Recent studies show that many preterm children without apparent neurological sequelae present some difficulties in different areas, such as coordination or balance during their school years. The Movement Assessment Battery for Children-2 (MABC-2) has demonstrated to be a useful tool to validate the coordination, while the stabilometric platform was the reference standard test for validating the balance.
Patients and methodCase–control study carried out on preterm children from 7 to 10 years old and healthy term infant controls of the same ages. The same age band of MABC-2 was applied and the static balance by the stabilometric platform was analysed.
ResultsA total of 89 subjects were included, 30 preterm children ≤1500g birthweight, 29 preterm children >1500g birthweight, and 30 controls. Preterm children obtained the lowest scores on an overall basis in hand dexterity and balance tests in MABC-2, regardless of their birthweight. Lower gestational age was associated with poorer outcomes in hand dexterity and total scores in MABC-2. Balance results were similar using the stabilometric platform, regardless of prematurity.
ConclusionsA little more than 10% preterm and term children could have coordination disorders or be at risk of developing them using the MABC-2. Despite the visual-motor coordination being similar, preterm children could face greater difficulties in hand dexterity while, in the absence of neurological comorbidity, preterm and term children balance could be comparable.
Estudios recientes demuestran que muchos niños prematuros sin secuelas neurológicas aparentes presentan dificultades en diferentes áreas, como la coordinación o el equilibrio, durante la etapa escolar. El Movement Assessment Battery for Children-2 (MABC-2) constituye una herramienta validada para la valoración de la coordinación, mientras que la estabilometría sería la prueba gold standard para el equilibrio.
Pacientes y métodoEstudio de casos y controles realizado en niños prematuros de 7-10 años y controles sanos nacidos a término de la misma edad. En ambos grupos se aplicó la franja de edad número 2 del MABC-2 y se analizó el equilibrio estático mediante estabilometría.
ResultadosSe incluyeron 89 sujetos: 30 prematuros de peso al nacimiento≤1.500g, 29 prematuros de peso>1.500g y 30 controles. Los prematuros obtuvieron peores puntuaciones totales de forma global en destreza manual y equilibrio en el MABC-2, independientemente del peso al nacimiento. La menor edad gestacional supuso la obtención de peores puntuaciones en destreza manual y scores totales en el MABC-2. El equilibrio fue similar mediante la estabilometría, independientemente de la prematuridad.
ConclusionesAlgo más de un 10% de prematuros y controles podría tener trastornos de la coordinación o estar en riesgo de desarrollarlos empleando el MABC-2. A pesar de que la coordinación visomotriz fue similar, los prematuros podrían tener mayores dificultades en destreza manual, mientras que en ausencia de comorbilidad neurológica, el equilibrio postural parece ser equiparable al de los controles sanos de su misma edad.
Advances in the fields of obstetrics and neonatology have improved the survival of children born preterm. However, this improvement is associated with considerable morbidity.1
Recent studies have shown that compared to their peers, many children born preterm considered to be free of neurological sequelae experience difficulties in some developmental areas that may go unnoticed until school age, such as coordination, balance, or attention.2,3
The acquisition of motor skills and control is a long process that starts with newborn reflexes and continues throughout the lifespan and is influenced by environmental factors and the performance of motor activities during development.4,5 Visual-motor integration is defined as the immediate and precise response that takes place following the appearance of an object in the visual field.6 Developing adequate coordination requires having an adequate body scheme combined with adequate afferent sensory information and control over the existing body scheme, which allow an effective motor response.
Postural control is defined as the ability to sustain balance by maintaining the body centre of gravity on the base of support.7 From a biomechanical perspective, we use the term “balance” to refer to the dynamics of body posture to prevent falls, which is related to the forces that act on the body.8 Maintaining balance requires the integration of the information provided by the proprioceptive, vestibular and visual systems.
There are different tools to assess motor competence and coordination, such as the Bayley-III scale or the Touwen Infant Neurological Examination for infants and toddlers, and the Bruininks-Oseretsky Test of Motor Proficiency, the Visual Motor Integration Test or the Movement Assessment Battery for Children-2 (MABC-2) for school-aged children, among others.
Recent studies have shown that the Bayley scale is one of the best tools for the assessment of infants and young children, while the MABC-2 and the Bruininks-Oseretsky Test of Motor Proficiency would be the preferred assessment tools in school-aged children.9 Stabilometry, also known as posturography, is currently the gold standard for the specific assessment of balance.10
We designed this study with the aim of analysing coordination and balance in school-aged children born preterm with no significant neurological sequelae, comparing them with healthy children born to term of the same age to assess the potential association of the degree of prematurity and these two motor skills.
