of episodes, such like the ICCS criteria. We also considered NMSE presenting not only with daytime symptoms of lower urinary tract dysfunction but also with 2 clinical features typically found in these patients, constipation/encopresis and symptoms of upper airway obstruction. We defined the latter feature as parents answering “yes” to all items regarding apnoea or snoring during sleep, daytime somnolence, waking up tired and history of tonsillar or lymph node hypertrophy. We excluded questionnaires submitted outside the established time window, completed incorrectly or for children aged less than 5 years or with chronic cardiovascular, urological or renal disease that could result in impaired bladder control.
We entered the data in an electronic database and processed them with the statistical software R, version 3.4.4 (http://cran.r-project.org/). All variables under study were qualitative and summarised as absolute frequencies and percentages.
The study was authorised by the Fiscalía de Menores (child welfare and prosecution office) and approved by the Research Ethics Committee of Asturias.
ResultsPilot study: of the 100 distributed questionnaires, 82 were submitted after completion, and we excluded 3 due to incomplete data. The time it took to complete the questionnaire ranged from 2 to 30 min (mean, 8 min). Only 3 parents considered that the difficulty was “average”, and parents singled out 6 terms that were “difficult to understand”, of which we replaced one for a more commonly used term because it had been marked as difficult by 3 respondents.
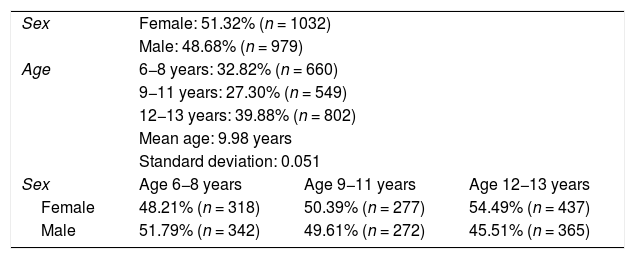
We selected 47 schools for participation in the study. We distributed a total of 3548 questionnaires and collected 2011 (56.6%) that had been completed correctly. Most respondents were mothers (85.3%), followed in frequency by fathers (11.5%), another caregiver of the child (1.8%) and a minority was filled out by both parents (0.9%). The sample included children aged 6–13 years (mean, 9.9 ± 0.05) and 51.3% were female. Table 1 summarises the characteristics of the sample.
Distribution of the sample by age and sex.
| Sex | Female: 51.32% (n = 1032) | ||
| Male: 48.68% (n = 979) | |||
| Age | 6−8 years: 32.82% (n = 660) | ||
| 9−11 years: 27.30% (n = 549) | |||
| 12−13 years: 39.88% (n = 802) | |||
| Mean age: 9.98 years | |||
| Standard deviation: 0.051 | |||
| Sex | Age 6−8 years | Age 9−11 years | Age 12−13 years |
| Female | 48.21% (n = 318) | 50.39% (n = 277) | 54.49% (n = 437) |
| Male | 51.79% (n = 342) | 49.61% (n = 272) | 45.51% (n = 365) |
Total sample, N = 2011.
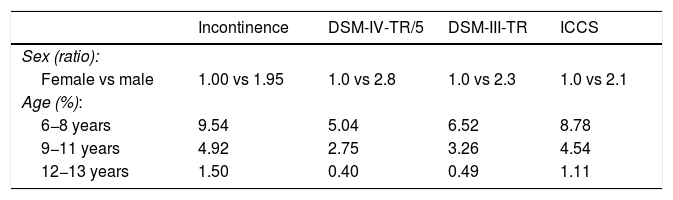
A total of 102 parents reported that their children experienced involuntary urination during the night (prevalence of involuntary urination at night of 5.5%). When we analysed the frequency of NE based on the different diagnostic criteria, we found that the prevalence decreased to 2.8% applying the DSM-IV-TR/DSM-5 criteria (n = 51) compared to 3.7% with the DSM-III-TR criteria (n = 67) or 5.0% with the ICCS criteria (n = 92). Applying the case definitions of other societies that share similar criteria we find overlapping prevalence values, as occurs with the ICD-10 and the ICCS criteria.
