Haemophilia is a rare disease and its management can pose a challenge to Emergency Department paediatricians.
AimTo describe the frequency and reasons for consultation by haemophilic children in the ED.
Materials and methodsLongitudinal retrospective study was conducted in a paediatric Emergency Department of a tertiary care hospital. The study included haemophiliacs A and B, ages 0 to 16 years old, and who had consulted the Emergency Department for whatever reason over a span of 6 years (2011–2016). The data analysed include: age, type and severity of haemophilia, reason for query, prophylactic status, complementary examinations, established diagnosis, treatment, and number of visits to the Emergency Department.
ResultsThe analysis included 116 males with a total of 604 Emergency Department visits. The mean age was 5.5 years, and the median age was 5.3 years. A total of 101 patients were categorised as haemophiliac A (38 mild, 4 moderate, 59 severe), and 15 as haemophiliac B (9 mild, 3 moderate, 3 severe). The main reasons for initial Emergency Department visits (ranked by triage) were: musculoskeletal problems/injury or bleeding (66.7%), causes unrelated to haemophilia (29%), suspected central venous catheter related infection (2.8%), and routine clotting factor infusion (1.5%). Additional tests were conducted during 335 visits (55.5%). Factor replacement was undertaken in 317 visits (52.5%). A total of 103 episodes (17.1%) required hospital admission, due to: head trauma (35.9%), central venous catheter -related infection (13.6%), haemarthrosis (8.7%), muscle haematoma (6.8%), and haematuria (5.8%).
ConclusionHaemophilic patients went to the Emergency Department for common paediatric causes, but also requested consultation on specific problems related to haemophilia, with musculoskeletal problems/injury or bleeding being the main issues. The paediatric Emergency Department is an indispensable component of haemophilia care.
La hemofilia es una enfermedad rara, por lo que su abordaje en Urgencias puede suponer un reto para los pediatras.
ObjetivosDescribir la frecuencia y motivos de consulta de los niños hemofílicos en Urgencias.
Material y métodosEstudio retrospectivo longitudinal realizado en Urgencias Pediátricas de un hospital de tercer nivel. Se incluyeron hemofílicos A y B, desde el nacimiento hasta los 16 años, que consultaron por cualquier motivo durante 6 años (2011-2016). Se analizaron: edad, tipo y gravedad de hemofilia, motivo de consulta, profilaxis domiciliaria frente a sangrados, pruebas complementarias, diagnóstico establecido, tratamiento y número de visitas a Urgencias.
ResultadosSe analizaron 116 varones con un total de 604 visitas. La media de edad fue de 5,5 años y la mediana de 5,3. De ellos, 101 pacientes eran hemofílicos A (38 leves, 4 moderados, 59 graves) y 15 hemofílicos B (9 leves, 3 moderados, 3 graves). Los principales motivos de consulta (clasificados en triaje) fueron: problema musculoesquelético/traumático o sangrado (66,7%), causas no relacionadas con hemofilia (29%), sospecha de infección de catéter central (2,8%) y administración rutinaria de factor (1,5%). Se realizaron pruebas complementarias en 335 visitas (55,5%). Del total, 317 consultas (52,5%) requirieron factor; 103 episodios (17,1%) precisaron ingreso, cuyos principales motivos fueron: traumatismo craneoencefálico (35,9%), infección de catéter venoso central (13,6%), hemartrosis (8,7%), hematoma muscular (6,8%) y hematuria (5,8%).
ConclusiónLos pacientes consultaron por causas habituales de la edad pediátrica, pero también lo hicieron por motivos específicos de su enfermedad; lo más frecuente fue el problema musculoesquelético/traumático o sangrado. El Servicio de Urgencias es un componente indispensable en su atención.
Haemophilia is an inherited disorder affecting coagulation. It results from the deficiency or impaired function of clotting factor VIII (haemophilia A) or factor IX (haemophilia B). The incidence is 1/5000 in the case of haemophilia A and 1/30000 in case of haemophilia B; severe forms of disease are more prevalent in type A. Haemophilia is inherited in a recessive X-linked pattern, although one third of mutations are de novo.1–3
The clinical presentation is the same in both forms of haemophilia. The characteristic manifestations are joint and muscle bleeds, and one of the most serious ones is intracranial haemorrhage, which is less frequent compared to bleeding in other areas but is associated with significant morbidity and mortality. In case of potential bleeding, early administration of factor replacement therapy is essential.
