The low FODMAP diet (fermentable oligosaccharides, monosaccharides, disaccharides, and polyols) has shown to be effective in adult patients with irritable bowel syndrome, but there are few studies on paediatric patients. The aim of this study is to assess the implementation and the outcomes of a low FODMAP diet in the treatment of functional abdominal pain in children from a Mediterranean area.
Material and methodsA table was designed in which foods were classified according to their FODMAP content, as well as a ‘Symptoms and Stools Diary’. A prospective study was conducted on children with functional abdominal pain in our Paediatric Gastroenterology Unit.
ResultsA total of 22 patients were enrolled in the trial, and 20 completed it. Data were collected of the abdominal pain features over a period of 3 days, and then patients followed a two-week low FODMAP diet. Afterwards, information about abdominal pain features was collected again. After the diet, they showed fewer daily abdominal pain episodes compared to baseline (1.16 [IQR: 0.41–3.33] versus 2 [IQR: 1.33–6.33] daily episodes, P=.024), less pain severity compared to baseline (1.41cm [IQR: 0.32–5.23] versus 4.63cm [IQR: 2.51–6.39] measured by 10-cm Visual Analogue Scale, P=.035), less interference with daily activities, and less gastrointestinal symptoms. Only 15% of patients found it difficult to follow the diet.
ConclusionsThe implementation of a low FODMAP diet for 2 weeks in a Mediterranean paediatric population diagnosed with functional abdominal pain is possible with adapted diets. It was highly valued by patients, and they showed an improvement in abdominal pain symptoms assessed by objective methods.
La dieta baja en FODMAP (acrónimo en inglés de polioles, monosacáridos, disacáridos y oligosacáridos fermentables) ha demostrado eficacia como tratamiento del síndrome de intestino irritable en adultos, siendo escasos los estudios en niños. Nuestro objetivo es analizar la implantación de esta dieta como tratamiento del dolor abdominal crónico funcional en población pediátrica de un área mediterránea, y su respuesta a esta.
Material y métodosSe elaboró una tabla clasificando los alimentos según su contenido en FODMAP, y se diseñó un «Diario de síntomas y deposiciones» para recoger los datos. Posteriormente se realizó un estudio prospectivo con niños con dolor abdominal crónico funcional de nuestra Unidad de Gastroenterología Pediátrica.
ResultadosSe reclutaron 22 pacientes, 20 de los cuales completaron el estudio. Se recogieron durante 3 días datos sobre el dolor abdominal; posteriormente recibieron dieta baja en FODMAP 2 semanas, y al finalizarla recogieron de nuevo dichos datos. Tras la dieta se objetivó disminución en frecuencia diaria de episodios de dolor abdominal (1,16 [RIQ: 0,41-3,33] frente a 2 [RIQ: 1,33-6,33] inicialmente, p=0,024), menor intensidad del dolor (1,41cm [RIQ: 0,32-5,23] frente a 4,63cm [RIQ: 2,51-6,39] inicial, p=0,035, medido mediante Escala Visual Analógica de 10cm), menor interferencia con la actividad diaria y menos síntomas acompañantes. Solo un 15% de los pacientes consideraron la dieta difícil.
ConclusionesLa implantación de una dieta baja en FODMAP durante 2 semanas en una población pediátrica mediterránea con dolor abdominal crónico funcional es posible utilizando dietas adaptadas, es bien valorada por los pacientes, y su evaluación mediante herramientas objetivas muestra mejoría en los síntomas de dolor abdominal.
