School-aged children with type 1 diabetes (DM1) require access to appropriate and safe care for their disease during their stay in the educational centre.
ObjectiveTo identify the needs perceived by families of schoolchildren with DM1 that affect their educational integration, safety, and well-being during the school day.
MethodologyA descriptive and cross-sectional study was conducted using a questionnaire based on information and opinions provided by families of 362 schoolchildren between 3 and 16 years old with DM1 registered in their health history in the Public Health System of Extremadura.
ResultsThe response rate was 56.9% (206). It was shown that 35% of schoolchildren with DM1 were treated with continuous subcutaneous insulin infusion therapy. Almost all of them (95.1%) required glucose monitoring, and 57.8% required insulin administration during the school day. Most (88%) children had adjusted well to school and did not describe any type of discriminatory treatment (87.4%). Glucagon is available in 82% of educational centres, in which 43.7% had a trained adult person to administer it. That teachers could recognise a hypoglycaemia was expressed by 21.4% of the families, and 29.1% were unaware of the existence of coordination protocols in the school. More than half (58.7%) claimed that the information available in schools about diabetes was low, and 77.2% stated that the control of the disease would improve if more training was provided to teachers.
ConclusionsThere are aspects optimally covered in the care of schoolchildren with DM1 in the schools of Extremadura. Among situations identified with potential room for improvement were adherence to the coordination protocol, information about diabetes, and training of adults to deal with emergency situations.
El alumnado con diabetes tipo 1 (DM1) requiere durante su estancia en el centro educativo unos cuidados adecuados y seguros para su enfermedad.
ObjetivoIdentificar las necesidades percibidas por las familias del alumnado con DM1 que afecten a la integración educativa, seguridad y bienestar durante la jornada educativa.
MétodosEstudio descriptivo y transversal, mediante encuesta, basado en la información y opiniones proporcionada por las familias de los 362 pacientes entre 3 y 16 años con DM1, registrados en la historia de salud del Sistema Sanitario Público de Extremadura.
ResultadosTasa de respuesta del 56,9% (206). El 35% del alumnado con DM1 estaba en tratamiento con infusión subcutánea continua de insulina. El 95,1% precisó medir la glucemia y el 57,8% administrarse insulina durante la jornada escolar. Un 88% presentó buena adaptación al colegio y el 87,4% no describió ningún tipo de trato discriminatorio. El 82% de centros dispuso de glucagón y en un 43,7% hubo alguna persona adulta entrenada para administrarlo. Un 21,4% de familias pensaban que los profesores podían reconocer una hipoglucemia. El 29,1% desconocían la existencia de protocolos de coordinación en centros educativos, el 58,7% alegaron que la información en el centro sobre diabetes fue poca y un 77,2% que su control mejoraría con más formación del profesorado.
ConclusionesExisten aspectos óptimamente cubiertos en la atención al alumnado con DM1 en los centros educativos de Extremadura. Las situaciones con margen de mejora son la adherencia al protocolo de coordinación, la información sobre la diabetes y el adiestramiento de adultos ante emergencias.
Type 1 diabetes (T1D) is one of the most prevalent chronic diseases in childhood and adolescence. Of the 490000 children living with T1D, 24% reside in the European Region.1 Furthermore, its incidence continues to increase,1,2 and it is estimated that approximately 78000 children aged less than 15 years develop the disease each year worldwide.3,4 In Spain, an incidence rate of 17.69 cases/100000 inhabitants/year has been reported in children aged less than 15 years.5 In the Autonomous Community of Extremadura, the most recent studies show even higher figures of up to 25.2 cases/100000 inhabitants.6,7
Type 1 diabetes is a disease that requires immediate care and lifelong treatment after diagnosis. Its daily management requires the whole household to adapt to a new way of life, as it requires frequent monitoring of blood glucose levels, keeping track of carbohydrate intake and continuously adjusting insulin doses according to the physical activity and diet of the patient.8 Thus, it would be very difficult for children to follow recommendations for the management of diabetes without appropriate support from their families, who need to be educated on how to care from the patient at the outset.9
One of the greatest challenges faced by schoolchildren with T1D and their families is how to manage the disease at school, as young children in preschool and primary school have yet to develop the skills required to adequately manage their diabetes on their own.10 Schoolchildren spend approximately one third of the day in the school, so it is essential for them to have access to adequate care11 in order to participate in all the school activities and have the same opportunities as all other students.12 Appropriate school-based diabetes care is necessary to guarantee the immediate safety of students with T1D, their long-term wellbeing and an adequate academic performance.13
In 2011, a Protocol for the Care of Children and Adolescents with Diabetes in Schools was introduced in Extremadura (currently integrated in the Protocol for the Management of Medical Emergencies in Schools of Extremadura14), leading to significant advances in the monitoring, safety and equality of opportunities of students with T1D. It is the responsibility of families to inform the school about the protocol, at which point a personalised care plan starts to be implemented. The referring nurse, who usually belongs to a primary care team, is responsible for providing basic training on diabetes in schools, educating teachers on how to respond to an emergency and overseeing the personalised care plan.14 In 2014, the coverage of this protocol had reached 67.7%15 and it has continued to increase, reaching 74% in 2016 (data not published).