Patients and methodsWe conducted a cross-sectional analytical case–control study in children aged 7–10 years born in our hospital between 2001 and 2004. We collected the data for the study in 2012. There were two groups of children under study:
- -
Experimental group of children born preterm (≤37 weeks’ gestation). This group was further subdivided based on birth weight into children with birth weights of 1500g or less and with birth weights greater than 1500g. Chronological age was corrected based on 40 weeks’ gestational age.
- -
Control group (friends of the children in the experimental group): healthy children born at term (≥37 weeks’ gestation) with adequate birth weights (≥2500g).
We obtained the neonatal and perinatal data of the children born preterm from the database of the neonatal unit, and the information on the control group from structured interviews with the families. We verified that participants in both groups had good clinical outcomes, excluding children with cerebral palsy, chromosomal disorders, muscular disorders, cognitive impairment or severe neurosensory deficits. The sex distribution was random.
The study was approved by the Ethics Committee of the research centre, and the confidentiality of participants was protected conforming to the Declaration of Helsinki of 2008. We obtained the informed consent of the family or legal guardians for all participants in the study.
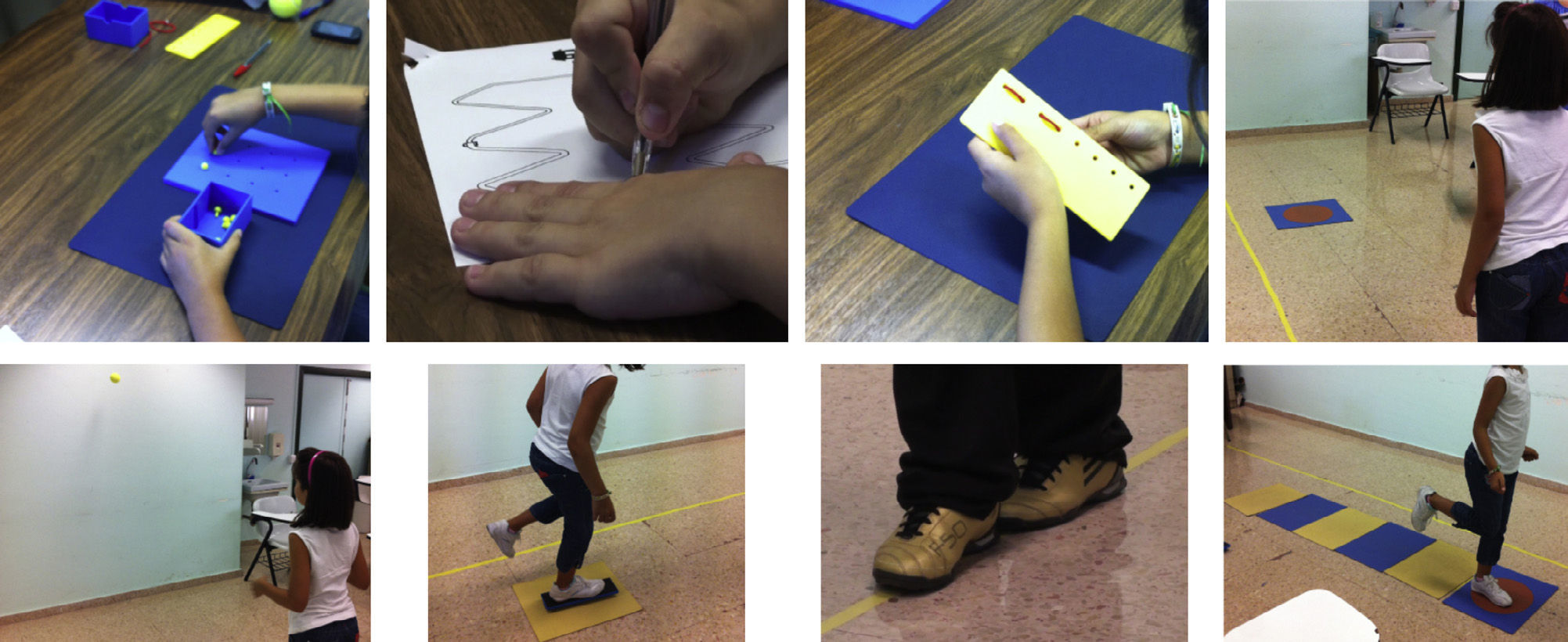
Movement Assessment Battery for Children-2We administered the battery of tests corresponding to age band 2 in the MABC-2, which comprehends ages 7 through 10 years.11 This battery assesses three motor skill categories: manual dexterity, aiming and catching, and balance through the performance of eight tasks: placing pegs in a board with holes, threading lace in the holes of a board, drawing a trail, ball throwing and catching, throwing a beanbag aiming at a target, balancing on one foot on a structure that is narrower at the bottom, heel-to-toe walking and hopping on one foot (Fig. 1). The scores obtained in each task are compared with the reference values for each age group to calculate a standard score that ranges between 1 and 19 and a corresponding percentile that is higher the higher the standard score. The sum of the score obtained in the three categories gives rise to a total test score (TTS). Total tests scores greater than 67 or percentiles greater than 15 are considered normal; TTSs ranging from 57 to 67, both included, or percentiles ranging from 6 to 15 indicate risk; and TTSs of 56 or less or percentiles of 5 or less are considered pathological. The interpretation of percentiles is equivalent for each of the three specific categories.