At present, the main interventions for treatment and prophylaxis of episodes of potential bleeding are delivered in haematology units or even at home, but there are instances in which patients seek care in the emergency department, where their management may pose challenges.4–8
Previous studies have analysed the frequency of emergency department visits by haemophilic children, including those published by Morgan et al. in 1993,5 Nuss et al. in 20026 and, more recently, Özgönenel et al. in 2013,7 all of which highlighted the importance of the emergency department in their care.
The main aim of our study was to describe the main reasons haemophilic patients visited our emergency department and their clinical characteristics, in addition to analysing the diagnostic tests performed, aspects related to home prophylaxis and treatment, number of visits per patient and overall management of these patients in the emergency department.
Materials and methodsWe conducted a retrospective observational study in the paediatric emergency department of a tertiary care university hospital that has a comprehensive haemophilia treatment centre. We included male patients with a diagnosis of haemophilia A or B aged 0 days to 16 years that visited the emergency department during a 6-year period (January 2011–December 2016). All patients had a previous diagnosis of haemophilia.
We identified patients searching the coding system of our hospital. We performed an exhaustive collection of data by reviewing the electronic health records of these patients, including the age, type and severity of haemophilia, reason for the emergency visit, home prophylaxis with factor, diagnostic tests, final diagnosis, treatment and total number of emergency visits. The study was assessed and approved by the ethics committee of our hospital.
We classified the severity of disease according to the level of activity of the factor: mild for an activity of 5% to 40%, moderate for activity between 1% and 5% and severe in case of a level of activity of less than 1%.
We classified emergency visits in 4 categories according to whether they were related to: (1) musculoskeletal problem/trauma or bleeding; (2) suspected central venous catheter-related infection central; (3) routine factor infusion and (4) common paediatric complaints unrelated to haemophilia.
We have summarised quantitative data as mean±standard deviation, median and interquartile range. We have described qualitative data as absolute frequencies and percentages.
ResultsStudy sampleWe analysed 604 visits made during the period under study corresponding to 116 children aged 7 days to 15.14 years (mean, de 5.5 years; median, 5.3 years).
As for the type and severity of disease, 101 patients (87.1%) had a diagnosis of haemophilia and 15 (12.9%) of haemophilia B. In the group of patients with haemophilia A, 38 had mild disease (32.8%), 4 moderate disease (3.4%) and 59 severe disease (50.9%). Of the patients with haemophilia B, 9 had mild disease (7.7%), 3 moderate disease (2.6%) and 3 severe disease (2.6%). There were 6 patients with inhibitors, 5 of who had severe haemophilia A and 1 mild haemophilia A.
Emergency visitsThe mean number of emergency visits per patient was 5.2. The patient that sought care most frequently made 26 visits; 34 patients made 1 visit, 16 made 2 visits, 11 made 3 visits, 8 made 4 visits, 8 made 5 visits and the rest visited the emergency department more than 5 times.
Children with haemophilia A made 91.1% of all visits, while patients with haemophilia B made 8.9%. When it came to the distribution by severity of disease, 56% of visits corresponded to severe forms of haemophilia, 4.6% to moderate forms and 39.4% to mild forms. Patients with inhibitors made 44 visits (7.28% of the total).
The main reasons for visiting the emergency department (documented during triage on arrival to the department) were the following: musculoskeletal problem/trauma or bleeding in 66.7% (n=403), suspected central venous catheter-related infection in 2.8% (n=17) and routine factor infusion in 1.5% (n=9). In addition, 29% of emergency visits (n=175) were due to common paediatric complaints unrelated to haemophilia (such as diarrhoea, difficulty breathing and pharyngitis). The 6 patients with inhibitors experienced 15 episodes of bleeding. Table 1 presents the reasons for emergency department visits distributed by age group.
