A study was performed in order to describe injuries associated with falls in children aged <1 year who attended the emergency department. The approaches used were examined, as well as the factors associated with the greater use of these approaches, and the management of the patient.
Patients and methodsThis was a multicentre, descriptive and analytical study that included all patients aged <1 year who had experienced a fall for which they attended the emergency departments of one of 8 Spanish Hospitals belonging to the “Unintentional Paediatric Injury Working Group” of the Spanish Paediatric Society. A record was made of the data regarding the visit, circumstances before arrival at the hospital, injuries observed, and the diagnostic and therapeutic approaches used.
ResultsA total of 1022 patients had experienced falls, that is, 0.35% of the emergencies attended in the study hospitals (95% CI, 0.348–0.352). The most commonly affected part was the head (58%). Cranial radiography was ordered in 31.8% of cases, and was associated with the presence of bruising or signs of fracture on examination (p<0.001), falls from heights >100cm (p<0.001), and age <3 months (p=0.004). Minor head injury was the most common finding (85.6%), followed by fractures, especially cranial fractures (7.1%), which were associated with bruising or signs of fracture on examination (p<0.001), and age <3 months (p<0.001). Six percent of the patients required admission to hospital. The risk factors for hospital admission in this group were falls from heights >50cm and age <3 months.
ConclusionsInjuries after falls in infants aged <1 year are commonly due to head trauma and frequently require additional diagnostic tests.
Describir y analizar las lesiones asociadas a caídas en los menores de un año, la actuación durante su atención en urgencias, los medios empleados en su manejo y los factores que condicionan un mayor uso de los mismos.
Material y métodosEstudio multicéntrico, descriptivo y analítico. Se incluyeron los menores de un año que habían acudido por caídas al servicio de urgencias de 8 hospitales integrantes del Grupo de Trabajo de Lesiones no Intencionadas de la Sociedad Española de Urgencias Pediátricas. Se recogieron datos sobre las circunstancias previas a la llegada a urgencias, las lesiones observadas, la actuación en urgencias y los medios empleados durante su manejo.
ResultadosSe identificaron 1.022 pacientes, un 0,35% de las urgencias atendidas (IC 95%: 0,348–0,352). La localización más frecuente del traumatismo fue craneal (58%). La indicación de radiografía de cráneo (31,8%) se relacionó con hematomas o signos de fractura en la exploración física (p<0,001), alturas mayores de 100cm (p<0,001) y edad menor de 3 meses (p=0,004). Tras el traumatismo craneal leve (85,6%), las fracturas fueron el diagnóstico más frecuente, fundamentalmente craneales (7,1%), asociándose con una edad menor de 3 meses (p<0,001) y con la existencia de haematoma o signos de fractura en la exploración física (p<0,001). Un 6% de los casos requirieron hospitalización, identificándose la edad menor a 3 meses y una caída mayor a 50cm como factores de riesgo.
ConclusionesLas lesiones por caídas en los menores de un año se producen fundamentalmente por traumatismos craneales y siguen constituyendo una indicación frecuente de realización de pruebas complementarias.
Of all unintentional injuries, falls constitute the most frequent reason for visiting paediatric emergency departments in the United States, generating more than 2 million visits in patients aged less than 19 years in 2013.1
The injuries sustained in falls are among the main causes of death and permanent brain damage secondary to unintentional injuries. The rate of mortality is highest in infants aged less than 1 year and adolescents,2 in who falls are associated with a large number of hospitalizations and a considerable economic and social burden.
Despite the current recommendations of major research groups3 that support watchful waiting in cases of mild fall-related injury, the performance of diagnostic tests in the initial assessment of these patients continues to be a widespread practice in many paediatric emergency departments.
The aim of our study was to describe and analyze fall-related injuries in infants aged less than 1 year, their management in emergency departments, the resources used in its management and the factors associated with an increased use of resources.
Materials and methodsWe conducted a substudy in the context of a larger study on the epidemiology and risk factors of fall-related injuries in infants aged less than 1 year.4
It was a descriptive multicentre study. We included infants aged less than 1 year that had sought care for a fall in the emergency departments of 8 hospitals members of the Working Group on Unintentional Injuries of the Sociedad Española de Urgencias Pediátricas (Spanish Society of Paediatric Emergency Medicine), between March 1, 2014 and February 28, 2015.
