Acute cerebellitis (AC) is an inflammatory syndrome that causes acute cerebellar dysfunction (ataxia, nystagmus or dysmetria) often in association with fever, headache, nausea and altered consciousness.1,2 It usually occurs in the context of infection or after infection or vaccination, although there are cases in which a trigger is not identified.3–5
By consensus, cerebellar ataxia is defined as cases with normal neuroimaging, while AC is defined as cases presenting with imaging abnormalities,3 and magnetic resonance imaging (MRI) is the gold standard of diagnosis. Computed tomography (CT) can be useful during the acute phase to rule out other aetiologies and to detect the development of acute hydrocephalus or severe compression of the brainstem.
Acute cerebellitis is an infrequent process and its diagnosis is challenging, as its presentation and course are widely heterogeneous. Early intervention is essential to optimise outcomes, so this disease should be suspected in patients with symptoms suggestive of posterior fossa involvement.
Cerebellar inflammation can lead to compression of the brainstem and cause alterations in the level of consciousness that may mask the initial manifestations of cerebellar involvement, as patients may even present with coma and autonomic dysfunction. This presentation, in which raised intracranial pressure (RICP) symptoms predominate over cerebellar symptoms and associated with significant inflammation, is known as fulminant acute cerebellitis1 and should be considered in the differential diagnosis of patients with RICP of sudden onset.1 This form of disease carries an increased risk of permanent sequelae and even death.1,4,6
Due to the variable natural history of acute cerebellitis, its management needs to be individualised.4 In mild cases without clinical progression or neuroimaging findings suggestive of a fulminant course, a conservative approach with close monitoring may be sufficient. In moderate to severe cases, steroid drugs are the first-line treatment to reduce the mass effect of inflammation, and placement of an external ventricular drain (EVD) may be necessary to manage hydrocephalus.
We now present the cases of 3 patients aged 7–12 years that received a diagnosis of AC, none of whom had a personal or family history of interest.
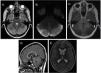
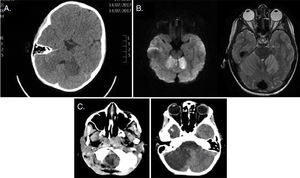
The first patient sought care due to vomiting and malaise, and presented on arrival with vasovagal syndrome, with altered level of consciousness, hypotonia and neurologic impairment. A cranial CT scan was performed, and the images showed hypodensity in the subcortical region of the left cerebellar hemisphere (Fig. 1A). The patient was admitted to the intensive care unit, and a cranial MRI was ordered to make the differential diagnosis between ischaemic injury of the posterior fossa, encephalitis and AC (Fig. 1B), while the patient remained under continuous monitoring (including intracranial pressure) and started treatment with acyclovir and antiplatelet and steroid therapy. At 12h from admission, the patient developed raised intracranial pressure and anisocoria, which led to performance of a cranial CT scan. Based on the results of the scan, we decided to perform a decompressive craniectomy with placement of an EVD, which achieved stabilisation. The patient subsequently started rehabilitation and showed neurologic improvement, although sequelae were still present at the 4-month follow-up evaluation, including dysarthria, hypotonia, inability to stand and right hemiparesis. The follow-up cranial MRI scan revealed that the mass effect had resolved, but also significant cerebellar atrophy.
(A) Cranial CT scan, axial plane: subcortical hypodensity in left cerebellar hemisphere with nonspecific appearance. (B) Head MRI, T2-weighted axial view: hyperintensity in both cerebellar hemispheres with restricted diffusion and cortical enhancement after administration of contrast. (C) Cranial CT scan, axial plane: evidence of progression of cerebellar ischaemia associated with swelling and mass effect and with descent of the cerebellar tonsils to the foramen magnum and raised supratentorial ventricle.
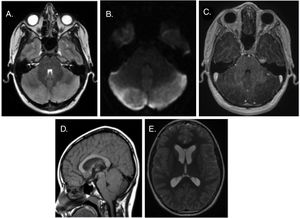
The second and third patients both sought care for headache of approximately a week's duration that had intensified, interfering with daily activities and disturbing sleep, and accompanied by vomiting. The findings of the physical examination and the CT scan were normal in both, and they were both admitted to hospital for analgesia. Due to lack of response, they underwent evaluation by cranial MRI (Fig. 2), which led to diagnosis of AC. The management of AC consisted of monitoring and steroid therapy. The patients responded well, with improvement of symptoms and no complications, so they were discharged with a prescription for a tapering course of steroids. There was no evidence of sequelae in the follow-up evaluations. The follow-up MRI confirmed the resolution of the mass effect.
Head MRI. (A) T2-weighted axial plane: hyperintensity and swelling in both cerebellar hemispheres. (B) Generalised restricted diffusion. (C) T1-weighted axial view: absence of enhancement after administration of gadolinium contrast. (D) T1-weighted sagittal view: descent of cerebellar tonsils into foramen magnum, anterior displacement of the brainstem and mild caudal compression of the cerebral aqueduct and the fourth ventricle. (E) Secondary supratentorial ventricular dilation.
In the 3 cases described here, symptoms associated with RICP dominated the presentation (headache and vomiting). The method used for diagnosis was MRI. We did not identify a likely aetiology in any case except the first, in which enterovirus was isolated from 2 stool samples. The approach to the management of AC was high-dose steroid therapy in all patients.
In conclusion, fulminant AC requires urgent medical treatment and sometimes surgical intervention. Thus, it is important for clinicians to be knowledgeable of this disease so that they can suspect it and perform an urgent head MRI for diagnosis, which allows early initiation of treatment.
Please cite this article as: Molina Corbacho M, Martín Birlanga F, Sarrión Sos N, Gargallo Tatay P, Tomás Vila M. Cerebelitis aguda fulminante, ¿una entidad infradiagnosticada?. An Pediatr (Barc). 2019;90:188–190.