Patients may be admitted to hospital by paediatric palliative care units (PPCU) for different reasons, due to their different needs and clinical problems. The objective of this study is to present the data of patients admitted to the PPCU of the Autonomous Community of Madrid.
MethodsDescriptive retrospective study was conducted by reviewing the clinical records of the PPCU between January 2011 and December 2016.
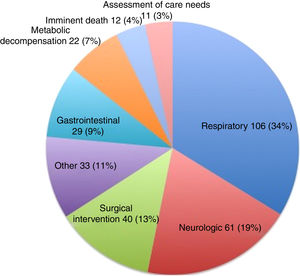
ResultsOf 499 patients attended in this period, 166 (33%) were admitted to hospital at some point, generating a total of 314 episodes. Respiratory problems (34%) were the main cause of admission. Gastrostomy intervention (23 patients) was the commonest reason for a surgical admission. In this period, 46 patients died during hospitalisation. The highest frequencies of death, according to the admission cause, were respiratory problems (18 out 46) and end-of-life care (11 out 46). More than half (59%) of admissions lasted less than 7 days and 88% were 15 days or less.
ConclusionsThe causes and characteristics of the hospital admissions at a PPCU are heterogeneous, with respiratory problems being the most common cause of admission. The duration of the hospitalisation appears to be similar to that described for acute palliative care units. The creation of a specific PPCU that can refer their patients for hospital admission might help to improve continuity of care.
Los pacientes en seguimiento por unidades de cuidados paliativos pediátricos (UCPP) pueden ingresar en el hospital por distintas circunstancias. Cuentan con características dispares en sus necesidades y en las situaciones clínicas que presentan. El objetivo de este estudio es presentar datos correspondientes a los pacientes ingresados a cargo de la UCPP de la Comunidad Autónoma de Madrid.
MétodosEstudio retrospectivo observacional realizado a partir de las historias clínicas de la UCPP. Periodo: enero-2011 a diciembre-2016.
ResultadosDe los 499 pacientes seguidos en ese periodo, 166 (33%) ingresaron en alguna ocasión, generando un total de 314 episodios. El principal motivo de ingreso fueron los problemas respiratorios (34%). El motivo más frecuente de ingreso para intervención quirúrgica fue la realización de una gastrostomía (23 pacientes). En este periodo, 46 pacientes fallecieron durante el ingreso, siendo el motivo más frecuente el ingreso por problemas respiratorios (18/46), seguido de los ingresos por agonía (11/46). El 59% de los ingresos duró menos de 7 días y el 88%, 15 días o menos.
ConclusionesLos motivos y las características de los ingresos hospitalarios a cargo de una UCPP son heterogéneos, siendo los motivos más frecuentes los problemas respiratorios. La duración de la estancia hospitalaria es equiparable a la de unidades de cuidados paliativos de atención aguda. La creación de unidades específicas con posibilidad de ingreso hospitalario a cargo de las mismas puede ayudar a mantener la continuidad asistencial.
In the past 10 years, there has been an exponential growth in paediatric palliative care (PPC)1,2 services in Spain,3 as reflected by the creation of new PPC teams or the institution of the Sociedad Española de Cuidados Paliativos Pediátricos (Spanish Society of Paediatric Palliative Care) in 2016. Following the analysis and development of care standards in this field by the Ministry of Health in 2014,4 some autonomous communities have updated and launched resources to offer PPC services. However, there is still substantial variability in the resources available within and between autonomous communities, and there is no common organisational model.5 In light of the rapid growth of PPC services, we need to share any available data on the use of resources in this field of care. Under certain circumstances, these patients may need to be admitted to hospital, and specific care delivery systems are required to this end.4
The purpose of PPC is to actively address the physical, psychological, social and spiritual needs of children with incurable diseases and their families,6,7 thereby increasing their quality of life. The preferred setting for delivery of PPC is the home. There are different organisational models for PPC,8 including structures like hospice care,9 home-based care teams, “hospital at home” services, hospital-based care teams or PPC units, which operate independently but are integrated in hospital settings. These resources could be interwoven into a single care delivery system, and there are guidelines in the literature that assert that the optimal approach to improving quality of life in these patients and their families is through an integrated network built around specific palliative care teams.10 Given complexity of these patients and the need to ensure the continuity of care, the ideal arrangement would be for the teams in charge of delivering home-based care to be able to also manage their outpatient and inpatient hospital-based care.7,8
The PPC unit of the Community of Madrid was created in 2008 and has since served approximately 700 patients. At present, it is staffed by 6 physicians, 7 nurses, 2 social workers, 2 psychologists and 1 administrative assistant and there is a pharmacist of the Hospital Infantil Universitario del Niño Jesús (HIUNJ), the children's hospital where the unit is physically located, specifically appointed to support the unit. The PPC unit offers 3 levels of care based on individual patient needs. If admission is necessary, patients can be admitted through the PPC unit to the HIUNJ or, if they and their families so prefer, in their local referral hospital, in which case the PPC unit would offer support in clinical decision making to the team that becomes responsible for the patient. In addition, patients previously admitted to other departments of the HIUNJ (neurology, oncology, intensive care1) may be transferred to the PPC unit in the course of their hospitalisation.