The study was approved by the ethics and clinical research committee of each participating hospital.
Fall is defined as the act or effect of falling until hitting ground or a firm surface that breaks the movement.5
We collected data in a form that was filled out with the families of patients during their stay in the emergency department. The data were entered in an electronic database (Google Drive) that could only be accessed by the principal investigator of the study.
We included epidemiological data (age, mechanism of the fall, height of fall and whether the fall had been witnessed), the circumstances of the arrival to the emergency department (reason for visit, mode of transport and time elapsed since fall) and the management in the emergency department (specialist that cared for patient, type and location of injuries, diagnostic tests, interventions performed, patient destination after discharge from department and final diagnosis).
The data were analyzed with the statistical software SPSS 18.0. We described quantitative variables as median and interquartile range (IQR), and qualitative variables as absolute and relative frequencies; we made inferential analyses of qualitative variables using the χ2 test, using the Bonferroni adjustment for multiple comparisons. In the latter case, we have presented the overall p-values in the tables, and specified in the text the p-values for each pair of categories for which the differences continued to be statistically significant after the correction. We used the Student t-test for the analysis of quantitative variables. We assessed for independent risk factors for the performance of diagnostic tests, the presence of a skull fracture and the need for hospital admission by means of logistic regression. We set the p-value for statistical significance at less than 0.05.
ResultsBefore arrival to the emergency departmentDuring the period under study, the participating hospitals received 289,887 emergency visits, and we identified 1022 patients aged less than 1 year that sought care for fall-related injuries, which amounted to an incidence of 0.35% (95% CI, 0.348–0.352%).
An evaluation in the emergency department was sought directly by parents in 924 patients (90.4%), whereas 63 patients (6.1%) were referred from primary care, 31 (3%) transferred from another hospital, and 4 (0.4%) arrived following a telephone consultation with the emergency department.
Most patients reached the emergency department in private vehicles (968; 94.7%), followed by non-urgent ambulances (36; 3.5%), urgent ambulances (14; 1.3%) and public transportation (4; 0.4%).
The median time elapsed to arrival to the emergency department was 60min (IQR, 60–180min). It is worth noting that the elapsed time was shorter in patients that had fallen from less than 1m (median, 60min) compared to those that fell from more than 1m (median, 90min), although the difference was not statistically significant (p=0.576). Less time also elapsed for falls that had been witnessed (median, 60min) compared to falls that were not witnessed (median, 90min), a difference that was also not significant (p=0.152).
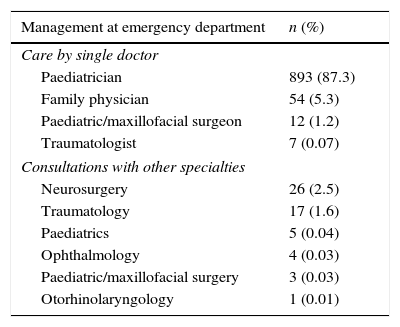
Data on emergency careNine hundred and sixty-six children (94.5%) received care from a specialist. Fifty-six cases (5.4%) required the collaborative assessment of several professionals, with the most frequent consultations involving specialists in neurosurgery (26; 2.5%) and traumatology (17; 1.6%) (Table 1).
Management at the emergency department.
| Management at emergency department | n (%) |
|---|---|
| Care by single doctor | |
| Paediatrician | 893 (87.3) |
| Family physician | 54 (5.3) |
| Paediatric/maxillofacial surgeon | 12 (1.2) |
| Traumatologist | 7 (0.07) |
| Consultations with other specialties | |
| Neurosurgery | 26 (2.5) |
| Traumatology | 17 (1.6) |
| Paediatrics | 5 (0.04) |
| Ophthalmology | 4 (0.03) |
| Paediatric/maxillofacial surgery | 3 (0.03) |
| Otorhinolaryngology | 1 (0.01) |
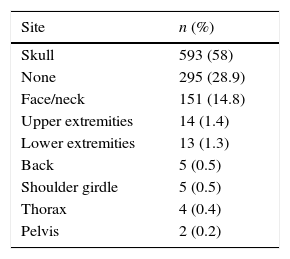
Traumatic injury was most frequently located in the head (593; 58%). The site of impact could not be determined in a considerable percentage of cases (295; 28.9%), and 59 patients (5.8%) experienced trauma in more than one site. Contusion and haematoma were the lesions detected most frequently (633; 61.9%), followed by signs of fracture (94; 9.1%). In 44 cases (4.3%) there was more than one type of injury, mostly the combination of haematoma and signs of fracture (23; 2.2%) (Table 2).
