The use of central catheters (CC) is associated with mechanical complications (MC).
ObjectiveOur objective was to determine the relationship between CC positions and associated MC in neonates.
MaterialA descriptive analytical study was performed over a six year period in the NICU of the University Hospital Santa Lucía de Cartagena. Details were collected on the CC used, indication, reason for withdrawal, position in the imaging, MC, and treatment arising from them, as well as epidemiological data.
ResultsOf the total of 604 CC studied, the majority (347) were via the umbilical vein, followed by epicutaneous (193), and femoral vein (34). There were MC in 14.2% of catheters. Incorrect position of the tip was associated with greater MC (21.1 vs 8.2%; P<.001), including withdrawal due to MC (8.4 vs 3.1%; P<.01), extravasation (4.9 vs 1.9%; P<.05), pleural and pericardial effusions (1.4 vs 0.0%; P<.05), liver haematomas (4.6 vs 0.6%; P<.01), and ascites (2.8 vs 0.0%; P<.01). The midclavicular epicutaneous position of the tip was associated with greater MC (18.5 vs 6.8%; P<.05) than the brachiocephalic (0 vs 6.8%; NS). The low and ductal position of the umbilical vein catheter was also associated with higher rates of MC (24.5 vs 6%; P<.001 and 27 vs 6%; P<.001) due to the position of the tip. The most common complication was accidentally dislodged catheter.
ConclusionsThe incorrect location of the tip was associated with more MC. The midclavicular epicutaneous had more risk than centrally or brachiocephalic locations. The low and ductal positions of the umbilical vein catheter were associated with higher rates of MC.
El uso de catéteres centrales (CC) está asociado a complicaciones mecánicas (CM). Nuestro objetivo fue conocer si la posición incorrecta de la punta se asociaba con mayor incidencia de CM.
MaterialEstudio descriptivo de 6 años en la UCIN del Hospital Universitario Santa Lucía de Cartagena. Se recogieron los CC, la indicación, el motivo de retirada, la posición en las pruebas de imagen, las CM y el tratamiento derivado.
ResultadosSe estudiaron 604 CC, la mayoría (347) de vena umbilical, epicutáneos (193) y de vena femoral (34). El 14,2% tuvo CM. La posición incorrecta de la punta se asoció a mayores CM (21,1 vs. 8,2%; p<0,001), retirada por problemas mecánicos (8,4 vs. 3,1%; p<0,01), extravasación (4,9 vs. 1,9%; p<0,05), derrames pleurales y pericárdicos (1,4 vs. 0,0%; p<0,05), hematomas hepáticos (4,6 vs. 0,6%; p<0,01) y ascitis (2,8 vs. 0,0%; p<0,01). Los epicutáneos medioclaviculares se asociaron a mayores CM (18,5 vs. 6,8%; p<0,05) que los localizados en posición braquiocefálica (0 vs. 6,8%; NS) respecto a las localizaciones correctas. La posición baja o en ductus del catéter venoso umbilical se asoció a mayores CM respecto a la posición correcta (24,5 vs. 6%; p<0,001. y 27 vs. 6%; p<0,001). La complicación más frecuente fue la salida accidental.
ConclusionesLas localizaciones incorrectas de la punta de los CC se asociaron a más CM. Los epicutáneos medioclaviculares tuvieron más riesgo que los localizados en cavas o braquiocefálicos. La posición baja o en ductus del catéter venoso umbilical se asoció a mayores CM.
The use of central catheters (CCs) in neonatal units is widespread, and is one of the most frequently used invasive procedures. From the moment umbilical venous catheterisation (UVC) was first described in the late 1940s,1 this technique has allowed the management of children with more complex pathologies. The description of peripherally inserted central catheters (PICCs) by Shaw in 19732 was another milestone, allowing the management of infants with progressively lower weights and gestational ages that require longer hospitalisations and in many cases several central lines during their stay.
They can be used for a wide variety of purposes, such as the delivery of drugs, fluids, parenteral nutrition or medications with irritant properties or high osmolarities. In other cases, they prevent multiple painful stimuli associated to the repetition of venipuncture or invasive measurements, for instance of central venous pressure or arterial pressure.
The use of CCs is associated with various complications, such as accidental dislodgment, occlusion, phlebitis, thrombosis, infection or extravasation and others that are less frequent, such as pleural and pericardial effusion, ascites and even death.3
There are no validated international consensus guidelines on the use of different types of catheters, and different units have their own management guidelines, which show considerable variability.