Chronic functional abdominal pain (CFAP) is the leading cause of long-term abdominal pain in the paediatric age group1 and belongs in the category of functional gastrointestinal disorders (FGIDs). These disorders are hypothesised to result from an interaction of psychosocial, environmental and genetic factors, alterations in gastrointestinal motility and the distensibility of the abdominal wall and the presence of an abnormal gut microbiome, which together promote the development of visceral hyperalgesia.2,3
Multiple treatments have been proposed for CFAP, but none have been clearly proven effective. In recent years, some authors have proposed a potential association between the manifestations of CFAP and the malabsorption of specific components of certain foods, which would trigger symptoms through carbohydrate malabsorption, and whose restriction in the diet would alleviate abdominal pain symptoms.4 Among these dietary changes, the restriction of short-chain fermentable carbohydrates, also known as FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) has been investigated in studies in adults with irritable bowel syndrome (IBS).5–10
The rationale for the restriction of FODMAPs is that these carbohydrates are barely absorbed in the small intestine and thus remain in its lumen, where they have an osmotic effect that draws in water, to then pass intact to the colon, where they are fermented by colonic bacteria with the ensuing generation of organic gases and acids, which cause abdominal distension. In individuals with visceral hyperalgesia, the abdominal distension produced by either gases or liquids may trigger or exacerbate abdominal pain.10,11
The FODMAPs include fermentable oligosaccharides (fructooligosaccharides and galactooligosaccharides), disaccharides (lactose), monosaccharides (fructose) and polyalcohols (sorbitol, mannitol, maltitol, xylitol).12 Fructose is absorbed by diffusion facilitated by the GLUT5 transporter; its malabsorption is dose-dependent, and approximately 30% of the population has a very limited capacity to absorb it in free forms.12,13 Lactose needs to be hydrolysed by the enzyme lactase, whose activity decreases through early childhood in most humans.12 As for polyols, 70% are not absorbed by healthy individuals.14 Lastly, the oligosaccharides include the fructooligosaccharides (FOS), which are absorbed in vary small amounts, and galactooligosaccharides (GOS), which are not absorbed.15
In the adult population with IBS, a low FODMAP diet has been shown to achieve good symptom control in approximately 70% of patients.16,17 When it comes to the paediatric age group, this far there is only one published study on its effect in children with IBS, conducted in the United States, which showed positive results.18 However, there are no data on the paediatric population of the Mediterranean region, whose diet is very different from the diet in the United States, as the latter usually includes a much higher amount of FODMAPs compared to the Mediterranean diet.14
On the other hand, since IBS is one of the FGIDs associated with abdominal pain,2 it seems reasonable to propose that these dietary changes could be useful in the management of CFAP, as the two disorders have similar underlying pathophysiological mechanisms.
For these reasons, we present this study, whose main goal was to assess the implementation of the low-FODMAP diet in clinical practice for treatment of CFAP in a Mediterranean paediatric population, taking into account the adaptations required for the characteristic diet of the region. We describe the method used to collect data on the impact of this intervention in terms of the reduction of the frequency and intensity of abdominal pain episodes, the reduction of the interference of abdominal pain in daily activities, changes in the characteristics of bowel movements and accompanying symptoms and the perception of families, and present the outcomes observed in our sample.
Materials and methodsStudy design for the introduction and assessment of a low-FODMAP dietTo introduce the low-FODMAP diet in a sample of a Mediterranean paediatric population, we reviewed the foods proposed in previous studies, such as those by Barret and Gibson4 or Magge and Lembo,19 and developed a table (Table 1) classifying foods as “allowed” or “not allowed” based on their FODMAP content, adapting the selection of foods to the dietary characteristics of our region.
Classification of foods based on their FODMAP content.
| Food groups | Foods with a high FODMAP content | Foods with a low FODMAP content |
|---|---|---|
| Dairy | Cow's, sheep and goat milk. Yogurt, ice cream, fresh cheese, cheese aged for a short time | Lactose-free milk, rice milk, lactose-free yogurt, sorbets, ice lollies, cured cheese |
| Fruits | Apple, pear, peach, nectarine, apricot, flat peach, mango, cherry, watermelon, persimmon, plum, raisins, nuts, canned fruit, fruit juice, high fruit intake | Banana, orange, mandarin orange, lemon, lime, grape, kiwi, strawberry, raspberry, blueberry, melon, papaya, grapefruit |
| Vegetables | Artichoke, asparagus, broccoli, cauliflower, Brussels sprouts, mushrooms, leek, garlic, onion, peas, beet, cabbage, fennel, avocado | Corn, celery, lettuce, tomato, green beans, chard, spinach, zucchini, pumpkin, pepper, aubergine, potato |
| Cereals | Foods made with wheat or rye (if eaten in large amounts) such as bread, pasta, biscuits, couscous, crackers | Gluten-free foods (made with corn, rice) |
| Legumes | Lentils, chickpeas, dried beans | |
| Sweeteners | Artificial sweeteners: hydrogenated isomaltose or isomalt, sorbitol, xylitol, manitol, other sweeteners with names ending in -ol. Honey | Sucrose, glucose, other artificial sweeteners whose names do not end in -ol |
| Protein | Meat, fish, eggs |
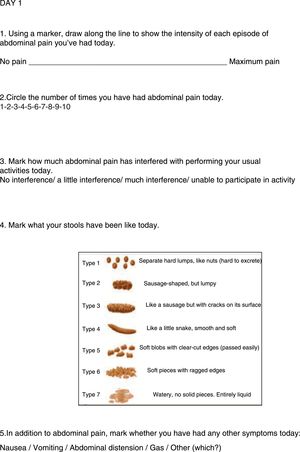
Later on, we designed a “Diary of symptoms and bowel movements” to collect data on the characteristics of abdominal pain in the patients in our study, and to be able to compare these characteristics before and after the implementation of the diet (Fig. 1). The diary was used to collect data on the following variables:
- (a)
Intensity of abdominal pain assessed by means of a visual analogue scale (VAS) consisting of a line measuring 10 cm anchored with the phrases “no pain” and “maximum pain”, across which children were asked to draw a line to indicate the intensity of their pain.20
- (b)
Number of episodes of abdominal pain per week.