The aim of our study was to establish the current needs of schoolchildren with T1D in Extremadura from preschool through age 6 years based on the information provided by their families, with the purpose of identifying opportunities for improvement in the care and seamless integration of this population in the school setting.
MethodsWe conducted a cross-sectional, observational and descriptive study based on the information and opinions given by the families of students with T1D aged 3–16 years enrolled in schools in Extremadura.
The universe of the study consisted of 362 children with T1D with files in the health record database of the public health system of Extremadura (Servicio Extremeño de Salud).
We collected information using a questionnaire specifically designed for the purpose (Appendix B), which we developed taking into account previous research15–19 and was reviewed by a panel of experts. We carried out a pilot study to ascertain the understanding of the items of the questionnaire and analyse its internal consistency (Cronbach α, 0.772). We mailed the questionnaires by certified post, including an envelope with prepaid postage for its submission and a letter to inform the recipient about the study.
We entered the submitted data in a database and analysed them using the software IBM® SPSS® Statistics version 25 for Windows®. We have summarised qualitative variables as absolute and relative frequencies and compared them by means of the Pearson chi-square test. We defined statistical significance as a P-value of less than .05.
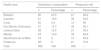
ResultsWe submitted 362 questionnaires and received 206 responses (response rate, 56.9%); when it came to the distribution among the 8 administrative health areas of Extremadura, participation was highest in Plasencia (75.9%) and lowest in Badajoz (48.2%). In 1.9% of responses, the participant had not specified the health area to which they belonged (Table 1).
Response rate by health area.
| Health area | Distribution of population | Response rate | ||
|---|---|---|---|---|
| n | Percentage | n | Percentage | |
| Badajoz | 85 | 23.5 | 41 | 48.2 |
| Cáceres | 61 | 16.9 | 32 | 52.5 |
| Coria | 20 | 5.5 | 10 | 50 |
| Don Benito-Villanueva | 57 | 15.7 | 32 | 56.1 |
| Llerena-Zafra | 38 | 10.5 | 21 | 55.3 |
| Mérida | 54 | 14.9 | 35 | 64.8 |
| Navalmoral de la Mata | 18 | 5 | 10 | 55.6 |
| Plasencia | 29 | 8 | 21 | 72.4 |
| Total | 362 | 100 | 206 | – |
Questionnaires were completed by the mother (78.6%), father (18%) or legal guardian (1.5%) of the child. Table 2 presents the sociodemographic and clinical characteristics of the schoolchildren included in the sample.
Sociodemographic characteristics, age of onset and treatment.
| Variable | n | Percentage |
|---|---|---|
| Sex | ||
| Male | 109 | 52.9 |
| Female | 97 | 47.1 |
| Age group (years) | ||
| 3–5 years | 14 | 6.8 |
| 6–9 years | 46 | 22.3 |
| 10–12 years | 65 | 31.6 |
| 13–15 years | 63 | 30.6 |
| 16 years | 18 | 8.7 |
| Years from onset of diabetes | ||
| <3 years | 78 | 37.4 |
| 3–6 years | 54 | 26.2 |
| >7 years | 68 | 33.5 |
| N/A | 6 | 2.9 |
| Type of school | ||
| Public | 171 | 83.0 |
| Private with public funding | 31 | 15.0 |
| Private | 1 | 0.5 |
| N/A | 3 | 1.5 |
| Type of treatment | ||
| Multiple daily injections | 131 | 63.6 |
| Infusion pump | 72 | 35 |
| N/A | 3 | 1.5 |
N/A: did not answer.