StabilometryPostural sway was measured using the Metitur Good Balance force platform and the software GB 300.1.3.20. The test was performed by having the child stand barefoot on the platform with arms lying straight at the sides of the body, with the palms of the hands resting against the outer thighs and the head facing forward in the direction of a mark on the wall placed at the child's eye level. We assessed static postural balance under eight conditions, combining feet together (ft) and feet apart (fa), eyes open (EO) and eyes closed (EC), with and without dampening of proprioceptive input through the addition of foam to the support surface (Fig. 2). Each task lasted 20s. We analysed the following variables: movement velocity (area drawn by the centre of pressure over a predetermined time span [mm2/s]) and length (in mm) of the smallest possible square containing 90% of the force points measured over 20s with a sampling frequency of 100Hz (side length/radius); therefore, lower scores in these variables corresponded to better results.
Statistical analysisWe used SPSS® version 18.0. We have expressed quantitative variables as mean and standard deviation, and qualitative variables as frequencies. We tested the goodness of fit of the different variables by means of the Kolmogorov–Smirnov test. To analyse quantitative variables, we used Student's t test for independent data if the variables followed a normal distribution, and otherwise the nonparametric Mann–Whitney U test. We compared variables between more than two groups by analysis of variance (ANOVA), with the post hoc Bonferroni correction whenever necessary. We compared qualitative variables by means of the chi square test. We set the level of statistical significance at P<.05.
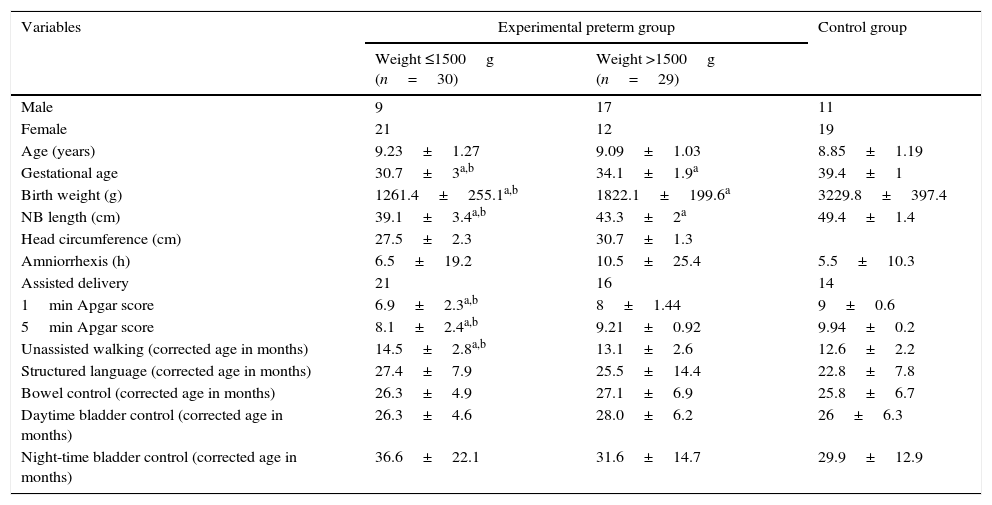
ResultsSample characteristicsDuring the four years under study, 546 children were born preterm in our hospital with birth weights of less than 2500g. The birth weight was 1500g or less in 81 (14.8%). We excluded 26 children from the latter group: twelve that died in the neonatal period, six that had cerebral palsy, two with intellectual disability and severe neurosensory deficits, four with severe malformations in other organs that impacted motor development, one with Steinert disease and one with Turner syndrome. Of the 55 children born preterm with weights of 1500g or less that appeared to develop normally, 30 agreed to participate. In order to have a homogeneous sample, we sought out 30 children born preterm with weights greater than 1500g free of neurologic sequelae. One participant did not show up on the day of the assessment, so this group ended up consisting of 29 children. The control group included 30 healthy children born to term with weights of 2500g or greater. We did not find statistically significant differences between the experimental preterm group and the control group in the age or sex distributions. All participants had a normal level of psychomotor development and neurologic examination. Table 1 shows the sample characteristics in terms of sex, perinatal and neonatal variables and timing of main milestones in psychomotor development.