Site and type of injuries.
| Site | n (%) |
|---|---|
| Skull | 593 (58) |
| None | 295 (28.9) |
| Face/neck | 151 (14.8) |
| Upper extremities | 14 (1.4) |
| Lower extremities | 13 (1.3) |
| Back | 5 (0.5) |
| Shoulder girdle | 5 (0.5) |
| Thorax | 4 (0.4) |
| Pelvis | 2 (0.2) |
| Type of injury | N (%) |
|---|---|
| Contusion/haematoma | 633 (61.9) |
| None | 341 (33.4) |
| Open/closed fracture | 49 (4.8) |
| Abrasion/laceration | 20 (2) |
| Cut/puncture wound | 14 (1.4) |
| Avulsion | 6 (0.6) |
| Corneal erosion | 4 (0.4) |
| Localized oedema and tumefaction | 1 (0.1) |
Diagnostic tests were performed in 421 visits (39.2%).
Skull radiographs were the most frequently ordered diagnostic test, performed in as many as 31.8% of patients, followed by head computed tomography (CT) in 7.6%, long bone radiographs in 2.2% and transfontanellar ultrasound in 1.2%. Blood or urine tests were ordered in 17 patients (1.6%) and radiographs of the chest or abdomen in 15 (1.5%). Sixty-two patients (6%) underwent more than 1 diagnostic test, most frequently a skull radiograph and a head CT scan (in 38 patients).
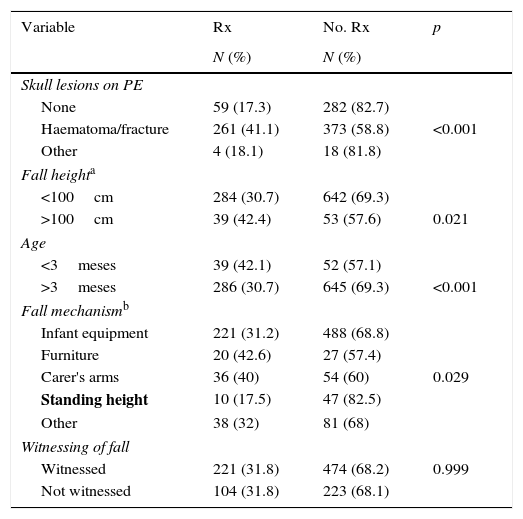
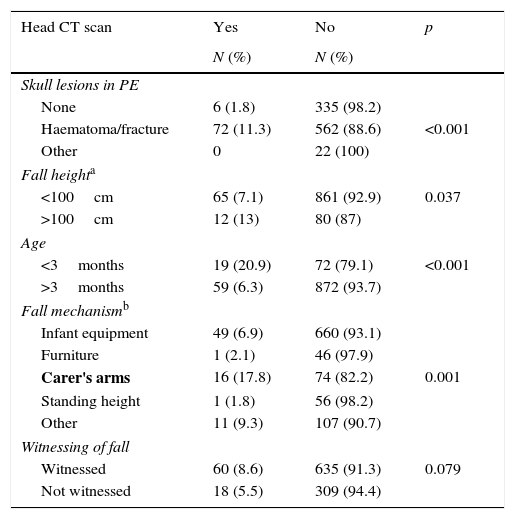
We analyzed the performance of diagnostic tests based on the detection of injuries during physical examination, the height of the fall, the mechanism of the fall and whether the fall was or was not witnessed by a caregiver (Tables 3 and 4).