A little more than half of the families (54.4%) were members of an association of individuals living with diabetes. Half of the parents reported that they had needed to change their work schedule to help care for their child in school, most frequently in the age range of 6–9 years (68.9%) (P=.003). No children had been denied admission to a school due to their diabetes.
Most schoolchildren with T1D were under pharmacological treatment with multiple daily injections of insulin (MDI, 63.6%), followed by insulin pump therapy (35%), whose use varied with age and was more frequent in children aged 3–5 years and 16 years (42.9% and 50%, respectively).
When it came to the sources of information and education on diabetes, families mainly reported seeking them from health care professionals (92.7%). Also, 18% reported seeking support in summer programmes, which was more common in families that belonged to diabetes associations (31.3%) compared to those that did not (2.2%) (P<.001). Most respondents (90.8%) stated that they had not needed to seek psychological care for their children due to circumstances associated with the disease, and we found no differences in the need for psychological care based on sex.
Of all families, 70.9% were aware of the Protocol for the Care of Children and Adolescents with Diabetes in Schools of Extremadura. Most have been informed of its existence by health care professionals (54.4%), followed by the school (33.6%) and diabetes associations (26%).
Self-management of type 1 diabetes by schoolchildrenAll students brought some type of snack with them to school to manage potential episodes of hypoglycaemia, most frequently soft drinks or juices (68.9%), biscuits (57.8%), sugar or candy (56.8%) and glucose formulations (23.8%).
Nearly all children knew how to measure their blood glucose level (93.7%) and interpret the results (88.8%), with no difference between the sexes. The percentage was lower in younger children, and it was between ages 10 and 12 years that children developed the ability to self-manage glucose monitoring and insulin administration, as can be seen in Table 3.
Skills of schoolchildren to self-manage diabetes.
| Skills | Total sample | 3–5 years | 6–9 years | 10–12 years | 13–15 years | 16 years |
|---|---|---|---|---|---|---|
| Measurement of glucose levels (%) | 93.7 | 42.9 | 93.3 | 100 | 100 | 100 |
| Interpretation of glucose levels (%) | 88.8 | 21.4 | 82.2 | 98.5 | 98.4 | 100 |
| Administration of insulin (%) | 83 | 7.1 | 60 | 96.9 | 100 | 100 |
| Dose and type of insulin (%) | 73.8 | 0 | 40 | 84.4 | 100 | 100 |
During the school day, most children needed to measure their blood glucose levels (95.1%) and more than half needed to receive insulin (57.8%). These children usually monitored their own glucose (76.5%) and a high percentage injected insulin themselves (81.5%).
By age group, children aged less than 6 years depended on others, usually parents/legal guardians and teaching staff, for the administration of insulin and blood glucose monitoring, with autonomy increasing in subsequent years (Table 4).
Need for blood glucose monitoring and administration of insulin during school hours and need for help in these activities.
| Total sample | 3–5 years | 6–9 years | 10–12 years | 13–15 years | 16 years | |
|---|---|---|---|---|---|---|
| Needed blood glucose monitoring (%) | 95.1 | 100 | 100 | 98.5 | 93.7 | 72.2 |
| Needed no help (%) | 76.5 | 14.3 | 45.7 | 89.2 | 95 | 100 |
| Help from parents/guardians (%) | 14.5 | 42.9 | 37 | 9.2 | 1.7 | 0 |
| Help from teachers (%) | 7 | 42.9 | 10.9 | 1.5 | 1.7 | 0 |
| Help from others (%) | 2 | 0 | 6.5 | 0 | 1.7 | 0 |
| Needed insulin administration (%) | 57.8 | 42.9 | 56.5 | 56.9 | 61.9 | 61.1 |
| Needed no help (%) | 81.5 | 0 | 50 | 94.7 | 97.4 | 100 |
| Help from parents/guardians (%) | 16.8 | 83.3 | 46.2 | 5.3 | 2.6 | 0 |
| Help from teachers (%) | 0.8 | 16.7 | 0 | 0 | 0 | 0 |
| Help from others (%) | 0.8 | 0 | 3.8 | 0 | 0 | 0 |
The information that the families provided the school about the condition of the child was usually given to the form tutor (95.6%), followed by school administrators (77.9%) and, less frequently, to other teachers (66.2%) and other students (63.2%).