Comparative analysis of sex, age, perinatal variables, neonatal anthropometric measurements and timing of psychomotor development milestones.
| Variables | Experimental preterm group | Control group | |
|---|---|---|---|
| Weight ≤1500g (n=30) | Weight >1500g (n=29) | ||
| Male | 9 | 17 | 11 |
| Female | 21 | 12 | 19 |
| Age (years) | 9.23±1.27 | 9.09±1.03 | 8.85±1.19 |
| Gestational age | 30.7±3a,b | 34.1±1.9a | 39.4±1 |
| Birth weight (g) | 1261.4±255.1a,b | 1822.1±199.6a | 3229.8±397.4 |
| NB length (cm) | 39.1±3.4a,b | 43.3±2a | 49.4±1.4 |
| Head circumference (cm) | 27.5±2.3 | 30.7±1.3 | |
| Amniorrhexis (h) | 6.5±19.2 | 10.5±25.4 | 5.5±10.3 |
| Assisted delivery | 21 | 16 | 14 |
| 1min Apgar score | 6.9±2.3a,b | 8±1.44 | 9±0.6 |
| 5min Apgar score | 8.1±2.4a,b | 9.21±0.92 | 9.94±0.2 |
| Unassisted walking (corrected age in months) | 14.5±2.8a,b | 13.1±2.6 | 12.6±2.2 |
| Structured language (corrected age in months) | 27.4±7.9 | 25.5±14.4 | 22.8±7.8 |
| Bowel control (corrected age in months) | 26.3±4.9 | 27.1±6.9 | 25.8±6.7 |
| Daytime bladder control (corrected age in months) | 26.3±4.6 | 28.0±6.2 | 26±6.3 |
| Night-time bladder control (corrected age in months) | 36.6±22.1 | 31.6±14.7 | 29.9±12.9 |
NB, newborn.
We found statistically significant differences between the three groups in gestational age, birth weight and birth length. We could not make comparisons of head circumference since we could not obtain this datum for most of the controls, as the families were unable to recall it. The Apgar scores were significantly lower in the group of children born preterm with weights of 1500g or less. When it came to psychomotor development, children born preterm with weights of 1500g or less started walking unassisted at a significantly later corrected age, albeit within normal limits.
Although we used birth weight as the criterion to determine the degree of prematurity, we also analysed the sample classifying children born preterm by weeks’ gestation (WG), and the resulting subgroups were comparable to those obtained based on birth weight (born at ≤32 WG and born at >32 WG). In the gestational age classification, 9 out of 30 children born at 32 WG or less had birth weights greater than 1500g, and 9 out of 30 children born at more than 32 WG had birth weights of 1500g or less, so the size of both groups did not change.
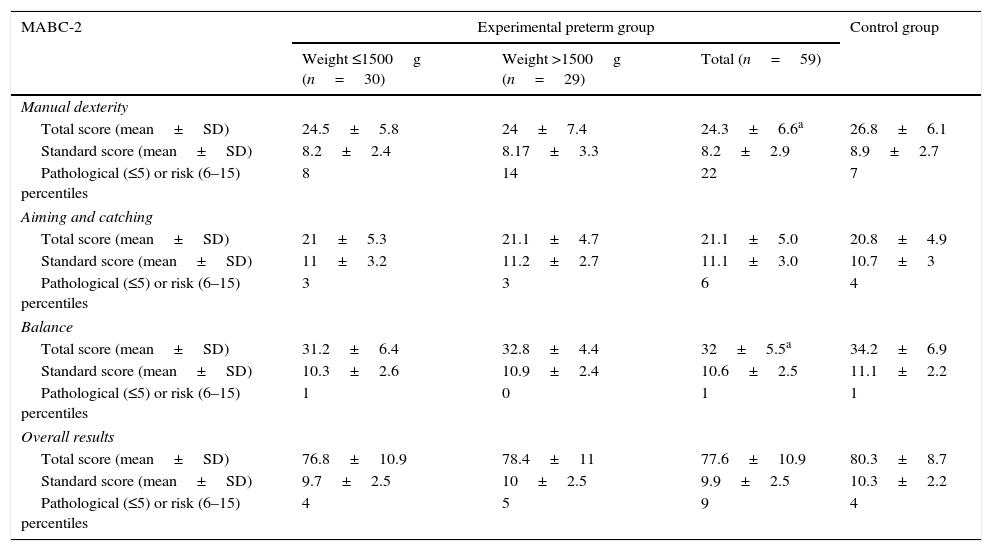
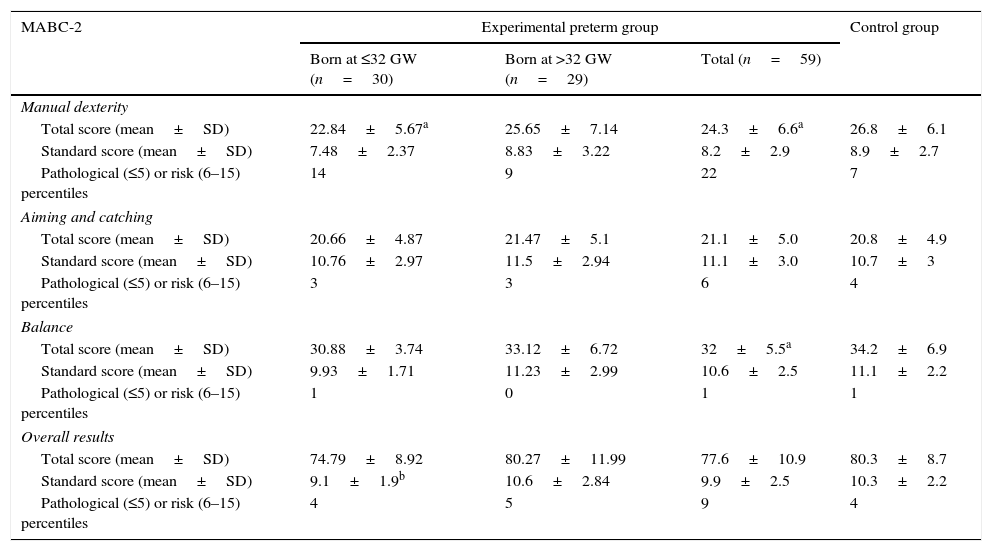
