To study the impact of the economic crisis on the families of the children who attend Primary Health Care and its relationship with their socioeconomic status.
Patients and methodsObservational descriptive study was conducted by analysing the results of 453 questionnaires, given to the parents of children between 1 and 7 years old who attended 4 paediatric clinics in Madrid. The raw data was analysed, and comparisons between groups and multivariate analysis were performed.
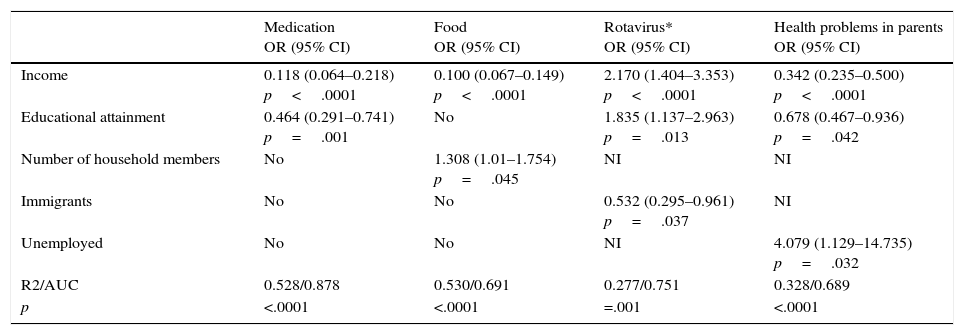
ResultsIn the multivariate analysis, the variables related to the non-acquisition of prescribed medication are: lower income level OR=0.118, p<.0001 and lower educational level OR=0.464, p<.001; the variables related to the reduction of food expenditure are: lower income level OR=0.100, p<.0001 and a higher number of family members OR=1.308, p=.045; the variables related to anti-pneumococcal vaccination without public funding are: higher income level OR=2.170, p=.0001, higher educational level OR=1.835, p=.013, and not being an immigrant OR=0.532, p=.037. The presence of health problems from the beginning of the economic crisis is related to unemployment OR=4.079, p=.032, lower educational level R=0.678, p=.042, and income level OR=0.342, p<.0001. In all cases, the models achieved a statistical significance of p<.0001.
ConclusionsThe economic crisis has greater impact on the group with the lowest income level in all analysed variables. The lower educational level and higher number of family members has an impact on the reduction in food expenditure. The fact of being an immigrant has an impact on not receiving the anti-pneumococcal and rotavirus vaccination. Unemployment leads to an increase in health problems in the family. To sum up, the economic crisis has increased inequalities according to socioeconomic status.
Estudiar el impacto de la crisis económica sobre las familias de los niños que acuden a las consultas de Atención Primaria y su relación con el nivel socioeconómico.
Pacientes y métodosEstudio descriptivo observacional mediante cuestionario. Se han recogido 453 encuestas de niños entre 1 y 7 años de edad pertenecientes a 4 consultas de Atención Primaria de Madrid. Se analizaron datos crudos, comparaciones entre grupos y análisis multivariante.
ResultadosEn el análisis multivariante, las variables relacionadas con no comprar medicamentos prescritos son: tener menor nivel de ingresos OR=0,118 p<0,0001 y de estudios OR=0,464, p=0,001; con la disminución del gasto en alimentación: tener menos ingresos OR=0,100, p<0,0001 y el número de miembros de la familia OR=1,308, p=0,045; con vacunarse frente a rotavirus sin financiación influye el tener mayor nivel de ingresos OR=2,170, p=0,0001 y de estudios OR=1,835, p=0,013 y no ser inmigrante OR=0,532, p=0,037. La presencia de problemas de salud desde la crisis está relacionada con encontrarse en paro OR=4,079, p=0,032 y tener menor nivel de estudios R=0,678, p=0,042 y de ingresos OR=0,342, p<0,0001. En todos los casos los modelos presentaron una significación estadística para p<0,0001.
ConclusionesLa crisis tiene mayor impacto en el grupo con menor nivel de ingresos en todas las variables analizadas. Influye el tener menor nivel de estudios y el número de miembros de la familia en la disminución de gasto en alimentación, el ser inmigrante en la no vacunación por rotavirus y el estar en paro en la presencia de problemas de salud en la familia. En resumen la crisis ha aumentado las desigualdades de acuerdo con el nivel socioeconómico.