Plain radiography (Rx) in head trauma caused by falls in infants aged less than 1 year (univariate analysis).
| Variable | Rx | No. Rx | p |
|---|---|---|---|
| N (%) | N (%) | ||
| Skull lesions on PE | |||
| None | 59 (17.3) | 282 (82.7) | |
| Haematoma/fracture | 261 (41.1) | 373 (58.8) | <0.001 |
| Other | 4 (18.1) | 18 (81.8) | |
| Fall heighta | |||
| <100cm | 284 (30.7) | 642 (69.3) | |
| >100cm | 39 (42.4) | 53 (57.6) | 0.021 |
| Age | |||
| <3meses | 39 (42.1) | 52 (57.1) | |
| >3meses | 286 (30.7) | 645 (69.3) | <0.001 |
| Fall mechanismb | |||
| Infant equipment | 221 (31.2) | 488 (68.8) | |
| Furniture | 20 (42.6) | 27 (57.4) | |
| Carer's arms | 36 (40) | 54 (60) | 0.029 |
| Standing height | 10 (17.5) | 47 (82.5) | |
| Other | 38 (32) | 81 (68) | |
| Witnessing of fall | |||
| Witnessed | 221 (31.8) | 474 (68.2) | 0.999 |
| Not witnessed | 104 (31.8) | 223 (68.1) | |
The table shows the overall p-value, while the text specifies the particular p-value for comparisons of 2 categories that were significant.
The category with a significantly lower frequency of skull radiograph ordering compared to other mechanisms is presented in boldface.
PE, physical examination.
Head computed tomography in fall cases in infants aged less than 1 year (univariate analysis).
| Head CT scan | Yes | No | p |
|---|---|---|---|
| N (%) | N (%) | ||
| Skull lesions in PE | |||
| None | 6 (1.8) | 335 (98.2) | |
| Haematoma/fracture | 72 (11.3) | 562 (88.6) | <0.001 |
| Other | 0 | 22 (100) | |
| Fall heighta | |||
| <100cm | 65 (7.1) | 861 (92.9) | 0.037 |
| >100cm | 12 (13) | 80 (87) | |
| Age | |||
| <3months | 19 (20.9) | 72 (79.1) | <0.001 |
| >3months | 59 (6.3) | 872 (93.7) | |
| Fall mechanismb | |||
| Infant equipment | 49 (6.9) | 660 (93.1) | |
| Furniture | 1 (2.1) | 46 (97.9) | |
| Carer's arms | 16 (17.8) | 74 (82.2) | 0.001 |
| Standing height | 1 (1.8) | 56 (98.2) | |
| Other | 11 (9.3) | 107 (90.7) | |
| Witnessing of fall | |||
| Witnessed | 60 (8.6) | 635 (91.3) | 0.079 |
| Not witnessed | 18 (5.5) | 309 (94.4) | |
The table shows the overall p-value, while the text specifies the particular p-value for comparisons of 2 categories that were significant.
The category with a significantly greater frequency of CT scan ordering compared to other mechanisms is presented in boldface.
PE: physical examination
When it came to the mechanisms of falls, we made an adjustment for multiple comparison using the Bonferroni method, and found that skull radiographs were ordered less frequently for falls from standing compared to falls from infant equipment (p=0.031), furniture (p=0.005), a carer's arms (p=0.004) and other mechanisms (p=0.045). Computed tomography scans were requested more frequently for falls from a carer's arms compared to falls from infant equipment (p<0.001), furniture (p=0.008) and standing (p=0.003).
The multivariate analysis identified the presence of haematoma or signs of bone fracture in physical examination (p<0.001), fall height (p<0.001) and age (p<0.004) as independent factors for performance of skull radiography, while the statistical significance of fall height disappeared in the multivariate model. When it came to performance of head CT, the only identified risk factors were the presence of haematoma or signs of bone fracture in the physical examination (p<0.001) and age less than 3 months (p<0.001).