Movement Assessment Battery for Children-2Table 2 shows the total scores, standard scores and corresponding percentiles for the entire MABC-2 and for each of its specific subscales for each of the groups under study. The total scores in the manual dexterity and balance subscales were significantly lower in the experimental preterm group as a whole compared to the control group (P=.04). We did not find such differences in the aiming and catching subscale or in the total scores for the entire battery of tests. We also found no statistically significant differences between groups when we used birth weight as the criterion to establish the degree of prematurity; however, we did find significantly lower total scores in the manual dexterity subscale and the total standard score for the entire MABC-2 in the group of children born preterm at 32 WG or less compared to the control group (Table 3). The frequency of pathological total scores in the MABC-2 indicative of coordination and balance disorders (≤5th percentile) or of scores indicative of being at risk of developing such disorders (6th–15th percentiles) was similar in all three groups and independent of the degree of prematurity.
Comparative analysis of the results obtained by children in the different groups in the Movement Assessment Battery for Children-2 taking into account birth weight as the criterion used to classify the degree of prematurity.
| MABC-2 | Experimental preterm group | Control group | ||
|---|---|---|---|---|
| Weight ≤1500g (n=30) | Weight >1500g (n=29) | Total (n=59) | ||
| Manual dexterity | ||||
| Total score (mean±SD) | 24.5±5.8 | 24±7.4 | 24.3±6.6a | 26.8±6.1 |
| Standard score (mean±SD) | 8.2±2.4 | 8.17±3.3 | 8.2±2.9 | 8.9±2.7 |
| Pathological (≤5) or risk (6–15) percentiles | 8 | 14 | 22 | 7 |
| Aiming and catching | ||||
| Total score (mean±SD) | 21±5.3 | 21.1±4.7 | 21.1±5.0 | 20.8±4.9 |
| Standard score (mean±SD) | 11±3.2 | 11.2±2.7 | 11.1±3.0 | 10.7±3 |
| Pathological (≤5) or risk (6–15) percentiles | 3 | 3 | 6 | 4 |
| Balance | ||||
| Total score (mean±SD) | 31.2±6.4 | 32.8±4.4 | 32±5.5a | 34.2±6.9 |
| Standard score (mean±SD) | 10.3±2.6 | 10.9±2.4 | 10.6±2.5 | 11.1±2.2 |
| Pathological (≤5) or risk (6–15) percentiles | 1 | 0 | 1 | 1 |
| Overall results | ||||
| Total score (mean±SD) | 76.8±10.9 | 78.4±11 | 77.6±10.9 | 80.3±8.7 |
| Standard score (mean±SD) | 9.7±2.5 | 10±2.5 | 9.9±2.5 | 10.3±2.2 |
| Pathological (≤5) or risk (6–15) percentiles | 4 | 5 | 9 | 4 |
MABC-2, Movement Assessment Battery for Children-2; SD, standard deviation.