The aim of this study was to present the data corresponding to the hospital admissions made through the PPC unit located at the HIUNJ between January 2011 and December 2016.
MethodsWe conducted a retrospective observational study by reviewing the health records of the PPC unit. We collected information for the period between January 2011 and December 2016, including data for the following variables:
- •
Epidemiologic characteristics: sex, age at admission and disease group or quadrant that the patient belonged to based on the classification model proposed by the Association for Children with Life-threatening or Terminal Conditions and their Families (ACT)11 (Table 1).
Table 1.Classification by clinical course of disease of the Association for Children with Life-threatening or Terminal Conditions and their Families.
Group I Life-threatening conditions for which curative treatment may be feasible (such as cancer) Group II Conditions where premature death is inevitable but preceded by long periods of intensive treatment to prolong life (cystic fibrosis, HIV infection, Duchenne muscular dystrophy, etc.) Group III Progressive conditions without curative treatment options that may extend over many years (neurodegenerative diseases, polymalformative syndromes, etc.) Group IV Irreversible but non-progressive conditions that may lead to premature death and associated with significant comorbidities (cerebral palsy) - •
Characteristics of the admission: main reason for admission (respiratory, neurologic, surgical intervention, gastrointestinal, metabolic decompensation, assessment of care needs, imminent death or other); point of patient origin (referral and transfer yes/no, and if transferred, referring facility), length of stay (days), death during admission (yes/no). In patients admitted more than once, we also documented whether the admission was a readmission (admission within 30 days from previous discharge), differentiating between early readmission (<8 days from discharge) and late readmission (8–30 days after discharge).
We made a descriptive analysis of the data using the software IBM SPSS Statistics® version 22 for Macintosh. We have summarised the data as absolute and relative (%) frequencies. To describe the data, we calculated the median, interquartile range (IQR) and range. We compared quantitative variables using the Student t test.
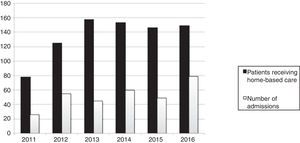
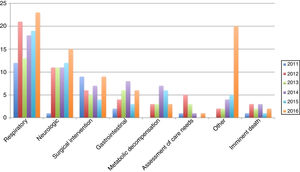
ResultsCharacteristics of hospital admissions: 1 out of 3 patients in followup required admissionIn the period under study, out of the total of 499 patients managed by the PPC unit, 166 (33%) were admitted to hospital at least once, for a total of 314 admissions. In relation to the number of patients receiving home-based care from the unit (Fig. 1), we found an increase in the number of admissions compared to the first year under analysis that paralleled the increase in the number of patients receiving home-based care.
Table 2 summarises the characteristics of the patients. We found that 93 were male and that there were 204 admissions in this group (male sex, 60% of patients and 65% of admissions). We did not find significant differences (P<.05) in the frequency of admission between male and female patients. The age range was 25 days to 28 years and 1 month; the median age was 8 years and 3 months (IQR, 2 years and 3 months–14 years and 3 months).