Diagnostic testsOut of all visits, 335 required some type of diagnostic test. Blood tests were performed in 80 visits (13.2%), urinalysis in 16 (2.6%), stool tests in 9 (1.5%) and culture of throat swab or respiratory secretion samples in 19 (3.1%). Imaging tests were performed in 266 visits (44%): musculoskeletal ultrasound examination in 134 (22.2%), musculoskeletal radiographs in 81 (13.4%), head computed tomography (CT) scans in 36 (6%), chest radiographs in 17 (2.8%), abdominal ultrasound in 19 (3.1%), cranial radiograph in 14 (2.3%), abdominal CT scan in 1 (0.2%), neck radiograph in 1 and neck CT scan in 1 (0.2%).
Assessment of intracranial haemorrhage: head computed tomographyA head CT scan was performed in 36 visits (corresponding to 31 cases of head trauma, 1 case of polytrauma, 1 patient with afebrile convulsive seizures and 3 patients with persistent vomiting). There was evidence of intracranial bleeding in 7 cases (1.16% of the total visits): subdural haematoma in 5 (in 4 patients following head trauma and in 1 patient with persistent vomiting) and epidural haematoma in 2 (in both cases following head trauma). Table 2 presents a brief summary of the cases of intracranial haemorrhage secondary to trauma. In all cases, patients received factor on arrival to the emergency department and before performance of imaging tests. Only 1 of these patients required surgical intervention.
Patients with head trauma and intracranial haemorrhage.
| Age (years) | Type of haemophilia | PX | Mechanism | Symptoms | Head CT | Management | |
|---|---|---|---|---|---|---|---|
| 1 | 4.05 | SHA | Yes | Fall from 0.5m | Headache | Subdural haematoma | FactorAdmission to ward |
| 2 | 8.91 | MHA | No | Impact with pole | Headache | Subdural haematoma | FactorAdmission to ward |
| 3 | 3.49 | MHB | No | Fall from 17m | Sleepiness | Epidural haematoma and fracture | FactorCraniectomy and drainage of haematoma |
| 4 | 1.24 | SHA | Yes | Fall from 0.3m | Vomiting | Subdural haematoma | FactorAdmission to ward |
| 5 | 14.52 | SHA | Yes | Frontal impact with object | Blurred vision | Subdural haematoma | Admission to ward |
| 6 | 6.37 | MoHA | No | Bicycle fall | Vomiting, sleepiness | Epidural haematoma | FactorAdmission to PICU (did not require surgery) |
MHA, mild haemophilia A; MoHA, moderate haemophilia A; MHB, mild haemophilia B; PICU, paediatric intensive care unit; PX, prophylaxis; SHA, severe haemophilia A.
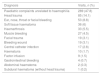
Table 3 presents the most frequent diagnoses made after the evaluation at the emergency department. In 47.8% of visits, the diagnosis at the time of discharge or admission to hospital was unrelated to haemophilia.
Diagnoses in the emergency department.
| Diagnosis | Visits, n (%) |
|---|---|
| Paediatric complaints unrelated to haemophilia | 289 (47.8) |
| Head trauma | 85 (14.1) |
| Ear, nose, throat or facial bleeding | 53 (8.8) |
| Soft tissue haematoma | 36 (6) |
| Haemarthrosis | 33 (5.5) |
| Muscle bleeding | 27 (4.5) |
| Facial trauma | 19 (3.1) |
| Bleeding wound | 19 (3.1) |
| Central catheter infection | 17 (2.8) |
| Haematuria | 10 (1.7) |
| Factor infusion | 9 (1.5) |
| Gastrointestinal bleeding | 4 (0.7) |
| Abdominal haematoma | 2 (0.3) |
| Subdural haematoma (without head trauma) | 1 (0.2) |
Haemarthrosis was diagnosed in 33 episodes (5.5%) and muscle bleeding in 27 (4.5%) (in 1 case manifesting with compartment syndrome). In 27.3% cases of haemarthrosis and 22.2% of muscle bleeding, the patient required admission to hospital.
Central venous catheter-related infectionThere were 14 episodes (2.3% of visits) if central venous catheter-related infection with microbiological confirmation; gram-positive bacteria were isolated in 1% of cases and the catheter had to be removed in 7 cases (50%).