Comparative analysis of the results obtained by children in the different groups in the Movement Assessment Battery for Children-2 taking into account gestational age as the criterion used to classify the degree of prematurity.
| MABC-2 | Experimental preterm group | Control group | ||
|---|---|---|---|---|
| Born at ≤32 GW (n=30) | Born at >32 GW (n=29) | Total (n=59) | ||
| Manual dexterity | ||||
| Total score (mean±SD) | 22.84±5.67a | 25.65±7.14 | 24.3±6.6a | 26.8±6.1 |
| Standard score (mean±SD) | 7.48±2.37 | 8.83±3.22 | 8.2±2.9 | 8.9±2.7 |
| Pathological (≤5) or risk (6–15) percentiles | 14 | 9 | 22 | 7 |
| Aiming and catching | ||||
| Total score (mean±SD) | 20.66±4.87 | 21.47±5.1 | 21.1±5.0 | 20.8±4.9 |
| Standard score (mean±SD) | 10.76±2.97 | 11.5±2.94 | 11.1±3.0 | 10.7±3 |
| Pathological (≤5) or risk (6–15) percentiles | 3 | 3 | 6 | 4 |
| Balance | ||||
| Total score (mean±SD) | 30.88±3.74 | 33.12±6.72 | 32±5.5a | 34.2±6.9 |
| Standard score (mean±SD) | 9.93±1.71 | 11.23±2.99 | 10.6±2.5 | 11.1±2.2 |
| Pathological (≤5) or risk (6–15) percentiles | 1 | 0 | 1 | 1 |
| Overall results | ||||
| Total score (mean±SD) | 74.79±8.92 | 80.27±11.99 | 77.6±10.9 | 80.3±8.7 |
| Standard score (mean±SD) | 9.1±1.9b | 10.6±2.84 | 9.9±2.5 | 10.3±2.2 |
| Pathological (≤5) or risk (6–15) percentiles | 4 | 5 | 9 | 4 |
MABC-2, Movement Assessment Battery for Children-2; SD, standard deviation; WG, weeks’ gestation.
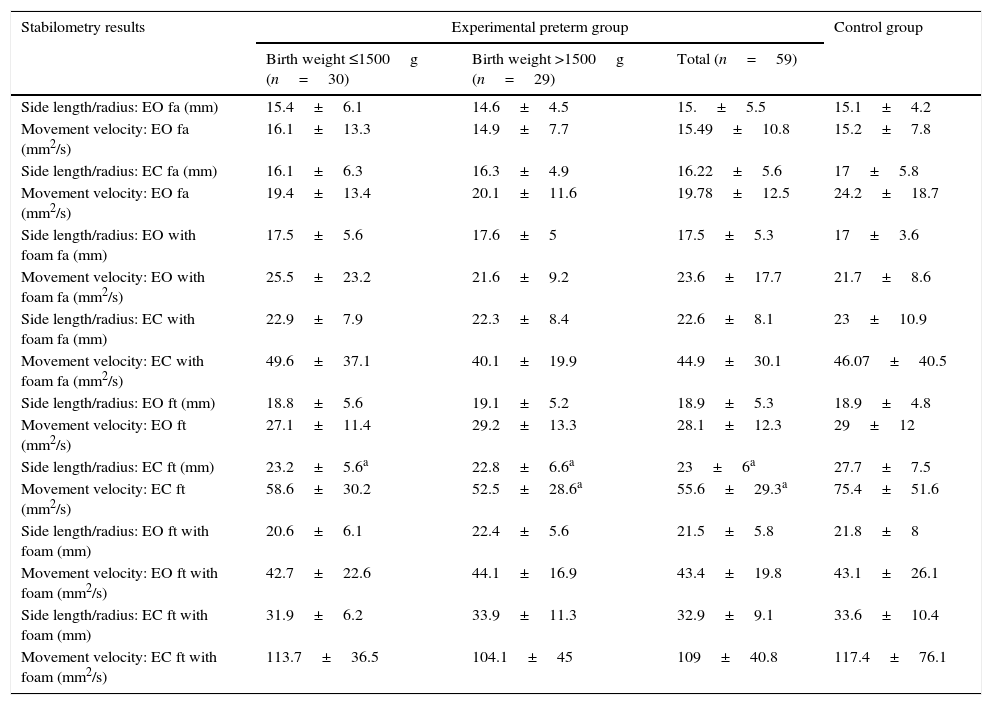
Table 4 shows the results obtained in the movement velocity and side length/radius variables for each of the eight conditions under study: EO+fa; EC+fa; EO+fa+foam; EC+fa+foam; EO+ft; EC+ft; EO+ft+foam; EC+ft+foam. The scores obtained with the eyes closed and feet together without foam were significantly better (lower) in the experimental group of children born preterm as a whole and also in children with lower birth weights compared to the control group. The scores obtained in both variables under the remaining conditions were similar, independent of the presence or absence of prematurity and of the degree of prematurity based on birth weight or gestational age.