More than half of respondents (55.8%) reported that their school lacked a dedicated space to monitor glucose or inject insulin during school hours. Most respondents reported that glucagon was available in their school (82%), but only half of them that there was someone in the school trained on how to administer it (43.7%). We ought to highlight that 39.3% of families did not know the answer to this question. We did not find statistically significant differences in the resources reported to be available at the school based on whether the family was or was not aware of the existence of the protocol.
Seven out of 10 schoolchildren had experienced episodes of hypoglycaemia while at school, with a higher frequency in children aged 6–9 years (78.3%) or 16 years (76.5%). Only 21.4% of the families felt sure that most teachers were able to identify this complication of diabetes. In 33% of cases, these episodes occurred before or during an exam, and less than half of these students (47.1%) were allowed to retake the exam at a later time. We did not find any differences in these variables based on the type of school.
A high percentage of respondents (77.2%) reported that diabetes control would improve if teachers were given more information and training on the disease, a demand that was voiced most strongly by respondents with children in public schools (81.9%) compared to those with children in fully private or publicly funded-private schools (64.5%) who, we may add, did not know how to answer the question in 25.8% of cases (P<.001).
Adaptation and integrationMost schoolchildren were well adjusted in their school before diagnosis (88%), and, of these children, 7.7% went on to have fair or poor adjustment after diagnosis according to their families.
When asked about whether problems or difficulties developed in school after the diagnosis of diabetes, 39.8% of respondents answered that they did, and they consisted in concentration problems (68.3%), poor academic achievement (52.2%), lack of interest and motivation (37.8%) and, in a few cases, problems with teachers (18.3%) or with other students (12.2%). We found no differences based on sex.
In most cases (87.4%), respondents reported that their children did not experience any form of discrimination associated with diabetes, and we found no differences on this aspect based on student sex or type of school. Among those that experienced discriminatory treatment, 43.8% reported it was from teachers, 31.3% from other students, and 12.5% from school administrators.
When it came to the support received at school, most families reported that the main sources were other students (71%) and teachers (65%), and a lower percentage reported receiving support from the administration (28.5%).
Very few students with diabetes used school lunch services (2.4%), most frequently because the service was not available (36.1%), the school was near the home (29.2%) or the service did not have qualified staff or did not offer adapted menus (4%).
All students with T1D engaged in physical education activities with the rest of the students, and more than half (55.8%) experienced episodes of hypoglycaemia in the course of these activities. However, only 31% of families felt that physical education teachers were capable of identifying the symptoms of hypoglycaemia.
Most students participated in field trips and extracurricular activities not requiring an overnight stay (82.9%). This participation dropped considerably when activities lasted several days (32.2%), especially in children aged less than 10 years (6.5%).
Last of all, more than half of the families (58.7%) considered that the school had little information about diabetes, with a minority reporting that the school had considerable or a lot of information on the subject (4.4%), and there were no differences on this aspect based on type of school or awareness of the protocol on the part of the family.
Discussion and conclusionsIn this study, we assessed the needs related to type 1 diabetes of schoolchildren in Extremadura by obtaining information from their families. This is the first study conducted on the subject at the autonomous community level in Extremadura, where, due to special characteristics such as the high regional incidence of diabetes and the amount of the population that resides in rural areas and their geographical dispersion, it is particularly important to continue advancing the full normalising and integration of these schoolchildren.