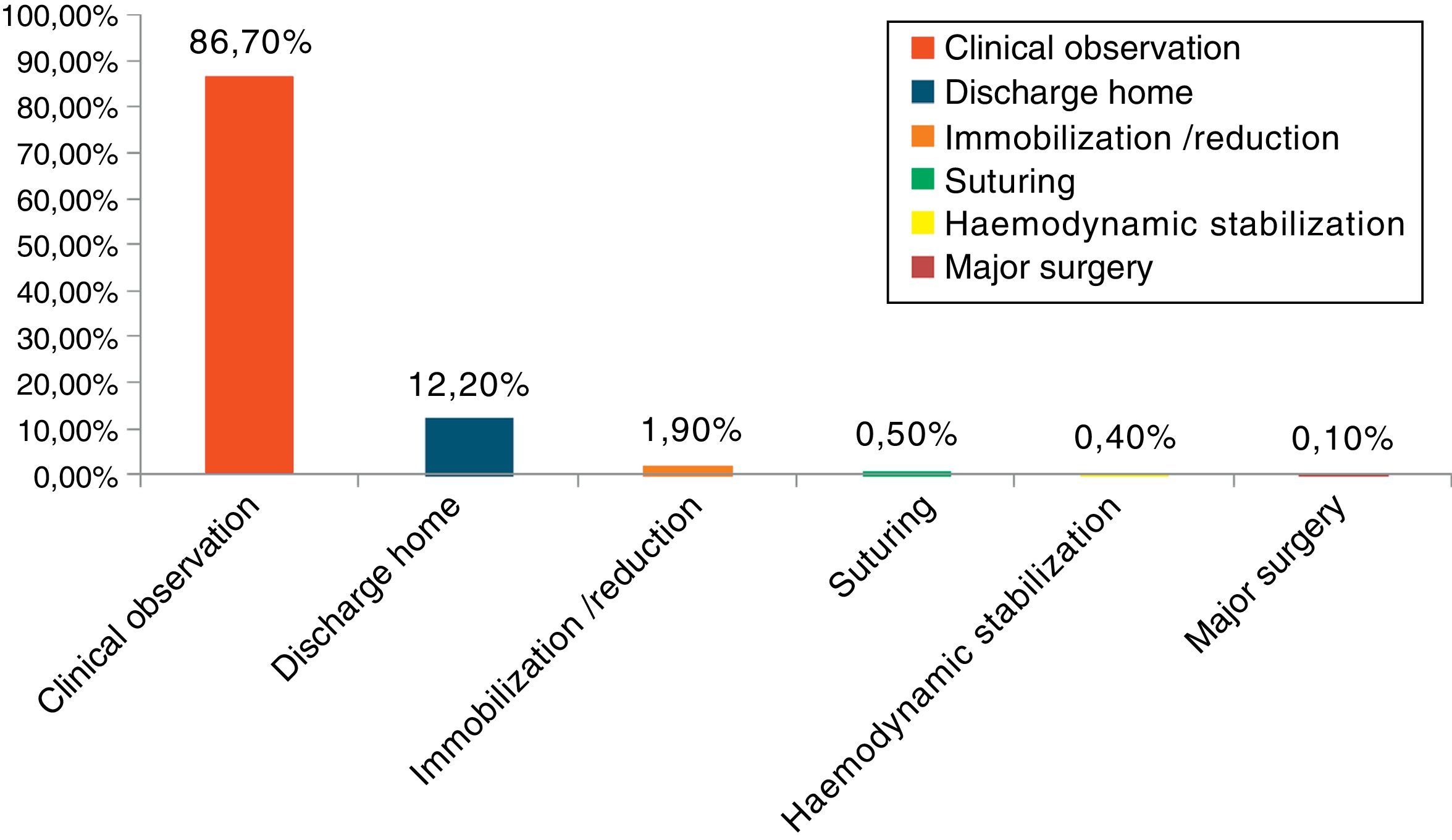
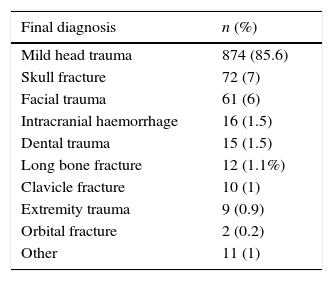
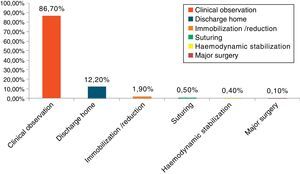
Most patients had to stay under observation, and 12.2% of them were discharged home directly from the emergency department (Fig. 1).
Although mild head trauma was the most frequent diagnosis (874; 85.6%), we ought to know that bone fracture was the second most frequent. The most frequent fractures were skull fractures (72; 7%), followed by long bone fractures (12; 1.1%) (Table 5). The independent risk factors for skull fracture identified in our study were the presence of haematoma or signs of fracture in the physical examination (p<0.001) and age less than 3 months (p<0.001), while fall height was not significant (p=0.075). Skull fractures were associated with falls from a carer's arms in the univariate analysis (p<0.001), but were not a significant factor and therefore removed in the logistic regression model.