Characteristics of admissions.
| n | % | |
|---|---|---|
| Patient sex | ||
| Male | 204 | 65 |
| Female | 110 | 35 |
| Patient age | ||
| <1 month | 1 | 0.3 |
| 1 month to 1 year | 31 | 9.8 |
| 1 year to 2 years | 29 | 9.2 |
| 2 years to 5 years | 52 | 16.6 |
| 5 years to 12 years | 98 | 31.2 |
| 12 years to 18 years | 74 | 23.6 |
| >18 years | 29 | 9.2 |
| ACT group | ||
| I | 20 | 7 |
| II | 3 | 1 |
| III | 89 | 28 |
| IV | 202 | 64 |
| Length of stay in days | ||
| <7 | 185 | 58.9 |
| 7–15 | 92 | 29.3 |
| 16–20 | 12 | 3.8 |
| 21–30 | 16 | 5.1 |
| ≥31 | 9 | 2.9 |
| Admissions per patient | ||
| 1 admission | 101 | 60.8 |
| 2 admissions | 34 | 20.5 |
| 3 admissions | 11 | 6.6 |
| 4 admissions | 9 | 5.4 |
| 5 admissions | 2 | 1.2 |
| 6 admissions | 5 | 3 |
| 7 admissions | 1 | 0.6 |
| 8 admissions | 1 | 0.6 |
| 9 admissions | 1 | 0.6 |
| 12 admissions | 1 | 0.6 |
Based on the ACT classification, the group of conditions corresponding to the greatest number of admissions was group IV (64%), followed by group III (28%). Only 7% corresponded to group I, and only 3 admissions corresponded to a patient in group II.
When it came to the number of admissions per patient, 87% of patients were admitted 3 or fewer times, and 60.8% only once. The median number of admissions in patients admitted at least once was 1 (IQR, 1–2). There were 26 readmissions, amounting to 8.2% of total admissions. Of these readmissions, 9 were early (<8 days post discharge) and 17 late (between 8–30 days post discharge). In 14 cases (6 early and 14 late), the patient was readmitted for the same reason that prompted the previous admission. The median length of stay was 5 days (IQR, 3–11; range, 1–195). The length of stay was of 15 days or less in 88% of admissions and shorter than 7 days in 59%. Of the 314 admissions, 25 (8%) lasted more than 3 weeks.
Clinical characteristics of hospital admissions: a predominance of admissions due to respiratory and neurologic conditionsRespiratory problems were the most frequent reason for admission (34%, Fig. 2), both overall and in each year under study (Fig. 3), followed by neurologic conditions (19%). There was an increase through the years in the number of admissions classified as “other”, which eventually became the second largest group in 2016. In this group, the main reason for admission was to offer relief to caregivers (11 patients), followed by pain management (7 patients) and cardiovascular complications (4 patients).
Of all admissions, 33.4% corresponded to patients transferred from other departments in the hospital (Table 3). The most frequent departments of origin were paediatric surgery (23 admissions), paediatric intensive care (22 admissions) and paediatrics (21 admissions). Two patients were transferred from other hospitals to ensure continuity of care.
Point of origin for admissions following transfer from other departments or facilities.
| Referral from other departments or facilities (%) | ||
|---|---|---|
| Not referred by other departments | 210 | (66.8) |
| Other hospitals | 2 | (0.3) |
| Paediatric surgery | 23 | (7.3) |
| Intensive care | 22 | (7) |
| Paediatrics | 21 | (6.6) |
| Traumatology | 14 | (4.4) |
| Neurology | 10 | (3.1) |
| Neurosurgery | 5 | (1.6) |
| Oncology | 4 | (1.3) |
| Gastroenterology | 3 | (0.19) |
| Pulmonology | 1 | (0.3) |
In the period under study, 40 admissions were made to carry out surgical interventions: 23/40 for performance of gastrostomy, 9/40 for orthopaedic surgery and 5/40 for placement of an intrathecal baclofen pump.
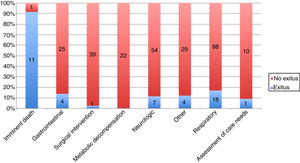
Death during hospitalisation: 20% of patients admitted through the PPC unit died during hospitalisationA total of 46 patients died while hospitalised. This corresponds to 14% of the total number of admissions, 27% of the patients admitted at least once during the period under study, and 20% of the patients managed by the PPC unit that died during the same period. In absolute terms, the group with the highest number of deaths corresponded to patients admitted for respiratory problems (18/46; 17% of patients in this group). Twelve patients were admitted because the PPC team realised they were nearing death (Fig. 4). One of these patients was finally moved to the home at the end of life. Thus, 11 out of these 12 patients died during hospitalisation.