The study reflected the widespread use of continuous subcutaneous insulin infusion (CSII) in Extremadura (amounting to one third of schoolchildren with T1D), an approach that achieves better glycaemic control and reduces the risk of hypoglycaemia16,17 and the costs associated with episodes of severe hypoglycaemia.18 This proportion nears the proportion achieved in other European countries19 and is above the national average in Spain based on the reports of the Federación Española de Empresas de Tecnología Sanitaria (Spanish Federation of Businesses in Health Care Technology [FENIN]), which found that CSII was used in 4% of patients in Spain in 2012 (unpublished data), and on studies conducted in other autonomous communities.20,21
Diabetes has an impact on the family routine, and half of parents/legal guardians had to make adjustments to their work schedule, a proportion similar to the one found in the nationwide study by Beléndez and Lorente,22 although in our study this occurred more frequently in parents or guardians of children aged 6–9 years and less frequently in those of children aged less than 6 years. This may be related to schooling not being mandated by law in the younger age group, an issue that we did not explore but that should be taken into consideration in future studies. Few families (7.7%) reported a poorer adjustment to school life after diagnosis, consistently with other nationwide studies.23 Most families sought the information they need about diabetes from health care professionals, and in nearly every case the schoolchildren received education on diabetes in paediatric clinics, as recommended by the American Diabetes Association.10 Few families (18%) sought to reinforce diabetes education in the summer programmes organised by associations of patients with diabetes, even though more than half of the sample belonged to one of these associations.
Overall, schoolchildren with T1D exhibited an ability to self-manage the disease that was considered age-appropriate based on current recommendations10 and exceeding the skills found in other studies.24–26 The biggest challenge involves schoolchildren aged 3–9 years, who are totally or partially dependent on adults for management, especially when it comes to the injection of insulin, which requires more training and collaboration on the part of the school staff.
At any rate, regardless of the responsibility that each child takes on in self-management, supervision and support from a properly trained adult is still always recommended in case an emergency arises.10 However, we found that families were unsure whether teaching staff, including the physical education teachers, were trained to identify and manage hypoglycaemia. This is a key issue considering that 2 out of 3 schoolchildren with T1D had suffered episodes of hypoglycaemia during school hours and half during physical education activities. Most families considered that further education and training of the teaching staff is required in relation to all the above aspects. This issue may be at the heart of the reason why children with T1D are less likely to join in extracurricular activities lasting longer than 1 day, which may have a negative impact on normalising and integration in school. The fact that 3 out of 10 families were unaware of the protocol for the coordination of diabetes management in school settings, a finding that was consistent with the reported coverage of the protocol, could mean that, by not being put into action, teachers are less prepared and the schools have fewer resources for the management of emergencies related to diabetes. However, based on the information we obtained from the families, we did not find an association between these 2 variables. This aspect is an important area for improvement in the implementation of protocols, as the coordination of the family, the health care team and the school can guarantee a safer learning environment through the joint implementation of care plans.
While most form tutors had been made aware of the diabetes of the schoolchildren in our sample, 4 out of 10 respondents reported that the rest of the teachers and the classmates were not informed about it, contrary to the findings of the study carried out by Beléndez and Lorente,22 in which classmates of children with diabetes knew they had this disease in 91% of cases. This low level of awareness could have a negative impact on the integration with peers and normalising of children with T1D and in the successful management of episodes of hypoglycaemia.
In conclusion, this study shows that despite the progress made with the implementation of protocols to coordinate families, teachers and health care workers to advance integration and normalising in schoolchildren with T1D, there are still opportunities for improvement that ought to be explored and implemented.
First of all, it is essential that adherence to protocols increases, which could be facilitated by including the protocol in the health records as part of the treatment plan of schoolchildren with T1D and setting up a system for the communication of health care and school administrators that would allow the detection of cases of non-adherence.
In addition, it would be helpful to develop a mandatory training programme for the school setting to guarantee basic knowledge and skills on diabetes that would include the student body and the development of more advanced skills in the teachers in charge of students with diabetes on the identification and management of emergencies related to the disease. This programme should be developed by the school nurse/point of contact and supported by the paediatrics teams that manage the schoolchildren. The use of emerging technologies in the school and health care environments could support the continuing education and communication between all individuals that interact with children with T1D. Advances in health care safety in schoolchildren with T1D will unquestionably contribute to their full integration and improve academic performance, as well as reassure their families.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Tomé Pérez Y, Barroso Martínez V, Félix-Redondo FJ, Tobajas Belvis L, Cordón Arroyo AM. Necesidades del alumnado con diabetes tipo 1 en Extremadura: percepción de las familias. An Pediatr (Barc). 2019;90:173–179.