Although the association between infection and CC use has been investigated extensively, fewer studies have analysed mechanical complications (MCs), their impact and their risk factors. Most of these studies consist in the enumeration of individual cases, which are very frequent, to the point that Garden and Laussen4 referred to the use of CCs as “an unending supply of unusual complications.”
There is evidence that malposition of the catheter tip is associated with increased morbidity.5 It is recommended that the catheter tip be placed in a central position. This placement, which should be the norm, is not always achieved, leading to the management of children with catheters that are by definition not placed in the midline.
The primary objective of our study was to determine whether different final positions, whether correct or incorrect, are associated with different rates of MCs. The secondary objective was to analyse the epidemiology of the use of CCs in our unit.
MethodsWe conducted an analytical and descriptive study of the newborns admitted between March 1, 2009 and February 28, 2015 to the neonatal intensive care unit of the Hospital Universitario Santa Lucía in Cartagena, Spain. The study had a retrospective design, with prospective collection of data starting on December 1, 2014. We did not include data on catheters already placed in patients who were transferred to our hospital (but included any catheters subsequently placed on them).
The catheters were of three different brands that were used indistinctly (Vygon, Plastimed, Arrow), with a single or double lumen, all of them made of polyurethane. The preferential method for verifying the final position of the tip was plain radiography. Repositioning manoeuvres of up to 1cm could be performed without the need to repeat the imaging test. We collected data from the hospital electronic health record database (SELENE) and the internal database (Neosoft). We designed a data collection spreadsheet and reviewed the medical records of all the patients, including imaging tests, admission and discharge summaries, data from autopsies when applicable, clinical outcomes and data on catheter insertion and maintenance. We actively searched for keywords such as complication, removal, catheter, line, thrombosis, haematoma, extravasation, ascites and effusion. Whenever we found an episode suggestive of a catheter-related complication, we sought information on it.
Classification of catheter positionPlacement was always assessed by a minimum of two researchers that were blinded to the final result. We considered UVCs in the inferior vena cava (IVC) or the junction of the IVC and the right atrium, and femoral catheters in the IVC to be placed correctly. We considered PICCs in high positions to be correctly placed if they were in the midline approaching the heart from above with the tip in the superior vena cava (SVC) at least 1cm away from the outline of the heart in preterm infants, and up to 2cm in full-term infants.6 Peripherally inserted central catheters in low positions were placed correctly if they were in the midline aiming at the heart from below, and considered iliac if the tip was positioned in a lower quadrant without reaching the midline; correctly placed jugular CCs were those that reached the midline through the SVC or with the tip positioned up to 1cm away from the outline of the heart in preterm infants or 2cm in infants born to term. We considered umbilical artery catheters (UACs) in high and low positions (D8-10 and L3-L5, respectively) to be correctly placed. Their placement was considered incorrect when the catheter was not in any of the aforementioned positions and there were no attempts to reposition it or a change in position at least 1cm away from the original site was not verified. The PICC was considered brachiocephalic if the tip of the catheter went past the midclavicular line but did not reach the correct position, and midclavicular if the tip was positioned between the lateral border and the midline of the clavicle.
In patients with hydrops fetalis, we excluded ascites and pericardial or pleural effusions from the analysis of complications.
We counted catheter days including the day of insertion as day 1. In cases in which the patient was transferred or died, that date was considered the last catheter day.
We performed the statistical analysis with SPSS 20 (IBM). We have described qualitative variables as proportions and quantitative variables and medians and interquartile ranges. We compared qualitative variables by means of the chi-square or the Fisher's exact test. We analysed qualitative variables by means of Student's t test or the Mann–Whitney U test, as appropriate. We used bivariate logistic regression analysis to calculate the odds ratio of different factors associated with MCs for each type of catheter. The independent variables under analysis, which have been studied in the literature,3,5 were gestational age and weight at the time of insertion, sex, number of lumina, and use of high-osmolarity parenteral nutrition. A two-tailed P<.05 was considered statistically significant. The study was approved by the Hospital Ethics Committee.