Comparison between groups of stabilometry results.
| Stabilometry results | Experimental preterm group | Control group | ||
|---|---|---|---|---|
| Birth weight ≤1500g (n=30) | Birth weight >1500g (n=29) | Total (n=59) | ||
| Side length/radius: EO fa (mm) | 15.4±6.1 | 14.6±4.5 | 15.±5.5 | 15.1±4.2 |
| Movement velocity: EO fa (mm2/s) | 16.1±13.3 | 14.9±7.7 | 15.49±10.8 | 15.2±7.8 |
| Side length/radius: EC fa (mm) | 16.1±6.3 | 16.3±4.9 | 16.22±5.6 | 17±5.8 |
| Movement velocity: EO fa (mm2/s) | 19.4±13.4 | 20.1±11.6 | 19.78±12.5 | 24.2±18.7 |
| Side length/radius: EO with foam fa (mm) | 17.5±5.6 | 17.6±5 | 17.5±5.3 | 17±3.6 |
| Movement velocity: EO with foam fa (mm2/s) | 25.5±23.2 | 21.6±9.2 | 23.6±17.7 | 21.7±8.6 |
| Side length/radius: EC with foam fa (mm) | 22.9±7.9 | 22.3±8.4 | 22.6±8.1 | 23±10.9 |
| Movement velocity: EC with foam fa (mm2/s) | 49.6±37.1 | 40.1±19.9 | 44.9±30.1 | 46.07±40.5 |
| Side length/radius: EO ft (mm) | 18.8±5.6 | 19.1±5.2 | 18.9±5.3 | 18.9±4.8 |
| Movement velocity: EO ft (mm2/s) | 27.1±11.4 | 29.2±13.3 | 28.1±12.3 | 29±12 |
| Side length/radius: EC ft (mm) | 23.2±5.6a | 22.8±6.6a | 23±6a | 27.7±7.5 |
| Movement velocity: EC ft (mm2/s) | 58.6±30.2 | 52.5±28.6a | 55.6±29.3a | 75.4±51.6 |
| Side length/radius: EO ft with foam (mm) | 20.6±6.1 | 22.4±5.6 | 21.5±5.8 | 21.8±8 |
| Movement velocity: EO ft with foam (mm2/s) | 42.7±22.6 | 44.1±16.9 | 43.4±19.8 | 43.1±26.1 |
| Side length/radius: EC ft with foam (mm) | 31.9±6.2 | 33.9±11.3 | 32.9±9.1 | 33.6±10.4 |
| Movement velocity: EC ft with foam (mm2/s) | 113.7±36.5 | 104.1±45 | 109±40.8 | 117.4±76.1 |
EC, eyes closed; EO, eyes open; fa, feet apart; ft, feet together.
Data expressed as mean±standard deviation.
There is evidence that many of the children born preterm that we considered to be free of neurologic sequelae are at higher risk of developing coordination or balance disorders during school years.2,12–14 This type of disorders could impact numerous activities in the child that are important in developing autonomy, participating in sports, social skills and even academic performance.2,12,15
The MABC has proven to be an effective tool for the detection of coordination disorders in children born preterm. Its latest version, the MABC-2,11 has been validated recently for use in the Spanish paediatric population.16 Still, there is no data on its use on at-risk populations such as children born preterm.
In our study, the prevalence of coordinator disorders in the experimental group of children born preterm using percentiles of 15 or less in the MABC-2 as the cutoff was 15% (birth weight ≤1500g, 13%; birth weight >1500g, and 17%), compared to 13% in the control group; we did not find any differences between groups taking into account the degree of prematurity.
Studies similar to the one we have conducted have found prevalences of approximately 20%,2,15,17 however, a case series of 221 children born with weights of 1500g or less and/or at 32 WG or less18 found a prevalence of 15% at ages 7 and 8 years using the same cut-off point in the MABC, which is consistent with what we found in our series.
There is evidence that the prevalence of this type of disorders is inversely correlated with gestational age and birth weight, as studies conducted in children born preterm with birth weights of 1000g or less and/or at 28 WG or earlier have reported prevalences of about 30–40%3,19,20 and even higher.21
Leaving aside the limitations involved in having a small sample size, we did not find statistically significant differences in the total MABC-2 score within our sample using birth weight as the criterion for determining the degree of prematurity. However, when we categorised the degree of prematurity based on WG, children born at ≤32 WG or less had significantly lower standard scores compared to preterm children born at greater gestational ages.