- (c)
Interference with daily activities, rated with a 4-point Likert scale: 1 (“no interference”), 2 (“little interference”), 3 (“much interference”) and 4 (“unable to participate in activity”).20
- (d)
Characteristics of stools based on the Bristol stool scale modified for children.21
- (e)
Associated symptoms, such as abdominal distension, gas, vomiting, nausea and other.
Lastly, to assess how the diet was perceived by families, we designed a questionnaire to collect the opinions of children and their families as to how easy it was to follow the diet, the degree of adherence with it, and overall satisfaction with the diet, all of which were rated on a 5-point Likert scale.22
Performance of the studyWe conducted a prospective study over a 10-month period, consecutively including all patients aged 5 to 15 years with a diagnosis of CFAP based on the Roma III criteria23 that sought care in the paediatric gastroenterology and nutrition unit of a tertiary care hospital. The exclusion criteria were age less than 5 or greater than 15 years, the presence of warning signs or clinical suspicion of an organic cause, a previous diagnosis of organic disease, or refusal of parents to consent to participation in the study.
All participating patients and their parents or legal guardians were informed about the study and received an explanatory written document about it, and, once they agreed to participate, signed an informed consent form before being included. The study was approved by the Clinical Research Ethics Committee of the autonomous community of Aragon.
Statistical analysisWe used Microsoft Excel 2007 to create the database and SPSS version 23.0 to perform the descriptive and inferential analyses. We have summarised descriptive results as median and interquartile range. Due to the small sample size (n=20), we used nonparametric tests in the inferential analysis. We used the Wilcoxon and the McNemar tests. We set the threshold of statistical significance at 95% for all tests (P<.05).
ResultsWe recruited 22 patients, of who 20 completed the study (10 female and 10 male). Of the 2 losses to followup, one occurred before the introduction of the diet due to improvement of abdominal pain, and the other after introduction of the diet due to family circumstances. The median age in our sample was 10 years (IQR, 8.25–11.75), and the median duration of abdominal pain at the beginning of the study was 36 months (IQR, 12–99). All patients had undergone an abdominal ultrasound and blood tests including a complete blood count, chemistry panel, levels of coeliac disease markers, immunoglobulins, liver function panel and levels of acute phase reactants. Based on the Roma III criteria,23 of the 20 patients, 12 met the criteria for functional abdominal pain, 6 for functional dyspepsia and 1 for IBS.
Once enrolled in the study, patients received a copy of the Diary of Symptoms and Stools, which they had to fill out for 3 consecutive days, after which they started a 2-week low-FODMAP diet. Before starting, we educated them on what the diet involved and gave them the table that classified foods by FODMAP content (Table 1). We instructed them to avoid all high-FODMAP foods for 2 weeks, emphasising that the table showed alternative, allowed low-FODMAP foods for each category (except legumes). We asked patients to fill out an identical Diary of Symptoms and Stools during the last 3 days of the diet, and once the diet was completed, patients were re-evaluated and families asked about the feasibility of, adherence to and satisfaction with the diet.22 Lastly, after this 2-week restrictive period, we recommended the progressive reintroduction of FODMAPs. The order in which the high-FODMAP food groups were introduced was left to the choice of the patient, as long as foods were introduced on different days and in increasing doses to allow the identification of the foods associated with abdominal pain and the amount of each food required to trigger pain in each patient.