DiscussionIn this article, we present the data corresponding to hospital admissions initiated from the PPC unit of the Community of Madrid, located at the HIUNJ children's hospital. To the best of our knowledge, this is the first study analysing the characteristics of hospital admissions made through a PPC unit in Spain. In our study, we found that 1 out of every 3 patients managed by the PPC unit was admitted at least once, with a length of stay of less than 15 days in nearly 90% of cases. The most frequent reasons for admission were neurologic conditions (groups III and IV of the ACT) and miscellaneous reasons, most frequently respiratory problems. Only 27 of admitted patients (20% of all patients managed by the PPC unit in the period under study) died while hospitalised.
From an epidemiological perspective, we found a predominance of the male sex and a heterogeneous age distribution. The low frequency of admissions in newborns aged less than 1 month, in spite of the fact that they are the age group corresponding to 50% of patients with expected deaths,15 can be largely attributed to the fact that most of these patients remain hospitalised in neonatal units. Furthermore, 9.2% of admissions occurred in patients aged more than 18 years. This can be explained by the presence in young adults of diseases whose characteristics (diagnosis in childhood, clinical course etc.) require care and management in the speciality of paediatrics.4 In relation to this, we ought to highlight that 39% of the patients ever admitted were admitted more than once, with a readmission rate that was similar to the rates reported in previous studies.12,13
Most patients had conditions in groups IV and III of the ACT classification. These groups mostly corresponded to patients with severe neurologic disease, often with chronic respiratory or gastrointestinal comorbidities and/or dependent on medical devices (home ventilatory support, artificial enteral nutrition, etc.). In contrast, while based on internal records of the PPC unit approximately 30% of our patients had some form of cancer and would therefore be included in group I, only 7% of admissions corresponded to this group. There are different possible explanations for this finding, ranging from patients being admitted to the department of oncology and receiving coordinating care from both this department and PPC, to a lower duration of followup by the PPC unit in these patients, which would account for the lower probability of requiring admission through the PPC unit. At any rate, the data collected in this study does not suffice to establish the reason. As for the low frequency of admissions corresponding to group II, our unit has only managed 8 patients in this category. Many of the conditions included in this group (AIDS, cystic fibrosis, etc.) have higher survival rates in developed countries due to the existence of treatments that delay disease progression.
The most frequent reasons for admission (Figs. 2 and 3) were respiratory and neurologic conditions, and corresponded to problems common in patients with severe neurologic impairment, which was consistent with the findings of previous studies.14–16 Additional studies would be needed to obtain details on the specific reasons for admission within each category and the care needs for each admission, especially in the most frequent groups, such as patients with respiratory problems. In the group of admissions made to perform surgery, the most frequent intervention was performance of gastrostomy, associated with one of the devices used most frequently in the delivery of PPC12,17 both to prevent potential admissions due to respiratory infections15 and possibly to improve symptom control and quality of life in patients with dysphagia, although the evidence on the latter aspect is still not definitive.
We ought to highlight the increase of admissions for “other reasons” in 2016 (Fig. 3). Within this category, the most frequent reasons for admission were pain management and offering respite to caregivers. This changing trend could be associated with an increased complexity of symptom management or in the health condition of the patients. Establishing this would require an analysis of this trend in subsequent years. We ought to mention that hospital admissions due to respiratory problems18 could be prevented if there were specific structures, such as hospice services, to care for these patients at the end of life.9 At the time of this writing, there is no facility in Spain meeting the necessary criteria to operate as a paediatric hospice.
When it came to the length of stay and the readmission rate, we found that the median and IQR were similar compared to those corresponding to the Paediatric Chronic Complex Disease Unit of the Hospital Infantil La Paz,17 which manages patients of similar characteristics and where the median length of stay was 6 days (IQR, 3–14 days). Additional studies are required to analyse the factors associated to the length of stay and the measures that could be implemented to reduce it.12 The availability after discharge of continuous care services19 and telemedicine tools20,21 could enable an earlier discharge of patients.
Our analysis of the referral of patients from other departments found that one third of patients had been transferred from elsewhere in the hospital (Table 3). Referrals from paediatric surgery occurred in the context of postoperative care following gastrostomy. The possibility of facilitating the transition between intensive care and palliative care and adjust the management as needed was the subject of a previous study1 of the activity of our unit in collaboration with intensive care units in the Community of Madrid. In the study presented here we did not analyse whether patients had been managed in the PPC unit before being admitted to these other departments or these other departments were the initial point of contact between the patients and the PPC unit. We also did not analyse data on admissions to other units of the hospital or to departments or units in other facilities in which the PPC unit may have been involved as a source of support. This type of information would be needed to analyse the overall care received by these patients, although the objective of our study was to describe the delivery of care in admissions initiated from the PPC unit.