General management in emergency departmentOf all visits, 51.2% corresponded to patients undergoing factor replacement therapy at home for prophylaxis of bleeding episodes (n=309). As for treatment, 317 visits (52.5%) were made by patients that required administration of clotting factor, prescribed in consultation with the Department of Haematology. After the evaluation in the emergency department, 501 visits (82.9%) ended in discharge home, while 103 (17.1%) led to hospital admission. The main reasons for admission were head trauma (35.9%), central venous catheter-related infection (13.6%), hemarthrosis (8.7%), muscle bleeding (6.8%), haematuria (5.8%), soft tissue haematoma (2.9%), ear-nose-throat bleeding (2.9%), gastrointestinal bleeding (2.9%), fracture (2.9%), facial trauma (1.9%) and abdominal haematoma (1.9%). Another 12.6% of admissions were for reasons unrelated to haemophilia (pneumonia, bronchiolitis, appendicitis etc.). One patient was admitted after detection of intracranial bleeding in the absence of previous trauma (1%).
DiscussionGeneral aspectsPatients with haemophilia visit the emergency department frequently for different reasons, including common paediatric complaints and specific problems secondary to their disease, so this setting constitutes an indispensable component in their management.
The register of haemophilic patients in our hospital (the reference centre for haemophilia) includes at least 600 children with this disease. Most of them are managed exclusively in our hospital, although a smaller percentage are followed up in other hospitals and come to our hospital for evaluations every 6 months or yearly. In urgent or emergent situations (especially in cases related to trauma or bleeding), patients can visit the Department of Haematology, and after hours they usually seek care in the emergency department. In addition, referral to the emergency department may be useful if diagnostic tests need to be performed.
Previous studies have analysed the frequency of emergency department visits made by children with haemophilia. In 1993, Morgan et al. published a study conducted in 36 children with haemophilia, who made a total of 126 visits to the emergency department of a single hospital over a period of 10 years.5 Later, in 2002, Nuss et al. described 35 emergency visits made by haemophilic patients (paediatric and adult) made in a 1-year period to 25 hospitals.6 The most recent study on the subject was published in 2013 by Özgönenel et al., who described 536 emergency visits by 84 patients with haemophilia aged 0–21 years made over a period of 5 years to a single hospital.7 In every instance, the most frequent reasons for the visit were trauma or bleeding, and the authors concluded by highlighting the importance of the emergency department in the management of haemophilic patients and the need for emergency clinicians to be acquainted with the most common problems in these patients.
Between the time of the earliest studies to present, prophylaxis with clotting factor for prevention of potential bleeding episodes has been well established, constituting a significant improvement in the care of these patients. In our sample, 51.2% of episodes (n=309) corresponded to patients receiving home prophylaxis (299 with severe disease, 7 with moderate disease and 7 with mild disease). Patients and caregivers are educated on the disease and the main aspects of prophylaxis and treatment, which is associated with a decrease in morbidity and mortality, although visits to the emergency department continue to be frequent.
Our emergency department is part of a tertiary care hospital that also has a comprehensive haemophilia treatment centre, so the number of visits identified in our study is greater compared to other emergency departments in centres without these specialised services. We have described 604 emergency visits in a period of 6 years, which corresponds to 100.7 visit per year (1 emergency department visit every 3–4 days).
The most frequent reason for the visits (documented during triage) were musculoskeletal problems/trauma or bleeding, in 66.7% of the total (n=403), followed by common complaints unrelated to haemophilia, such as diarrhoea, difficulty breathing, pharyngitis etc. (29%). Trauma or bleeding were also the most frequent reasons for emergency department visits reported in the studies discussed above.5–7
Haemarthrosis and muscle haemorrhageJoint and muscle bleeds are among the most characteristic manifestations of haemophilia. The knees and ankles are the most frequently involved joints, and there is not always a previous traumatic event. The diagnosis of haemarthrosis is based on the data obtained in the history taking and physical examination, and frequently confirmed by ultrasound imaging. Muscle bleeds can be extensive in haemophilic patents and in some cases may even cause compartment syndrome.3 The approach to the management of both consists in early clotting factor replacement therapy. In our sample, 33 episodes (5.5%) were diagnosed as haemarthrosis and 27 (4.5%) as muscle bleed (1 of them with compartment syndrome). Hospital admission was required in 27.3% of cases of haemarthrosis and 22.2% of cases of muscle haemorrhage.