Sixteen patients presented with intracranial haemorrhage (1.5%), of who half were younger than 3 months (8; 50%), and the risk of haemorrhage was significantly associated with age less than 3 months (p<0.001). The analysis of patients that underwent CT did not find an association between the presence of intracranial haemorrhage and fall height (p=0.31) or the mechanism of the fall (p=0.438). We ought to note that 13 of the 16 episodes of haemorrhage occurred in patients with temporal or parietal bone fractures.
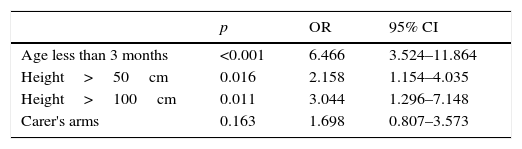
Hospital admission was required in 61 patients (6%), and we identified fall height of more than 50cm (p=0.001) and age less than 3 months (p<0.001) as risk factors for hospitalization. Hospital admission was also more frequent in patients that fell from a carer's arms compared to falls from infant equipment (p=0.004), although age less than 3 months and fall from a height of more than 50cm were the only independent risk factors identified in the logistic regression analysis (Table 6).
Twenty-four patients (39%) were hospitalised for more than 24h, and 8 required admission to an intensive care unit. None of the patients died in the first 24h following the fall.
DiscussionThe findings of this study allow us to analyze the emergency management of infants aged less than 1 year that seek care following a fall in paediatric emergency departments, and revealed a persisting tendency to perform skull radiographs and a moderate use of in-hospital resources in their management consisting of the performance of diagnostic tests, observation in emergency department, assessment by other specialists and admission to hospital.
In contrast, the use of out-of-hospital resources was scarce, as most patients sought care on the initiative of their parents and with their own resources, with referral from other health care settings amounting to only 9.5% and ambulance transport to 4.8% of the total. These findings were consistent with the results of a previous study conducted by the Sociedad de Urgencias Pediátricas, in which 96.3% of patients with mild head trauma reached the hospital through private means.6
One salient finding was the promptness with which caregivers sought an evaluation in the emergency department, with a median elapsed time since the fall of 1h, which has also been observed in previous studies.7 This may reflect an increased awareness of parents of the potential severity of fall-related injuries in this age group. Nevertheless, in our study we found that patients that fell from greater heights or whose falls were not witnessed, with mechanisms with a significant potential for injury, did not seek emergency care earlier. We did not find data in the literature regarding these factors.
Kendrick et al. also found no evidence that caregiver awareness of the potential for severe injury is associated with an increased use of preventive measures, and observed that parents of patients that had fallen from furniture were less likely to use safety gates and left infants on raised surfaces more frequently.8
Haney et al.9 also highlighted the absence of effective preventive measures, as 40% of children aged less than 2 years have experienced at least 1 previous fall from a height.
Paediatricians managed most patients, although other specialists were consulted to assess the child in 6.9% of cases, primarily in the area of neurosurgery (26; 2.5%). We did not find any previous studies documenting the need for evaluation by other specialists in children that had experienced a fall.
The proportion of patients that underwent skull radiography and head CT was similar to those reported by some studies,10–12 and slightly higher than that reported in others, especially when it came to skull radiographs.13 These tests were ordered more frequently in patients that presented with haematoma or signs of fracture in the physical examination, in those aged less than 3 months and, in the case of skull radiographs, in those who had fallen from heights of more than 1m. The univariate analysis also found an association with the mechanism of the fall, but this probably does not reflect an actual relationship – as demonstrated by the results of logistic regression – but rather the association of both age and fall height with fall mechanism. García et al. also found a more frequent use of skull radiographs in younger patients.6 We have not found works in the literature analysing the association of the use of diagnostic tests with fall height or fall mechanism.
In relation to this finding, we ought to note that international guidelines and various studies are increasingly questioning the need for skull radiographs in the initial evaluation of patients with head trauma. In spite of this, it continues to be frequently used in emergency departments for the purpose of ruling out skull fracture, which is significant risk factor for traumatic brain injury in infants. However, radiography has little predictive value in the detection of brain injuries compared to physical examination and clinical manifestations, and there is evidence that intracranial injury may be present in patients with normal radiographic findings.14 Even when radiography detects intracranial injury, only a small percentage of these patients requires neurosurgery.3
Although most of the fall-related injuries in our series were mild, we ought to note that fractures constituted the second most-frequent diagnosis, most of them skull fractures and in infants aged less than 3 months, with no association with the height of the fall. The incidence of skull fractures was similar to those reported in previous studies,6,11,13 although these works did not analyze the association between skull fracture and factors such as fall height, patient age or mechanism of injury.