Part of the variability in the prevalences reported in the literature may stem not only from the degree of prematurity, but also from the age at the time of assessment, the cut-off points used, or the version of the battery, as the scoring and interpretation schemes of the first and second version of the MABC are different and therefore may not be equivalent for the purpose of comparing studies that use different versions.20,22 On the other hand, some studies include children with neurologic sequelae such as cerebral palsy or neurosensory deficits, and this would alter the results to some extent,13,17,22–24 since were the children with neurologic disease excluded from the analysis the results could be comparable to those of the control group, as observed in our study.
Several authors have found that some variables, such as bronchopulmonary dysplasia or retinopathy and especially the presence of white matter lesions in the brain, can impact motor skills test results and the motor competence prognosis of children born preterm,23,25–27 while other variables, such as the early detection and treatment of neurologic sequelae by early intervention teams, could significantly improve motor competence. In our study, 40% of children born preterm with weights of 1500g or less and 10% of those born with weights ranging between 1501 and 2.499g had received this type of treatment, yet we were unable to find evidence of the influence of this variable based on the MABC-2 scores.
However, while some studies show a potential catch-up effect in motor skills scores in children born preterm with no medical comorbidities,19,28,29 others found that even in the absence of medical comorbidities, preterm children could experience greater difficulties performing tasks that require visual-motor integration, manual dexterity or balance,2,23,30 similar to what we found in our case series. Thus, there seems to be a multifactorial mechanism in the motor development of children born preterm.
When it came to the results for the different subscales of the MABC-2 in our study, 37% of children born preterm (birth weight ≤1500g, 27%; birth weight >1500g, 48%) scored in the 15th percentile or lower in the manual dexterity subscale compared to 23% of controls. The total scores in this subscale were significantly lower in the preterm group overall and also in the subgroup of preterm children born at 32 weeks’ gestational age or earlier compared to the control group, so these results suggest that prematurity overall and low gestational age in particular could be risk factors for future manual dexterity difficulties.
We did not find statistically significant differences in aiming and catching, while the total scores in the balance subscale of the MABC-2 were significantly lower in the experimental group of children born preterm and independent of the degree of prematurity. These results are consistent with the literature. Brown et al.20 observed that children with birth weights of 1000g or less had greater difficulties with balance, followed by manual dexterity and last of all aiming and catching using the MABC-2, which was similar to the findings of Zwicker et al25 using the first version of the MABC.
Several studies have shown that children born preterm, including those free of neurologic sequelae, have poorer balance based on some of the tests included in batteries such as the MABC-2 or the Bruininks-Oseretsky Test of Motor Proficiency.2,20,25,27 However, we did not find statistically significant differences between groups using stabilometry, which is considered the gold standard for the assessment of balance10; in fact, in our series, children born preterm occasionally performed better under some of the conditions under study. The observed discrepancies between the two balance assessment tools (MABC-2 and stabilometry) stem from the type of movement that is analysed, as stabilometry specifically assesses postural control and the adaptive response to various controlled changes in sensory input, whereas the MABC-2 includes less specific exercises that involve not only posture control, but other variables such as agility.
Very few studies have used stabilometry in the assessment of children born preterm.26,27,31–33 Kluenter et al.32 assessed balance by means of the Balance Master® platform (NeuroCom; Clackamas, Oregon, USA) in 44 children aged 7 years that had been born preterm with birth weights of 1500g or less and two control groups: healthy children born at term (n=21) and 19 adults; while Lorefice et al.33 used the Wii Balance Master with the LabVIEW software (National Instruments; Austin, Texas, USA) in children born before 30 weeks’ gestation without neurological sequelae at ages 4–5 years (n=90), comparing them with a control group of children born to term (n=36). Both studies had results similar to ours that were not affected by the degree of prematurity.
ConclusionsIn the group of children born preterm in our series, despite them being considered free of neurologic sequelae, 15% may have coordination problems or be at risk of developing them based on the assessment with the MABC-2; and even in the group of children that were born at term, approximately 10% may have this type of disorders. Although visual-motor integration was similar in both groups, children born preterm, especially those with higher degrees of prematurity, may experience greater difficulty in the development of fine motor skills, while in the absence of neurologic comorbidities, the balance at ages 7–10 years in children born preterm was comparable to that of healthy children born to term when assessed by means of stabilometry.
FundingThis study is part of a project that has been awarded one of the XIV grants for clinical and epidemiological research of the Fundación Ernesto Sánchez Villares in year 2011.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rodríguez Fernández C, Mata Zubillaga D, Rodríguez Fernández LM, Regueras Santos L, Reguera García MM, de Paz Fernández JA, et al. Valoración de la coordinación y el equilibrio en niños prematuros. An Pediatr (Barc). 2016;85:86–94.