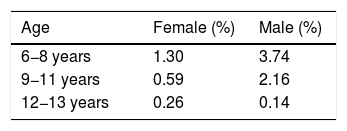
Independently of the diagnostic criteria applied, the prevalence was greater in boys compared to girls (2.8−1.9 vs 1) and decreased with age, with a prevalence of enuresis of 5.0%–9.5% in children aged 6–8 years compared to 0.4%–1.5% in children aged 12–13 years, depending on the applied definition (Table 2). Using the DSM-IV-TR/DSM-5 criteria, the decrease was quicker in girls in the early years (Table 3), without significant differences in the older age group (0.1% vs 0.3%, respectively).
Distribution of enuresis by age and sex based on different diagnostic criteria.
| Incontinence | DSM-IV-TR/5 | DSM-III-TR | ICCS | |
|---|---|---|---|---|
| Sex (ratio): | ||||
| Female vs male | 1.00 vs 1.95 | 1.0 vs 2.8 | 1.0 vs 2.3 | 1.0 vs 2.1 |
| Age (%): | ||||
| 6−8 years | 9.54 | 5.04 | 6.52 | 8.78 |
| 9−11 years | 4.92 | 2.75 | 3.26 | 4.54 |
| 12−13 years | 1.50 | 0.40 | 0.49 | 1.11 |
DSM-III-TR, Diagnostic and Statistical Manual of Mental Disorders, third edition, text revision; DSM-IV-TR/5, Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision and fifth edition; ICCS, International Children’s Continence Society.
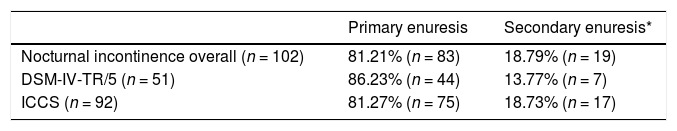
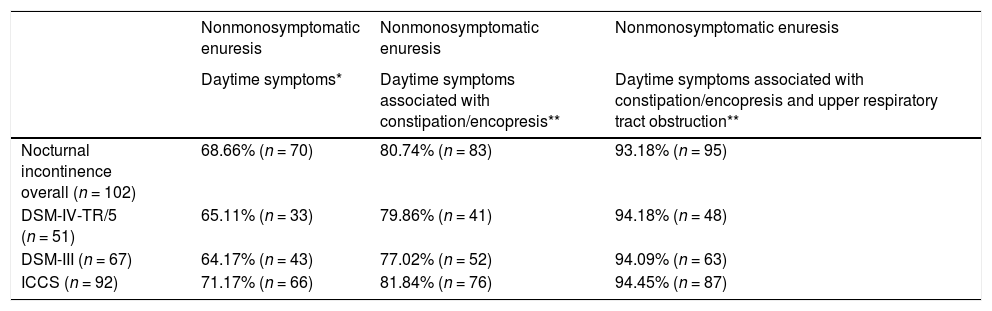
Most of the children had PNE (Table 4), regardless of whether the DSM IV-TR/DSM-5 or ICCS criteria were applied. This was also the case when we classified cases into the monosymptomatic or nonmonosymptomatic subtypes, with the latter being the most frequent form found in our sample either using the aforementioned criteria for enuresis or applied the definition of NMSE of the ICCS and DSM-5 (NE associated with daytime symptoms of lower urinary tract dysfunction) or other criteria proposed in the literature requiring the presence of manifestations of constipation/encopresis and signs of upper respiratory tract obstruction (Table 5).
Distribution of children with enuresis based on the diagnosis criteria for nocturnal enuresis classified into primary and secondary enuresis (n and %).
| Primary enuresis | Secondary enuresis* | |
|---|---|---|
| Nocturnal incontinence overall (n = 102) | 81.21% (n = 83) | 18.79% (n = 19) |
| DSM-IV-TR/5 (n = 51) | 86.23% (n = 44) | 13.77% (n = 7) |
| ICCS (n = 92) | 81.27% (n = 75) | 18.73% (n = 17) |
DSM-IV-TR/5, Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision and fifth edition; ICCS, International Children's Continence Society.