As for the place of death (Fig. 4), although the home has been identified as the most suitable setting for a patient's death,22,23 previous studies have found a higher frequency of deaths in hospital.24 Death at home seems to facilitate the grieving process in the family, reducing the need for psychological and social support.25 Overall, and contrary to the evidence in the previous literature, the deaths in hospital of patients admitted through the PPC unit amounted to only 20% of the total deaths in patients managed by the unit. This is an encouraging finding that highlights the usefulness of PPC units, although a significant number of patients could have died in other hospital departments or even in other hospitals. Based on our experience, the availability of an interdisciplinary team that includes mental health and social work professionals is one of the key elements needed to offer integrated and comprehensive care to these patients and to promote the home and the family as the main setting and unit for care delivery.8 However, we would need to collect data on the exact place of death of all other patients managed at the PPC unit to adequately describe and analyse this variable.
There are significant limitations to this study. It had a retrospective design based on the collection of data from documentation in the PPC unit and other health records, so that data relevant to the analysis may be missing. Since there was no control group to compare the data to, we could not determine which of the observed outcomes (admission rate, length of stay, etc.) could be improved. We mostly collected data on clinical and administrative aspects that do not reflect the social and emotional component of these conditions. Furthermore, we obtained overall data, as opposed to specific data for each admission based on patient characteristics. In previous studies, the length of stay seems to vary based on the health condition affecting the patient,26 with longer stays in patients with oncological or neuromuscular disease,16 especially in cases with multiple organ or system involvement. Taking into account that groups III and IV of the ACT correspond to patients with severe neurologic impairment and group I to patients with cancer and that 99% of our patients belonged in these categories, we were unable to establish a control group. Although we did not analyse the impact of factors mentioned above (hospital at home, continuous care, telemedicine etc.), the observed lengths of stay were consistent with the standards for acute care units of the European Association of Palliative Care.8 We did not compare endpoints by age group, as we were unable to correct for confounders that also influence the rate of admission, and age could be a determinant, as patients aged less than 1 year may be more likely to be admitted at the end of life compared to all other age groups.24 We excluded data corresponding to the first 4 years of activity of the PPC unit to avoid including data of the time when the unit was starting its operations so that the findings would reflect the characteristics of the unit once it was fully established. In spite of this, the number of admissions grew over the study period along with the number of patients managed by the PPC unit. Several factors may be at play in this, such as increased coverage by the PPC unit within the Community of Madrid or the changing medical complexity of its patients. The data in our study did not allow us to analyse these phenomena. In the categorization by reason for admission, we were unable to determine whether the documented reason was ultimately the main problem managed during hospitalisation or just the initial reason for admission. Based on our experience, the reason why a patient remains hospitalised often changes in the course of the hospitalisation, and lengths of stay and the use of resources may vary over time.
The findings of our study may not be generalisable to other settings. Further research is needed to analyse the characteristics of patients of similar medical complexity to be able to customise care to their individual needs. Regional studies are required in Spain to establish the characteristics of the population that would benefit from PPC, the current coverage of these services and the resources available to each palliative care delivery system.5 The inclusion of mental health and social work professionals in health care teams should be addressed directly, as the availability of these services may be crucial to allow establishing the home as the main care setting.14
ConclusionThe institution of PPC units must conform to the specific needs of these patients. This study is the first to contribute data corresponding to the inpatient activity of a specialised PPC unit in Spain. Our study found that only 1 out of 3 patients managed in the PPC unit required hospitalisation, and that lengths of stay were generally short. The most frequent reason for admission was respiratory disease. Only 20% of patients managed by the PPC unit in the period under study died during hospitalisation. Multicentric studies are required to identify and analyse the benefits of PPC units to patients and opportunities for improvement.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the staff employed at present and in previous years in the Paediatric Palliative Care Unit and the rest of the staff of the Hospital Infantil Universitario Niño Jesús for contributing to the care of our patients, and also our patients and their families for allowing us to be part of their lives, at hospital and in their homes.
Please cite this article as: de Noriega Í, Barceló M, Pérez MÁ, Puertas V, García-Salido A, Martino R. Ingresos hospitalarios en cuidados paliativos pediátricos: estudio retrospectivo. An Pediatr (Barc). 2020;92:94–101.