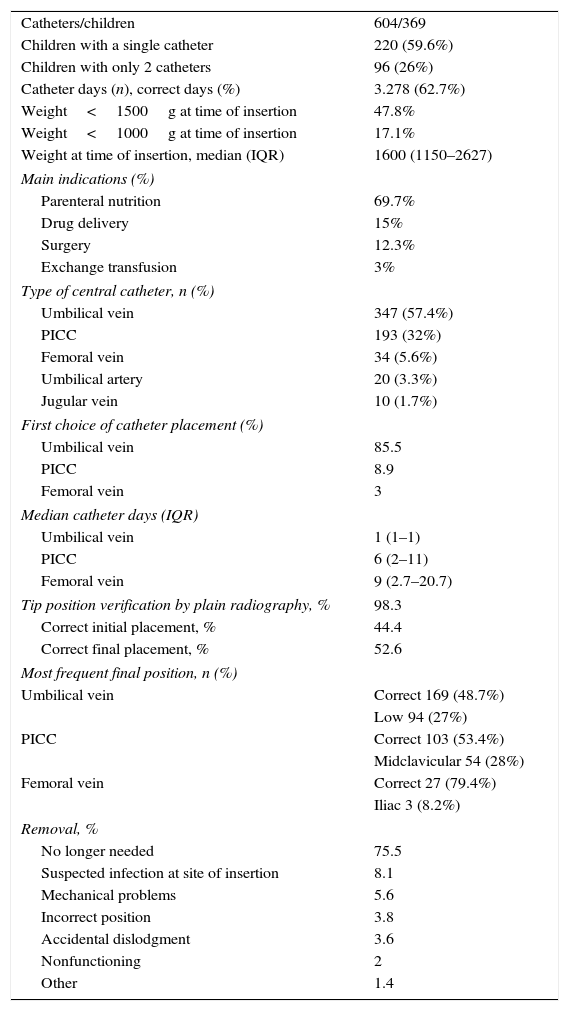
ResultsWe collected data on 628 CCs, of which 604 were finally included in the study. The reasons for excluding the other catheters were lack of data in four, and being already in place when the patient was transferred from another hospital and therefore not meeting the criteria for analysis in twenty. Table 1 summarises the epidemiology of CC use.
General data on the use of central catheters.
| Catheters/children | 604/369 |
| Children with a single catheter | 220 (59.6%) |
| Children with only 2 catheters | 96 (26%) |
| Catheter days (n), correct days (%) | 3.278 (62.7%) |
| Weight<1500g at time of insertion | 47.8% |
| Weight<1000g at time of insertion | 17.1% |
| Weight at time of insertion, median (IQR) | 1600 (1150–2627) |
| Main indications (%) | |
| Parenteral nutrition | 69.7% |
| Drug delivery | 15% |
| Surgery | 12.3% |
| Exchange transfusion | 3% |
| Type of central catheter, n (%) | |
| Umbilical vein | 347 (57.4%) |
| PICC | 193 (32%) |
| Femoral vein | 34 (5.6%) |
| Umbilical artery | 20 (3.3%) |
| Jugular vein | 10 (1.7%) |
| First choice of catheter placement (%) | |
| Umbilical vein | 85.5 |
| PICC | 8.9 |
| Femoral vein | 3 |
| Median catheter days (IQR) | |
| Umbilical vein | 1 (1–1) |
| PICC | 6 (2–11) |
| Femoral vein | 9 (2.7–20.7) |
| Tip position verification by plain radiography, % | 98.3 |
| Correct initial placement, % | 44.4 |
| Correct final placement, % | 52.6 |
| Most frequent final position, n (%) | |
| Umbilical vein | Correct 169 (48.7%) |
| Low 94 (27%) | |
| PICC | Correct 103 (53.4%) |
| Midclavicular 54 (28%) | |
| Femoral vein | Correct 27 (79.4%) |
| Iliac 3 (8.2%) | |
| Removal, % | |
| No longer needed | 75.5 |
| Suspected infection at site of insertion | 8.1 |
| Mechanical problems | 5.6 |
| Incorrect position | 3.8 |
| Accidental dislodgment | 3.6 |
| Nonfunctioning | 2 |
| Other | 1.4 |
IQR, interquartile range; PICC, peripherally inserted central catheter.
