Eosinophilic gastroenteritis (EGE) is a rare type of gastroenteritis characterised by eosinophilic inflammation in different segments of the GI tract in the absence of known causes for eosinophilia (parasitic infestation, drug toxicity, malignancy, inflammatory bowel disease or hypereosinophilic syndrome, among others).1
The clinical manifestations of EGE are nonspecific and vary based on the location and the depth of eosinophilic infiltration in the layers of the gastrointestinal tract, and may include chronic abdominal pain, vomiting, upper or lower gastrointestinal bleeding, diarrhoea and/or ascites.2 Its aetiology and pathophysiology is not understood, although they seem to be involve hypersensitivity mechanisms, and the antigen involved most frequently in infants is cow's milk protein (CMP).3,4 The diagnosis is confirmed by histological examination, and at present there is no established threshold for the definition of eosinophilia in the gastrointestinal tract.2,4,5
Eosinophilic gastroenteritis is rare in infants and its presentation can vary widely, so diagnosis requires a high level of suspicion. In patients that present with upper gastrointestinal bleeding, the disease may range from mild forms that are well tolerated to severe forms leading to anaemia or haemodynamic instability that may require transfusions. We present the cases of two infants with eosinophilic gastroenteritis and gastritis managed in our hospital.
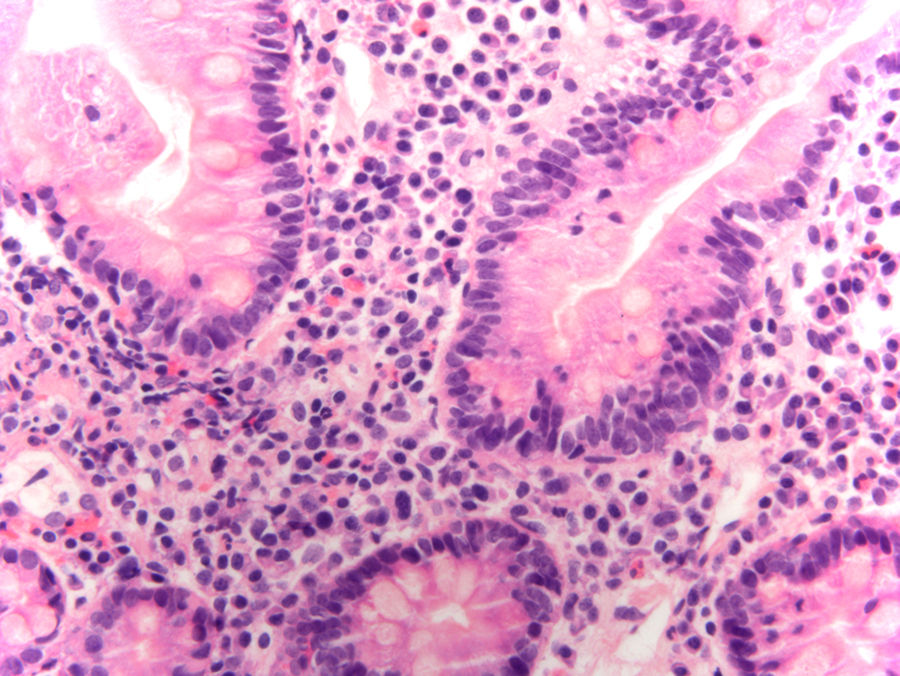
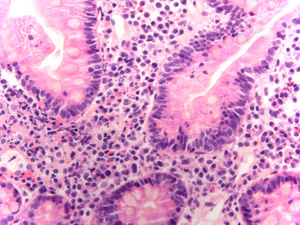
Case 1: infant aged 4 months, previously healthy, who in the context of acute gastroenteritis had three episodes of vomiting with presence of coagulated blood in the vomit. He had not received ibuprofen and had been fed infant formula since age 1 month. At the time of evaluation, he was in good general health with normal vital signs. He had several eczematous lesions in the trunk and retroauricular area. The complete blood count revealed a haemoglobin concentration of 11.2g/dL, a white blood cell count of 18800cells/mm3 (18.9% neutrophils, 56.4% lymphocytes, 22.8% monocytes, 1.8% eosinophils, 0.1% basophils) and a platelet count of 283000/mm3. The abdominal ultrasound findings were normal. Fresh blood was found on gastric suction, and oesophagogastroduodenoscopy revealed erosions in the antral mucosa and diffuse fibrin-coated lesions in the gastric body and a pale duodenal mucosa. Histological examination (Fig. 1) revealed a significant although heterogeneous eosinophilic component in the duodenal mucosa (>20 eosinophils/high power field [HPF] with focal involvement) and a mixed inflammatory cellular infiltrate in the gastric mucosa that included abundant eosinophils (25–30 eosinophils/HPF). The infant was managed by switching to elemental formula, to which he showed a favourable response. Allergen-specific IgE testing detected low titres of antibodies against CMP (casein, 0.44kIU/L; β-lactoglobulin, 0.24kIU/L, α-lactalbumin, 0.12kIU/L). Followup: from age 12 months, CMP was progressively reintroduced in the diet without negative repercussions.