The current financial and economic crisis that afflicts Europe, and Spain in particular, officially started in 2008. In January 2009, the Banco Exterior de España announced that Spain had entered a recession1; since then, numerous measures have been taken by governments at the national, regional and local levels, most of them austerity-based, containing and cutting costs in social services.2 Many scientific societies and national and international organisations have warned of the deleterious and counterproductive effects that such measures can have on the welfare and health of society at large and especially of vulnerable collectives.3–7 To date, few studies have provided data on the adverse effects of these measures on child health. Children, along with immigrants and the elderly, are the social collectives most at risk of suffering the negative effects of the crisis.
The relationship between the economic crisis, social inequality and health is complex, and its effects are therefore not clear8; furthermore, what truly matters is the impact on health of the public policies that are being implemented, keeping in mind that chains usually break at their weakest links.
The aim of our study was to analyse the impact of the economic crisis on the individuals receiving care at paediatric primary care (PC) clinics, and study how this impact correlates with the socioeconomic status of their households.
Patients and methodsWe conducted a descriptive observational study, analysing data obtained by means of a survey. The survey was first validated, assessing its reliability (Cronbach's α, 0.749; p<.0001) and construct validity (confirmatory factor analysis and calculation of the item-test correlation coefficient). The survey was administered to a total of 453 children aged 1–7 years that visited the four paediatric clinics of three urban health care centres in Madrid. The total number of children in this age group that were holders of health care cards in the caseloads of these four clinics was 3486, of which a randomly selected sample of the patients that attended a routine or non-routine visit between March and October 2014 was offered to participate; the final sample consisted of all that accepted. Only one patient refused participation in the survey.
We collected the following data: age and sex of the children, age and country of origin of the mother and father, employment status of the parents, and household characteristics. The latter included whether the parents lived together or apart, parental educational attainment, household income level, number of members in the household, perception of having reduced expenditures in food, leisure and vacations or travel, perception of the impact of employment and economic factors in parental health, financial difficulty in acquiring prescribed medications, and doses of rotavirus and pneumococcal vaccines administered to the child and paid by the parents.
Households were classified into three categories by income level: (1) Monthly income less than 1000 euro; (2) monthly income between 1000 and 2000 euro, and (3) monthly income more than 2000 euro. They were also classified into three categories based on educational attainment: parents with no education or that only completed primary education, that completed secondary education, or with higher education degrees.
We performed the survey in four different paediatric clinics so that the three income groups under study would be sufficiently represented.
The statistical analysis of the data was performed by means of the commercial application SPSS® 15.0. We expressed the main data as means and standard deviations in the case of quantitative variables and as absolute frequencies and percentages in the case of qualitative variables. We calculated the 95% confidence intervals (CIs).
We used the Mann–Whitney U test to compare quantitative variables after finding that they did not fit a normal distribution (Kolmogorov–Smirnov test). The chi squared test was used to compare qualitative variables. Statistical significance was defined as p<.05.
We performed a multivariate logistic regression analysis starting with the maximum border and removing variables one at a time until only those that were statistically significant remained.
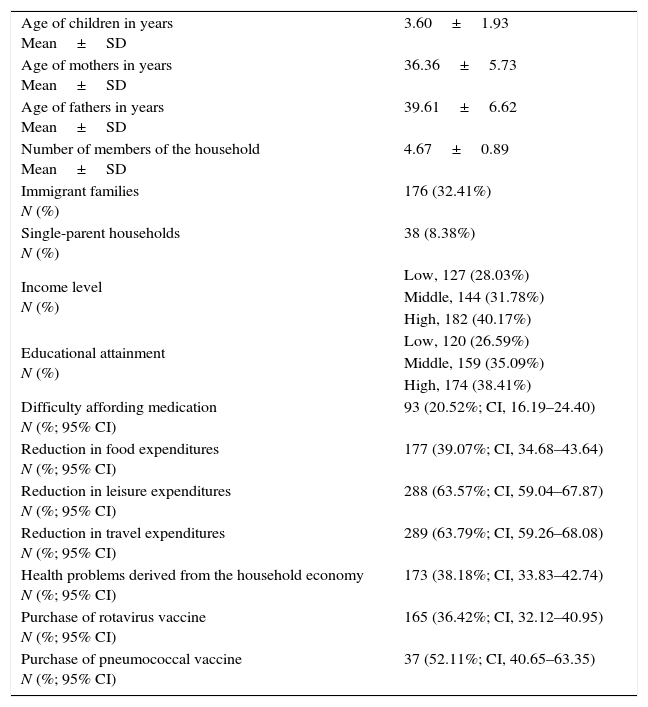
ResultsWe collected data for 453 children, of whom 217 (47.90%) were male and the rest female, with a mean age of 3.60 years (range, 1–7 years; SD, 1.93). The mean maternal age was 36.36 years (SD, 5.73) and the mean paternal age 39.61 years (SD, 6.62). The mean number of household members was 4.67 (range, 2–7; SD, 0.89).