Distribution of children with enuresis (n and %) based on the diagnosis criteria for nocturnal enuresis and classification as nonmonosymptomatic enuresis based on the application of 3 commonly accepted clinical features.
| Nonmonosymptomatic enuresis | Nonmonosymptomatic enuresis | Nonmonosymptomatic enuresis | |
|---|---|---|---|
| Daytime symptoms* | Daytime symptoms associated with constipation/encopresis** | Daytime symptoms associated with constipation/encopresis and upper respiratory tract obstruction** | |
| Nocturnal incontinence overall (n = 102) | 68.66% (n = 70) | 80.74% (n = 83) | 93.18% (n = 95) |
| DSM-IV-TR/5 (n = 51) | 65.11% (n = 33) | 79.86% (n = 41) | 94.18% (n = 48) |
| DSM-III (n = 67) | 64.17% (n = 43) | 77.02% (n = 52) | 94.09% (n = 63) |
| ICCS (n = 92) | 71.17% (n = 66) | 81.84% (n = 76) | 94.45% (n = 87) |
DSM-III-TR, Diagnostic and Statistical Manual of Mental Disorders, third edition, text revision; DSM-IV-TR/5, Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision and fifth edition; ICCS, International Children's Continence Society.
Nocturnal enuresis is a frequent disorder in childhood and is an example of a disease with a widely heterogeneous clinical management13 and that clinicians are poorly trained to evaluate and manage.13 This has a serious impact on children and their families in terms of complications and costs.14 At the primary care level, empirical management with a “trial and error” approach is generally the norm, which entails a prolonged follow-up and is associated with a greater level of frustration in families and clinicians alike. It may also have a negative impact on the mental health of the child, whereas a rational treatment plan would yield a higher success rate and faster results.15
There are reports on the prevalence of NE in different paediatric populations. We found three major studies in Spain. One was carried out in the province of Leon and analysed associated factors,16 the prevalence and maturational sequence of nocturnal bladder control17 and the differences between PNE and SNE18; another was conducted in Valencia19 and aimed at establishing the prevalence in primary education students and involved risk factors, and another one was conducted in Tenerife.20
In the research published at the global level, different questionnaires have been used that are neither validated nor standardised and that frequently are not featured in the publications. Most of these questionnaires were used without prior performance of a pilot study. As for the methodology of the field work, in many instances it has not been described in enough detail to be reproduced, and some authors do not specify whether the respondents are the parents or the children themselves. We obtained valid responses from a large percentage of students (56%) due to the use of a complex but useful distribution and collection procedure with the contribution of teaching staff. Some of the potential weaknesses of our study are the reliability of the parents and recall bias, although the study of controls suggests that these sources of bias are of limited importance. The use of a control group for comparison with cases has also not been described or included in the analysis in most previous studies, so it is fair to assume that it did not take place. We also ought to highlight that some of the most recent studies on the prevalence of enuresis or associated factors did not include information on the frequency with which enuresis was considered pathological21–23 or the starting age for the definition of enuresis,4,24,25 while 2 of the studies considered nocturnal voiding pathological from age 4 years.21,26
In the sample under study, we found that 5.52% of children experienced involuntary urination while asleep. The prevalence of NE varies between countries, with higher values ranging from more than 25% in children in the Dominican Republic27 to 50% in children in Jamaica.28 The reported prevalence in Finland (8.2%)29 or Bangkok (3.9%)30 was closer to the one found in our study. In the sample of 8242 children of the Avon Longitudinal Study of Parents and Children (ALSPAC) in the United Kingdom, the estimated prevalence of enuresis, defined as 2 or more episodes of unintentional urination per week, was 2.6% at age 7 years and 15.5% in children under 2 years, with a predominance of the male sex.2 The proportion of cases of secondary enuresis in our sample was consistent with most of the previous literature,1,3,17–19,31–34 unlike the proportion of the nonmonosymptomatic subtype, which was higher in our sample, as occurred in a multicentre study conducted in Italy.32 These large differences could be attributed to studies selecting children from either the general population or specific groups, differences in sample size and disparities in the criteria and age limits applied to the definition of NE. For instance, we noticed that studies that applied the ICD-10 criteria found higher proportions.31,35 All of these factors decrease the validity of research conclusions, and this lack of homogeneity precludes comparison with the results of other studies.