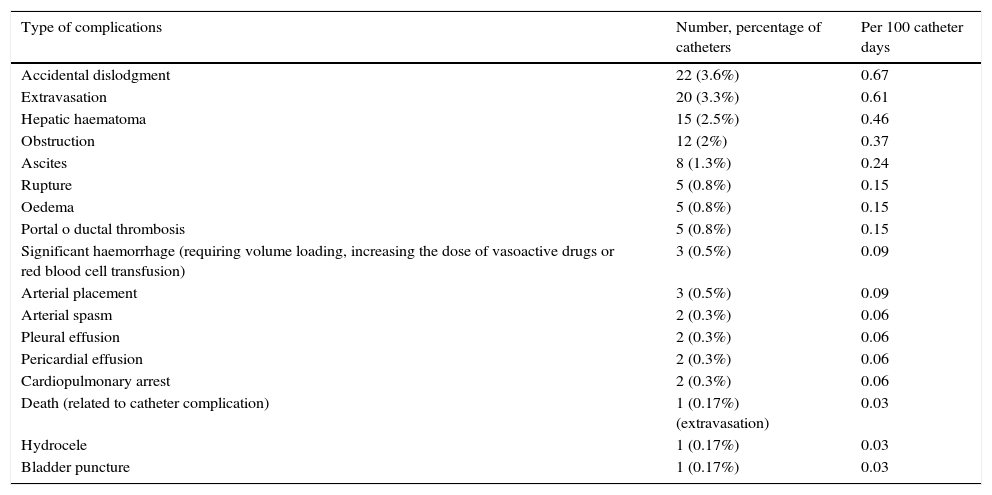
There were MCs in 86 catheters (14.2%) placed in 74 newborns. Nine newborns had complications from more than one catheter.
The most frequent complication was accidental dislodgment, followed by local extravasation. There were eight cases of ascites, two of pleural effusion, two of pericardial effusion and one death secondary to the extravasation of a PICC in the upper limb, leading first to cardiopulmonary arrest and to death four days later (Table 2). Most of these complications only required conservative treatment (86%), although several cases required abdominal paracentesis (3), pericardial drainage, pleural drainage, peritoneal dialysis, etc.
Mechanical complications.
| Type of complications | Number, percentage of catheters | Per 100 catheter days |
|---|---|---|
| Accidental dislodgment | 22 (3.6%) | 0.67 |
| Extravasation | 20 (3.3%) | 0.61 |
| Hepatic haematoma | 15 (2.5%) | 0.46 |
| Obstruction | 12 (2%) | 0.37 |
| Ascites | 8 (1.3%) | 0.24 |
| Rupture | 5 (0.8%) | 0.15 |
| Oedema | 5 (0.8%) | 0.15 |
| Portal o ductal thrombosis | 5 (0.8%) | 0.15 |
| Significant haemorrhage (requiring volume loading, increasing the dose of vasoactive drugs or red blood cell transfusion) | 3 (0.5%) | 0.09 |
| Arterial placement | 3 (0.5%) | 0.09 |
| Arterial spasm | 2 (0.3%) | 0.06 |
| Pleural effusion | 2 (0.3%) | 0.06 |
| Pericardial effusion | 2 (0.3%) | 0.06 |
| Cardiopulmonary arrest | 2 (0.3%) | 0.06 |
| Death (related to catheter complication) | 1 (0.17%) (extravasation) | 0.03 |
| Hydrocele | 1 (0.17%) | 0.03 |
| Bladder puncture | 1 (0.17%) | 0.03 |
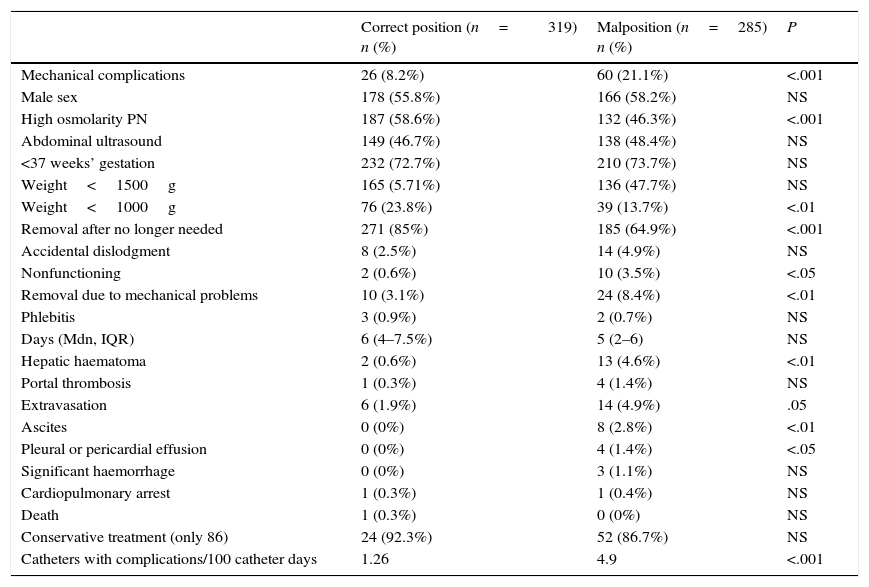
Incorrectly placed catheters were associated with a significantly greater frequency of MCs, fewer removals when the catheter was no longer required, more removals due to mechanical problems, and a higher incidence of hepatic haematoma, pleural and pericardial effusion and ascites. The number of catheters with complications per 100 catheter days was also significantly greater (Table 3).