In 176 families (32.41%) one of the parents was an immigrant. Thirty-eight households (8.38%) were of single parents, with the mother as the head in all cases.
Both parents were unemployed in 21 households (4.63%).
Regarding income, we found 127 households (28.03%) in the low-income bracket, 144 households (31.78%) in the medium-income bracket, and 182 households (40.17%) in the high-income bracket.
The high-income households were concentrated in one of the three health care centres where we conducted the study, the low-income households in another centre, and the middle-income households in the last of the three centres.
Purchasing prescribed medication was financially difficult for the families of 93 children (20.52%; 95% CI, 16.98–24.40).
With regard to parental educational attainment, 120 of those surveyed (26.59%) had completed basic studies, 159 (35.09%) secondary education, and 174 (38.41%) higher education degrees.
Of all households, 177 reported having reduced expenditures in food (39.07%; 95% CI, 34.68–43.64), 288 in leisure (63.57%; 95% CI, 59.04–67.87) and 289 in vacations and travel (63.79%; 95% CI, 59.26–68.08).
Parents reported having developed health problems due to their employment and economic circumstances in 173 cases (38.18%; 95% CI, 33.83–42.74).
When it came to vaccines that are not publicly funded, 165 children (36.42%; 95% CI, 32.12–40.95) were vaccinated against rotavirus, while 37 of the 71 children born after the funding for the pneumococcal vaccine had been discontinued had been vaccinated against pneumococcus (52.11%; 95% CI, 40.65–63.35).
Table 1 presents the epidemiological characteristics of the sample.
Epidemiological characteristics of the sample.
| Age of children in years Mean±SD | 3.60±1.93 |
| Age of mothers in years Mean±SD | 36.36±5.73 |
| Age of fathers in years Mean±SD | 39.61±6.62 |
| Number of members of the household Mean±SD | 4.67±0.89 |
| Immigrant families N (%) | 176 (32.41%) |
| Single-parent households N (%) | 38 (8.38%) |
| Income level N (%) | Low, 127 (28.03%) |
| Middle, 144 (31.78%) | |
| High, 182 (40.17%) | |
| Educational attainment N (%) | Low, 120 (26.59%) |
| Middle, 159 (35.09%) | |
| High, 174 (38.41%) | |
| Difficulty affording medication N (%; 95% CI) | 93 (20.52%; CI, 16.19–24.40) |
| Reduction in food expenditures N (%; 95% CI) | 177 (39.07%; CI, 34.68–43.64) |
| Reduction in leisure expenditures N (%; 95% CI) | 288 (63.57%; CI, 59.04–67.87) |
| Reduction in travel expenditures N (%; 95% CI) | 289 (63.79%; CI, 59.26–68.08) |
| Health problems derived from the household economy N (%; 95% CI) | 173 (38.18%; CI, 33.83–42.74) |
| Purchase of rotavirus vaccine N (%; 95% CI) | 165 (36.42%; CI, 32.12–40.95) |
| Purchase of pneumococcal vaccine N (%; 95% CI) | 37 (52.11%; CI, 40.65–63.35) |
CI, confidence interval; SD, standard deviation.