Comparing the baseline and the final diaries, we found that after following a low-FODMAP diet for 2 weeks, patients exhibited a reduction in the daily number of abdominal pain episodes, with a pre-intervention median of 2 (IQR, 1.33–6.33) and a post-intervention median of 1.16 (IQR, 0.41–3.33) (P=.024), as well as a reduction in the intensity of abdominal pain as measured with the 10-cm VAS, from 4.63 (IQR, 2.51–6.39) to 1.41 (IQR, 0.32–5.23) (P=.035). Patients also reported less interference of abdominal pain with daily activities and fewer associated symptoms like abdominal distension or gas, while the characteristics of their stools remained similar, with no statistically significant differences between the pre- and post-diet periods (Table 2).
Symptoms before and after the diet.
| Before (n=20) | After (n=20) | |
|---|---|---|
| Interference with activities (P=.061) | ||
| No interference | 4 patients | 12 patients |
| A little interference | 12 patients | 5 patients |
| Much interference | 2 patients | 2 patients |
| Unable to participate in activity | 2 patients | 1 patient |
| Associated symptoms | ||
| Gas (P=.180) | 14 patients | 9 patients |
| Distension (P=.25) | 5 patients | 2 patients |
| Nausea | 1 patient | 0 patients |
| Stool characteristics (Bristol scale adapted for children) (P=.261) | ||
| Bristol 1–2 | 4 patients | 5 patients |
| Bristol 3–4 | 14 patients | 13 patients |
| Bristol 5–6 | 2 patients | 2 patients |
At the end of the study, we asked patients and their families about how they perceived the diet. Of the 20 patients, 6 answered that they found it very easy to follow, while 7 found it easy, 4 a little difficult and 3 difficult. As for adherence, 13 reported substantial adherence, 6 good adherence and 1 fair adherence. Overall, 8 of the 20 patients reported that they were very satisfied with the results and 4 fairly satisfied, while 4 felt indifferent and 3 were not satisfied.
DiscussionChronic functional abdominal pain can have a negative impact on the quality of life of patients, who often experience chronic symptoms for which none of the available treatments were effective.24
In recent years, and parallel to the increase in the prevalence of CFAP, there has been a shift in the Western dietary pattern, with an increased intake of fructose and fructans due to an increased consumption of wheat-based and processed foods and also polyols, in response to an increased demand for sugar-free products.25 This increase in the intake of FODMAPs could promote the development of abdominal pain in children with CFAP, because these substances are poorly absorbed by the small intestine, which has an osmotic effect, and are subsequently fermented by colonic bacteria, which generates gases and abdominal distension.13 It follows that consumption of a low-FODMAP diet would decrease osmotic activity, carbohydrate fermentation and gas formation in the enteral lumen, alleviating abdominal distension and pain in these children.
The only study in the literature that has evaluated the impact of a low-FODMAD diet in the paediatric age group was conducted in the United States in a sample of children with IBS.18 We thought it would be relevant to investigate the possibility of introducing this diet in clinical practice for treatment of children with CFAP in a paediatric gastroenterology and nutrition unit in the Mediterranean region.
To this end, we reviewed the existing literature4,19 to develop a table of foods categorised by FODMAP content and adapted to the Mediterranean diet that would provide information about the most common foods in this diet and suggest a wide range of alternatives to excluded foods.
On the other hand, to obtain valid data, we developed a “Diary of symptoms and bowel movements” to facilitate the quick and easy collection of data regarding the baseline and post-intervention characteristics of abdominal pain to be able to compare and assess change between the two periods while minimising information bias. We chose the visual analogue scale to assess the intensity of abdominal pain, as it has been proven to be easy to use, valid and reliable for assessment of pain in children.20
As for clinical response, we found that the low-FODMAP diet could be an option for treatment of CFAP in children, as our patients exhibited a considerable reduction both in the daily number of episodes and the intensity of pain after the introduction of the diet, combined with a decrease in associated symptoms. These results are consistent with those reported by Chumpitazi et al.,18 who found improvement in these parameters after implementation of the low-FODMAP diet compared to the baseline diet and to the typical American childhood diet.