Overall comparison of correctly and incorrectly positioned catheters.
| Correct position (n=319) n (%) | Malposition (n=285) n (%) | P | |
|---|---|---|---|
| Mechanical complications | 26 (8.2%) | 60 (21.1%) | <.001 |
| Male sex | 178 (55.8%) | 166 (58.2%) | NS |
| High osmolarity PN | 187 (58.6%) | 132 (46.3%) | <.001 |
| Abdominal ultrasound | 149 (46.7%) | 138 (48.4%) | NS |
| <37 weeks’ gestation | 232 (72.7%) | 210 (73.7%) | NS |
| Weight<1500g | 165 (5.71%) | 136 (47.7%) | NS |
| Weight<1000g | 76 (23.8%) | 39 (13.7%) | <.01 |
| Removal after no longer needed | 271 (85%) | 185 (64.9%) | <.001 |
| Accidental dislodgment | 8 (2.5%) | 14 (4.9%) | NS |
| Nonfunctioning | 2 (0.6%) | 10 (3.5%) | <.05 |
| Removal due to mechanical problems | 10 (3.1%) | 24 (8.4%) | <.01 |
| Phlebitis | 3 (0.9%) | 2 (0.7%) | NS |
| Days (Mdn, IQR) | 6 (4–7.5%) | 5 (2–6) | NS |
| Hepatic haematoma | 2 (0.6%) | 13 (4.6%) | <.01 |
| Portal thrombosis | 1 (0.3%) | 4 (1.4%) | NS |
| Extravasation | 6 (1.9%) | 14 (4.9%) | .05 |
| Ascites | 0 (0%) | 8 (2.8%) | <.01 |
| Pleural or pericardial effusion | 0 (0%) | 4 (1.4%) | <.05 |
| Significant haemorrhage | 0 (0%) | 3 (1.1%) | NS |
| Cardiopulmonary arrest | 1 (0.3%) | 1 (0.4%) | NS |
| Death | 1 (0.3%) | 0 (0%) | NS |
| Conservative treatment (only 86) | 24 (92.3%) | 52 (86.7%) | NS |
| Catheters with complications/100 catheter days | 1.26 | 4.9 | <.001 |
IQR, interquartile range; Mdn, median; NS, not significant; PN, parenteral nutrition.
High osmolarity: osmolarity>800mOsm/L.
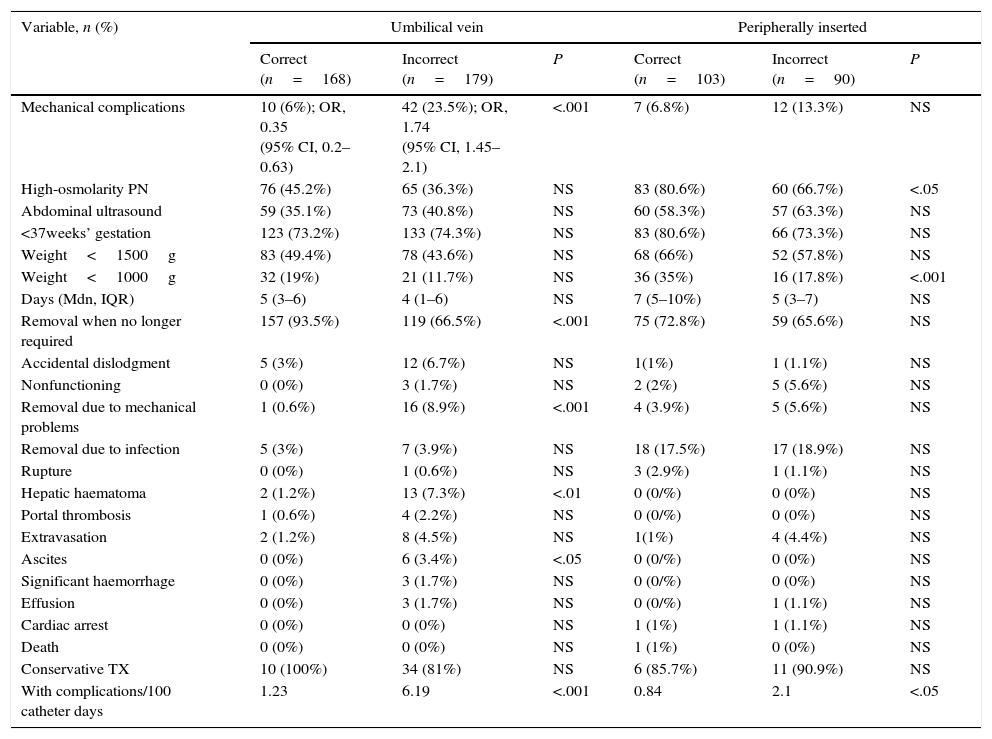
When we analysed the use of UVCs, we found that those placed incorrectly had more MCs, were removed less frequently due to no longer being required and more frequently due to mechanical problems, were associated with a higher incidence of hepatic haematoma and ascites, and corresponded to a higher number of catheters with complications per 100 UVC days (Table 4).