In the sample under study, the prevalence of NE was higher in boys compared to girls regardless of the applied definition, with a ratio of nearly 3:1 (2.8:1) using the DSM-IV-TR/DSM-5 criteria. A possible explanation is that the maturation sequence involved in sphincter control is quicker in girls. Our findings were consistent with most of the reviewed literature.21,32 There is considerable variability in studies that applied the DSM-IV criteira3,21,32 with ratios ranging from 1.3:1 to 3.5:1. These differences between sexes disappear over time.19,25,33 A study conducted in Italy33 found a 2:1 ration in the group aged 13–14 years that dropped to 0.7:1 in the group aged more than 17 years, and another study in Italy32 found ratios of 2:1 at age 7 years and 1:1 at age 13 years. Our study corroborated this difference in the temporal trends in the prevalence of NE based on sex, as we observed a 2.8:1 ratio in the 6-to-8 years group that decreased gradually to 0.5:1 in the group aged more than 12 years.
A more relevant aspect is the development of bladder control and the persistence of NE. In our study we found a higher frequency of NE in younger children that decreased with age. Applying the DSM-IV-TR/DSM-5 criteria, the prevalence was 5.0% in children aged 6–8 years compared to 0.4% in children aged more than 12 years, although the trend remained regardless of the criteria used to define NE (Table 2). Many recent studies have obtained similar results.3,23,34,36 Data from other countries also reveal frequencies that decrease from approximately 9.7% at age 7 years to 5.5% at age 10, which confirms the presence in diverse settings of factors that delay the development of nocturnal bladder control in some children.37 This leads most parents to believe that their children will stop wetting themselves in bed eventually without intervention. However, new statistical analyses of data obtained in two historic cohorts in the United Kingdom (one from 1946 including n = 4755 children and the ALSPAC 1991-G2 cohort including n = 10 818) revealed that 34% of children that had NE at age 4 years continued to have enuresis at age 1538 and that 41% of children without nocturnal bladder control at age 4 years continued to have NE at 9.5 years.39 In addition, in the latter cohort, in children that had MSE or NMSE at age 9.5 years, the probability of having NE at age 14 years (n = 5899) were 3.5% and 23%, respectively. Also, some authors consider that in case of severe NE (episodes more than 5 nights a week), the probability of spontaneous resolution before adulthood is as small as 50%, compared to 90% in case of mild to moderate enuresis.40 Thus, it is not absolutely guaranteed that enuresis in a child will resolve, and the presence of urinary tract manifestations and the severity of enuresis are the most reliable predictors of the lack of an eventual spontaneous resolution.
In short, we conclude that the heterogeneity of the studied populations and collected data significantly distorts any interpretation of NE and related aspects that may be attempted. The standardization of criteria and the investigation of biopsychosocial determinants of NE should be pursued to improve care and treatment outcomes. Although this lack of a consensus has been discussed for decades,10 we still face the challenge today to achieve it along with its widespread implementation.
FundingThis research project was funded through one of the grants for clinical and epidemiological research in paediatrics given by the Fundación Ernesto Sánchez Villares(Project no. 05/2008).
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Taborga Díaz E, Martínez Suárez V, Alcántara-Canabal L, Suárez Castañón C, Cebrián Muíños C. Valoración de los criterios diagnósticos de la enuresis nocturna. An Pediatr (Barc). 2021;95:101–107.