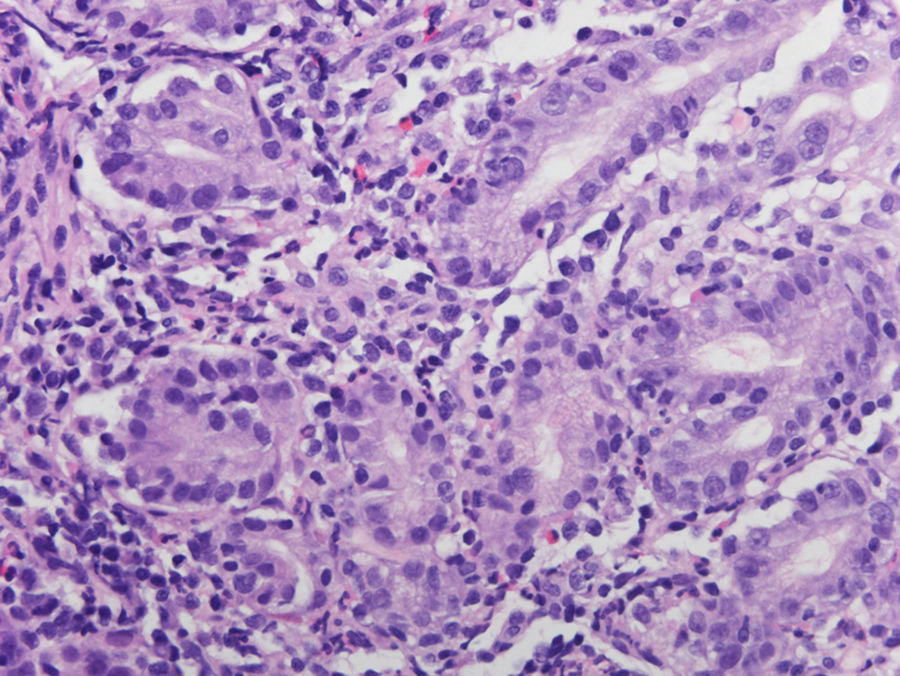
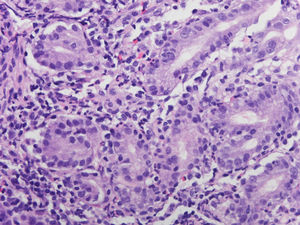
Case 2: infant aged 2 months, previously healthy, who had three episodes of vomiting with fresh blood and a darker-than-normal bowel movement the day before evaluation. She presented with urticarial-like lesions in the lower extremities that had developed 24h earlier, which she had also exhibited transiently at age 1 month. The patient had been formula-fed from birth. She was in good general health at the time of physical examination, whose salient findings were a marked paleness of the skin and mucosae and a red and swollen exanthema in the lower extremities that was spreading to the upper limbs. Auscultation of heart sounds revealed tachycardia, with 165 beats per minute, and a mild systolic murmur. The findings of the complete blood count were: haemoglobin concentration of 6.5g/dL, white blood cell count of 16700cells/mm3 (24.2% neutrophils, 61.3% lymphocytes, 13.5% monocytes, 0.7% eosinophils, 0.3% basophils) and 338000platelets/mm3, with normal features in the peripheral blood smear. The results of the blood chemistry and coagulation panel were normal, and haematuria was not detected in the urine test strip. The patient underwent gastric lavage and suction, and blood was not found in the recovered contents. Since the loss of blood had caused haemodynamic instability, the patient received a transfusion of packed red blood cells, which led to improvement of symptoms and laboratory parameters. Oesophagogastroduodenoscopy revealed diffuse erythema and multiple fibrinous lesions in the gastric mucosa and a normal duodenal mucosa. Biopsy examination revealed superficial gastritis and a mixed inflammatory cell infiltrate with a predominance of eosinophils, with up to 30 eosinophils/HPF (Fig. 2). The patient was switched to an exclusive diet of elemental formula, with resolution of symptoms. Allergen-specific IgE testing detected antibodies against CMP (casein, 1.24kIU/L; β-lactoglobulin, 2.82kIU/L; α-lactalbumin, 0.14kIU/L; cow's milk, 3.69kIU/L). Followup: the patient is still keeping a CMP-free diet, which is well tolerated.
The two patients whose cases we present here had onset during infancy with upper gastrointestinal bleeding and a different degree of haemodynamic impact, and received final diagnoses of eosinophilic gastroenteritis and eosinophilic gastritis, respectively. Recently, Choi et al.4 published a study assessing the clinical, endoscopic and histologic features and the response to treatment of 13 children with a histological diagnosis of EGE. They found that the most prevalent symptom at onset in the infant group (8 patients) was haematemesis (7 patients, 87.5%), followed by melena (2 patients, 25%). In contrast, recurrent abdominal pain was the predominant symptom in the group of children aged more than 1 year (60%). Furthermore, CMP was the allergen most frequently suspected to be involved based on the clinical manifestations, suspected in 76.9% of patients, and all infants in this study responded favourably to switching from cow's milk to extensively hydrolysed/elemental formula. These findings are consistent with the outcomes of the two patients managed in our hospital, although it is important to keep in mind that absence of peripheral eosinophilia or negative results of specific IgE assays are not sufficient to exclude a diagnosis of EGE.1,2
Please cite this article as: Soriano-Ramos M, Salcedo Lobato E, Rodríguez Gil Y, Medina Benítez E, Urruzuno Tellería P. Hematemesis como debut de gastroenteritis eosinofílica en lactantes. An Pediatr (Barc). 2018;88:351–353.