Intracranial haemorrhageIntracranial haemorrhage (the most dangerous form of bleeding in haemophilia) was documented in 7 patients (1.16% of all visits to the emergency department and 19.5% of the total CT scans performed). In patients with haemophilia, this type of bleeding can occur spontaneously (infrequently, save in cases with a recent history of haemorrhage or with anatomical lesions predisposing the patient to haemorrhage) or, more commonly, following trauma to the head.9–11 In our sample, there was only 1 episode of intracranial haemorrhage without previous trauma, which occurred in a patient aged 1 year with persistent vomiting. If intracranial haemorrhage is suspected, the imaging test of choice in the emergency setting is the head CT scan, although it is important to remember that administration of factor should not be delayed.12,13 The recommendation to routinely perform a head CT scan in haemophilic patients that experience head trauma has been the subject of heated debate. In our sample, all patients with intracranial bleeding had symptoms of some form, so we recently published an article proposing to limit the indication of CT to patients who are symptomatic or have some other risk factor. These patients need to remain under observation for longer periods compared to other patients (up to 24h).14
Central venous catheter-related infectionSince home factor replacement prophylaxis is one of the most important advances in the care of haemophilic patients in recent years, many of them have central catheters placed for its administration. These devices are usually inserted starting from age 1 year and the use of this type of catheter is frequent, especially in patients with severe forms of haemophilia. The percentage of haemophilic patients with central catheters that develop related infections has been reported to be as high as 44%.7 Therefore, when a patient with haemophilia with a central catheter presents with fever of unknown source, a catheter-related infection should be suspected and empirical antibiotherapy initiated after obtaining samples for culture. The most frequent pathogens involved in these infections are gram-positive bacteria (such as Staphylococcus aureus or Streptococcus epidermidis), followed by gram-negative bacteria (Pseudomonas aeruginosa, Klebsiella pneumoniae, Escherichia coli) and Candida species.15–17
In our sample, 14 visits (2.3%) corresponded to central venous catheter-related infections confirmed by microbiological testing, with isolation of gram-positive bacteria in 1%; 7 of these patients (50%) required removal of the catheter.
Inhibitor developmentThe most serious complication in patients with severe forms of disease is the development of inhibitors (autoantibodies produced in response to the administered factor that neutralise its activity).18 This occurs in 30% of patients with severe haemophilia A and 3% to 9% of patients with severe haemophilia B. In our sample, we found 6 patients with inhibitors (5 with severe haemophilia A and 1 with mild haemophilia A). Of the 44 visits made by these patients (7.28% of the total), 15 were due to bleeding. Patients with severe disease were receiving prophylactic factor replacement therapy at home, and in the emergency department, bleeding episodes in these patients were treated with bypassing agents.
Care and management of haemophiliaSeveral recommendations have been published for the management of haemophilia in the emergency care setting19,20 that clinicians should be aware of, including consultation with the department of haematology. In our emergency department, there are specific protocols for the management of the most frequent presenting problems of haemophilic patients at the emergency care level (head, abdominal and extremity trauma).21–24
If bleeding is suspected, the missing clotting factor must be administered without delay. The dosage and duration of treatment depends on the type of haemophilia and of bleeding.25,26 The family and caregivers must be educated on this aspect. In general, parents are advised to keep clotting factor at home in case of a potential emergency, and, should trauma or bleeding occur, to administer it as soon as possible (even before going to the emergency department if they are trained in its administration). The staff of the emergency department will try to administer the same factor that the patient uses habitually.
The main limitations of this study were its retrospective design and it being performed in a single centre. Multicentric studies could contribute more information.
ConclusionIn our study, the main reason for seeking emergency care in haemophilic children was musculoskeletal trauma or bleeding (66.7%), followed by common paediatric complaints unrelated to haemophilia (29%). The overall management of haemophilic patients is carried out in specialty clinics with haemophilia units, yet the emergency department is an indispensable component in the care of these patients, and therefore paediatricians should be knowledgeable of the most important complaints in these patients and their management. Treatment of potential bleeding episodes requires prompt infusion of clotting factor and a multidisciplinary approach involving the emergency department paediatrician and a haematologist.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the Department of Statistics of Hospital La Paz.
Please cite this article as: García Sánchez P, Martín Sánchez J, Rivas Pollmar MI, Álvarez Román MT, Jiménez Yuste V. Hemofilia: naturaleza de las visitas a urgencias pediátricas. An Pediatr (Barc). 2019;91:394–400.