In 2016, Cronin et al. published a study that demonstrated the noninferiority of dexamethasone compared to prednisolone for treatment of acute asthma exacerbations in the paediatric population.1 Treatment of bronchospasm with dexamethasone requires a single dose, which improves patient adherence compared to prednisolone. For this reason, in December 2016, the paediatric emergency care team in our hospital decided to introduce dexamethasone for the management of bronchospasm. To this end, a 15-min training session was delivered to the department of paediatrics by an adjunct physician employed in the paediatric emergency department, reviewing the scientific evidence on the use of dexamethasone for treatment of asthma. The same training was also delivered individually during working hours to medical residents and adjunct physicians in paediatrics staffing the emergency department who had not attended the initial group training.
The aim of our study was to evaluate the impact of the training session on the management of asthma exacerbations, for which we analysed the percentage of patients that received dexamethasone versus prednisolone. As a secondary objective, we analysed the impact of this change in patient outcomes, for which we calculated the percentage of patients that required admission or had to return to the emergency care unit.
We conducted an observational study by reviewing the health records of patients managed between January 1, 2016 and December 31, 2017 in the paediatric emergency department of a tertiary care hospital with a discharge diagnosis of bronchospasm (ICD-9 493.90). We collected this data from the hospital database. We divided the sample into 2 groups by time period: the pre-intervention group, which included patients managed between January 1 and November 30, 2016, and the post-intervention group, which included patients managed between January 1 and November 30, 2017. We considered the month of December a “window period”, as this was the time that the training sessions were delivered. The outcome variable was the corticosteroid prescribed to the patients.
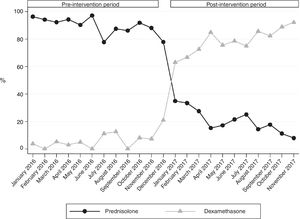
We analysed data for a total of 1688 patients managed during the period under study. There were 734 patients managed in the pre-intervention period and 750 managed in the post-intervention period, while 204 were managed during the window period. We did not find any differences between periods in the age of patients, with a median age in the preintervention period of 27.8 months (interquartile range [IQR], 14.6–61.9) and 23.7 months in the post-intervention period (IQR, 12.1–38.7) (P=.08), nor differences in the severity of the exacerbations (median Pulmonary score in both periods, 4 [IQR, 3–5]; P=.430). In the pre-intervention period, 48.4% of patients (n=343) presented with abnormalities in the paediatric assessment triangle on arrival to the emergency department compared to 49.9% (n=360) of patients in the post-intervention period (P=.557). In the pre-intervention period, 371 patients (50.5%) received steroid therapy compared to 449 (59.9%) in the post-intervention period (P<.01). In the pre-intervention period, 341 (91.9%) were treated with prednisolone and 16 (4.3%) with dexamethasone, while in the post-intervention period 91 received prednisolone (20.3%) and 354 (78.8%) dexamethasone (P<.01). Fig. 1 shows the percentage of patients treated with each of these corticosteroids by month. We found no differences in the proportion of patients that required hospital admission (9.3% in the pre-intervention group vs 9.0% in the post-intervention group; P=.865) or that returned to the emergency department (6.6% in the pre-intervention group vs 6.8% in the post-intervention group; P=.821).
Among the limitations of the study, we ought to highlight the lack of follow-up data on the adherence to treatment with prednisolone, so we could not rule out, although we find it unlikely, that the effect of prednisolone was underestimated due to a lack of adherence on the part of the patients. In addition, the perception of the paediatric staff that the use of dexamethasone was “mandatory” may have falsely inflated the effectiveness of training sessions. However, the fact that there is no established protocol for the management of asthma in the emergency department makes the latter possibility improbable.
Our study demonstrates that the delivery of training sessions in the department of paediatrics was an effective intervention to improve the approach to the treatment of asthma exacerbations while ensuring patient safety.
Please cite this article as: Bolívar Ruiz P, Fernández Arribas JL, Campo Fernández MN, Velasco Zúñiga R. Impacto de unas sesiones formativas en el tratamiento de los episodios de broncoespasmo en urgencias. An Pediatr (Barc). 2019;91:201–202.