Similarly, studies conducted in the adult population with IBS have found significant reductions in abdominal pain and distension following the introduction of low FODMAP diets, both in cohort studies7,8 and in studies comparing individuals following the diet usually recommended for IBS16,26,27 and individuals consuming a high-FODMAP diet.9,10
In our study, patients also experienced a decrease in the interference of abdominal pain with everyday activities after the introduction of the low-FODMAP diet, which entailed a considerable improvement in their quality of life, as has already been reported in adults.28 On the other hand, we found no significant changes in stool characteristics after the introduction of the diet, which was also consistent with the previous literature.9,16,26
We designed this study with the goal of assessing the implementation of this diet in everyday clinical practice. Thus, while our results showed good symptom control after the introduction of a low-FODMAP diet, we were unable to draw conclusions on its efficacy for treatment of CFAP in the paediatric age group, in part due to the small sample size, but most importantly due to the lack of a control group. We need to take into account that when a restricted diet is implemented without a control group, favourable results may be partly due to the potential placebo effect of removing certain foods. Still, these limitations are shared by many of the published studies on the subject of dietary interventions, as it is difficult to carry out controlled double-blind studies of diets.29,30
On the other hand, the potential role of non-coeliac gluten sensitivity (NCGS) in the improvement observed in these patients is currently being debated, as the low-FODMAP diet excludes wheat and therefore, to a great extent, gluten. However, there is also evidence that at least some patients with NCGS experience improvement with the exclusion of the oligosaccharides (FODMAPs) present in wheat independently of gluten intake,30–32 which suggest that further investigation is required on this aspect.
Since the low-FODMAP diet is a restrictive diet, there are concerns regarding long-term nutritional balance. In adults, it has been associated with a reduced intake of dietary fibre5 and a mild decrease in energy and calcium intake, with normalization with the progressive introduction of FODMAPs.33 If patients receive appropriate nutritional counselling, this diet can provide adequate nutrition,34 but this may not be the case if the diet is followed without supervision from a doctor or dietitian.35,36
However, there are no studies assessing the nutritional impact of a low-FODMAP diet in the paediatric population. This is one of the reasons why in our study we limited the duration of the diet to 2 weeks as opposed to 3-6 weeks, as recommended in the adult population,5 as a shorter duration could be just as effective18,19 while minimising potential nutritional risks and facilitating adherence. Indeed, most of our patients found this diet easy or very easy to follow, and nearly all families reported a high level of adherence to the diet, which is associated with better symptom control.7,11
Last of all, there are concerns regarding the potential negative impact on the intestinal flora of the exclusion of FODMAPs with a prebiotic effect. Some authors have reported changes in the composition of the gut microbiome and a reduction in the concentration of bifidobacteria,10,11,26,37 without an increase in the population of pathogenic bacteria,38 and the long-term effects on the microbiota remain unknown.39
Due to the above concerns, we do not recommend following a low-FODMAP diet for prolonged periods of time, and instead propose implementing a restricted diet of limited duration followed by the gradual reintroduction of different foods to determine which ones cause symptoms with the ultimate purpose of establishing the least restricted diet possible. In some cases, only a discrete reduction of specific FODMAPs is necessary.40
In conclusion, the implementation of a short-term low-FODMAP diet in children in our region for treatment of CFAP was feasible with the use of specially adapted diets, and we recommend the use of objective instruments to assess changes in symptoms. We ought to highlight that children and families in our sample considered this diet easy to follow, which, combined with its favourable outcomes, resulted in substantial patient satisfaction. Since there are no data on its long-term nutritional safety in the paediatric age group or on its effects on the intestinal microbiota, we recommend limiting the restrictive phase of the diet to a short period of time, followed by the progressive reintroduction of foods, as well as implementation of the diet under the supervision of a doctor or dietitian.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Baranguán Castro ML, Ros Arnal I, García Romero R, Rodríguez Martínez G, Ubalde Sainz E. Implantación de la dieta baja en FODMAP para el dolor abdominal funcional. An Pediatr (Barc). 2019;90:180–186.
Previous presentation: this study was presented at the 50th Annual Meeting of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN); May 11–13, 2017; Prague, Czech Republic.