Our study found a total of 16 patients with intracranial haemorrhage (1.5%), and brain injury in 22% of patients with skull fractures. The percentage of brain injury associated with skull trauma reported by other authors is slightly higher,3 which may be due to the fact that our study only included patients with fall-related injuries, excluding other mechanisms of injury such as motor vehicle accidents. The frequency of intracranial injury observed in our series was similar to the frequencies reported in studies with similar sample frames.11,15
Half of the patients presenting with intracranial haemorrhage were aged less than 3 years, and age was identified as a significant risk factor. Furthermore, 11 of the 16 cases of haemorrhage occurred in patients with parietal bone fractures, a type of skull fracture that was also significantly more frequent in this age group. However, there are other studies that have not found an increased risk of intracranial injury in children aged less than 2 years.6 One possible explanation is that the median age of the patients included in these other studies was greater, and that the authors did not carry out age-stratified analyses in children aged less than 2 years. We have not found any studies that included as many patients aged less than 3 months as ours.
In our series, 14 patients (1.3%) presented with clinically significant injuries (requiring neurosurgery, intubation of more than 24h, hospitalization of more than 48h, admission to the PICU or haemodynamic stabilization); none of them died. Kupperman et al.3 reported a prevalence of 0.9%, with an increased probability of clinically significant injury in the presence of certain prognostic variables. Similar percentages have been reported for Spain at the national level.6
On the other hand, only 12.2% of patients managed for falls were discharged without undergoing any intervention, while 86.7% required clinical observation and 2.9% some form of procedure (major surgery, suturing, immobilization/reduction or haemodynamic stabilization).
Furthermore, 6% (61) of the patients were hospitalised, of which 8 were admitted to an intensive care unit. There is variability in the percentages of hospitalization reported in the literature, with some studies reported rates similar to those in our study,11 and others reporting higher12 or lower13 rates, which may be due to differences in infrastructure and the availability of short-stay observation units. The rate of admission to the PICU was similar to those reported by other authors.6,13
The independent risk factors for hospital admission identified in our study were fall from height of more than 50cm and age less than 3 years. We did not find any studies in the reviewed literature analysing the association of these factors with the risk of hospitalization.
There are limitations to our study, for instance, that we did not consider the association between the clinical presentation and the ordering of diagnostic tests. However, the aim of our study was not to judge whether the use of diagnostic tests was appropriate, but to describe and analyze the actual characteristics and management of fall-related injuries in emergency departments in Spain. Other limitations include the variability that may stem from the different protocols at use in each hospital, the potential for missing data on patients that did not seek emergency care due to the seeming mildness of the manifestations, and the absence of a subsequent followup to analyze patient outcomes and detect events secondary to the fall that may have manifested at a later time.
Thus, we found evidence that while fall-related injuries in infants aged less than 1 year are not usually severe, they continue to be a frequent reason for the performance of diagnostic tests, especially in infants aged less than 3 years and falls from greater heights.
Infants are usually kept under observation in the emergency department, and a small proportion requires assessment by other specialists. Age less than 3 months and falls from heights of more than 50cm were independent risk factors for hospital admission, and management of such cases was associated with an increased use of in-hospital resources.
Infants aged less than 3 months constitute a high-risk group, with a significant incidence of secondary brain injury, so emphasis must be placed on the importance of appropriate preventive measures, striving to improve the knowledge of caregivers on potential fall mechanisms and the strategies that they can use to prevent them.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rubio García E, Jiménez de Domingo A, Marañon Pardillo R, Triviño Rodríguez M, Frontado Haiek LA, Gilabert Iriondo N, et al. Caídas en menores de un año: ¿qué hacemos en urgencias? An Pediatr (Barc). 2017;87:269–275.
Previous presentation: This study was presented as an oral communication at the XX Annual Meeting of the Sociedad Española de Urgencias de Pediatría, 2015, Bilbao, Spain.