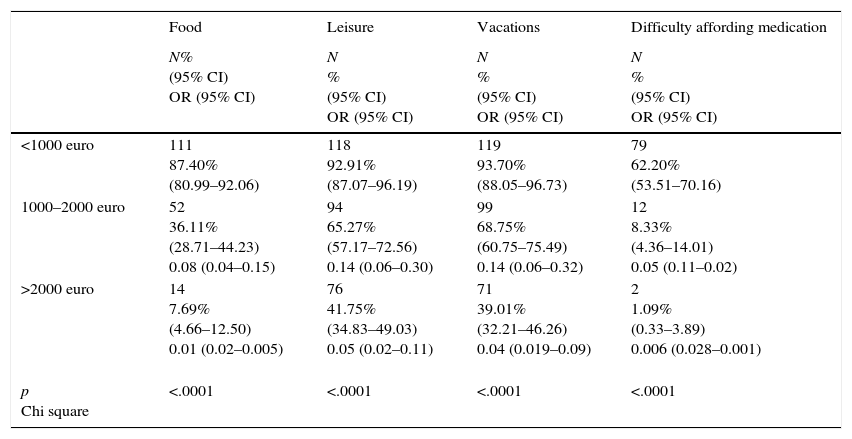
Table 2 presents the percentages of households in each of the three income groups under study that had reduced expenditures in food, leisure and vacations in the past year, showing that while reductions occurred in every group, the low-income group had been most affected. Table 2 also presents the data pertaining to the difficulty paying for medication, which was inversely correlated with income level.
Families that reduced their expenditures in the past year and had difficulty buying medicines by income level.
| Food | Leisure | Vacations | Difficulty affording medication | |
|---|---|---|---|---|
| N% (95% CI) OR (95% CI) | N % (95% CI) OR (95% CI) | N % (95% CI) OR (95% CI) | N % (95% CI) OR (95% CI) | |
| <1000 euro | 111 87.40% (80.99–92.06) | 118 92.91% (87.07–96.19) | 119 93.70% (88.05–96.73) | 79 62.20% (53.51–70.16) |
| 1000–2000 euro | 52 36.11% (28.71–44.23) 0.08 (0.04–0.15) | 94 65.27% (57.17–72.56) 0.14 (0.06–0.30) | 99 68.75% (60.75–75.49) 0.14 (0.06–0.32) | 12 8.33% (4.36–14.01) 0.05 (0.11–0.02) |
| >2000 euro | 14 7.69% (4.66–12.50) 0.01 (0.02–0.005) | 76 41.75% (34.83–49.03) 0.05 (0.02–0.11) | 71 39.01% (32.21–46.26) 0.04 (0.019–0.09) | 2 1.09% (0.33–3.89) 0.006 (0.028–0.001) |
| p Chi square | <.0001 | <.0001 | <.0001 | <.0001 |
The same was true of the percentage of individuals that reported health problems in the household since the start of the crisis: 70.07% (95%CI, 61.59–77.35) in the low-income group; 38.88% (95%CI, 31.30–47.05) in the middle-income group; and 15.38% (95%CI, 10.87–21.34) in the high-income group.
The presence of health problems since the start of the crisis was less frequent in individuals in the middle-income (1000–2000 euro; OR, 0.27; 95% CI, 0.45–0.16) and high-income brackets (>2000 euro; OR, 0.07; 95% CI, 0.13–0.04).
Likewise, individuals with a middle educational attainment (OR, 0.27; 95% CI, 0.14–0.52) and high educational attainment (OR, 0.033; 95% CI, 0.014–0.07) experienced less difficulty affording medications not funded by the public health care system.
The purchase of the rotavirus vaccine is directly correlated to middle and high income levels (OR, 1.13 and 3.84; 95% CI, 2–0.64 and 6.25–2.32, respectively) as well as middle and high educational attainment (OR, 1.92 and 9.97; 95% CI, 0.71–5.18 and 4.14–23.9, respectively).
We performed a multivariate analysis (binary logistic regression, see Table 3) of the variables that influenced non-purchase of prescribed medications (lower income and educational attainment), a reduction in food expenditures (lower income and number of members in the household), vaccination against rotavirus (higher income and educational attainment and non-immigrant status) and the presence of health problems in the family since the beginning of the crisis (unemployed status, lower educational attainment and lower income). In every instance, models were considered statistically significant if p<.0001. We validated the logistic regression models by means of the Hosmer–Lemeshow test and ROC curves.
Results of logistic regression analysis.
| Medication OR (95% CI) | Food OR (95% CI) | Rotavirus* OR (95% CI) | Health problems in parents OR (95% CI) | |
|---|---|---|---|---|
| Income | 0.118 (0.064–0.218) p<.0001 | 0.100 (0.067–0.149) p<.0001 | 2.170 (1.404–3.353) p<.0001 | 0.342 (0.235–0.500) p<.0001 |
| Educational attainment | 0.464 (0.291–0.741) p=.001 | No | 1.835 (1.137–2.963) p=.013 | 0.678 (0.467–0.936) p=.042 |
| Number of household members | No | 1.308 (1.01–1.754) p=.045 | NI | NI |
| Immigrants | No | No | 0.532 (0.295–0.961) p=.037 | NI |
| Unemployed | No | No | NI | 4.079 (1.129–14.735) p=.032 |
| R2/AUC | 0.528/0.878 | 0.530/0.691 | 0.277/0.751 | 0.328/0.689 |
| p | <.0001 | <.0001 | =.001 | <.0001 |
AUC, area under the curve; Food, decrease in food expenditures; Medication, difficulty affording medication; NI, variable not included in the final model; Rotavirus, vaccination against rotavirus.
Primary care is the foundation of the national health care system of Spain, and thus far it has been considered a model to follow due to its excellent outcomes.9,10 The policies undertaken to manage economic crises have an impact on the health of ordinary people.11 Countries such as Spain, Portugal and Greece have taken approaches based on budget cuts that have a negative impact on their health care systems and consequently on the well-being and quality of life of families.12
Primary care paediatric clinics provide a privileged vantage point to assess how individuals and families face the current crisis in Spain.13,14 As paediatricians caring for children and their families in PC clinics, we have the responsibility and the duty to promote social awareness of the rights of children and adolescents, so that they are acknowledged and protected.15
Certain collectives, such as children and immigrants, are particularly vulnerable during a crisis. Birth rates among immigrant populations are considerably higher than those in the native Spanish population, so this collective is well represented in our study, amounting to 32.41% of survey participants.
Children suffer the consequences of the economic crisis at home when their parents’ employment is affected: precarious employment, uncertainty and unemployment affect the physical and mental health of parents, leading to an increase in psychosocial disorders.16 The impoverishment of families due to precarious employment leads to difficulty affording a healthy diet or prescribed medications, especially if the latter are not funded by the public health care system, consistent with the findings of our study. There are still few studies on the impact of the economic crisis on individual health, and most of them have addressed the impact on mental health.17–19
The results of our study reflect the high unemployment rate in the population under study, which in many families affects both parents, with parents reporting health problems derived from their employment status and thus their economic situation. Broadly speaking, the immigrant population has a lower educational attainment, more members per household and higher rates of unemployment, and this economic precariousness entails difficulty affording prescribed medications and vaccinating children with vaccines that are not publicly funded, as well as reducing the budget for food.19 Most of the surveyed parents, including immigrants and native Spaniards, reported a reduction in their expenditures in leisure and travel.
At present and despite the crisis, immigrants continue to be a significant proportion of the Spanish population, and in fact the children of immigrants are part of the native Spanish paediatric population.20–24 The birth rate in the immigrant population far exceeds that of the native Spanish population,25 so this collective was well represented in our study. The current macroeconomic and job market situation are not the same as in the mid-eighties, when immigrants came attracted by the somewhat fictitious prosperity of Spain. Between 1995 and 2007, immigration was one of the main elements in the economic activity of Spain, whose model of development was based on labour-intensive sectors characterised by low productivity and little added value (construction, hospitality), and with immigrants coming from poor countries with weak health care systems who are most affected by discrimination, poor working conditions and unemployment while enduring xenophobic attitudes that have been exacerbated by the crisis in recent years.26–30 Nearly all immigrants in our study fit the pattern we have just described.
Along the lines of the reports of specialised foundations and institutions,31 we can conclude that the loss of income experienced by households is affecting the weakest and most vulnerable members of society, and that Spain is transitioning from a social model of “precarious integration” to a model of social welfare privatization32 in which the protective role of the state seems to be disappearing.33
There are limitations to our study, chief of which is the small sample size.
In the future, it would be advisable to conduct studies with larger samples and to reinforce that economic crises pose new challenges to society and the health authorities, chief among which is prioritising the protection of the health of the general population and of children in particular, as failing to protect children from poverty is one of the costliest mistakes a society can make.
FundingThis study did not receive any type of external funding.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Martín Martín R, Sánchez Bayle M, Gancedo García C, Teruel de Francisco MC, Coullaut López A. Las familias de la crisis en las consultas pediátricas de Atención Primaria: estudio descriptivo observacional. An Pediatr (Barc). 2016;84:189–194.