Mechanical complications by type of catheter and catheter position.
| Variable, n (%) | Umbilical vein | Peripherally inserted | ||||
|---|---|---|---|---|---|---|
| Correct (n=168) | Incorrect (n=179) | P | Correct (n=103) | Incorrect (n=90) | P | |
| Mechanical complications | 10 (6%); OR, 0.35 (95% CI, 0.2–0.63) | 42 (23.5%); OR, 1.74 (95% CI, 1.45–2.1) | <.001 | 7 (6.8%) | 12 (13.3%) | NS |
| High-osmolarity PN | 76 (45.2%) | 65 (36.3%) | NS | 83 (80.6%) | 60 (66.7%) | <.05 |
| Abdominal ultrasound | 59 (35.1%) | 73 (40.8%) | NS | 60 (58.3%) | 57 (63.3%) | NS |
| <37weeks’ gestation | 123 (73.2%) | 133 (74.3%) | NS | 83 (80.6%) | 66 (73.3%) | NS |
| Weight<1500g | 83 (49.4%) | 78 (43.6%) | NS | 68 (66%) | 52 (57.8%) | NS |
| Weight<1000g | 32 (19%) | 21 (11.7%) | NS | 36 (35%) | 16 (17.8%) | <.001 |
| Days (Mdn, IQR) | 5 (3–6) | 4 (1–6) | NS | 7 (5–10%) | 5 (3–7) | NS |
| Removal when no longer required | 157 (93.5%) | 119 (66.5%) | <.001 | 75 (72.8%) | 59 (65.6%) | NS |
| Accidental dislodgment | 5 (3%) | 12 (6.7%) | NS | 1(1%) | 1 (1.1%) | NS |
| Nonfunctioning | 0 (0%) | 3 (1.7%) | NS | 2 (2%) | 5 (5.6%) | NS |
| Removal due to mechanical problems | 1 (0.6%) | 16 (8.9%) | <.001 | 4 (3.9%) | 5 (5.6%) | NS |
| Removal due to infection | 5 (3%) | 7 (3.9%) | NS | 18 (17.5%) | 17 (18.9%) | NS |
| Rupture | 0 (0%) | 1 (0.6%) | NS | 3 (2.9%) | 1 (1.1%) | NS |
| Hepatic haematoma | 2 (1.2%) | 13 (7.3%) | <.01 | 0 (0/%) | 0 (0%) | NS |
| Portal thrombosis | 1 (0.6%) | 4 (2.2%) | NS | 0 (0/%) | 0 (0%) | NS |
| Extravasation | 2 (1.2%) | 8 (4.5%) | NS | 1(1%) | 4 (4.4%) | NS |
| Ascites | 0 (0%) | 6 (3.4%) | <.05 | 0 (0/%) | 0 (0%) | NS |
| Significant haemorrhage | 0 (0%) | 3 (1.7%) | NS | 0 (0/%) | 0 (0%) | NS |
| Effusion | 0 (0%) | 3 (1.7%) | NS | 0 (0/%) | 1 (1.1%) | NS |
| Cardiac arrest | 0 (0%) | 0 (0%) | NS | 1 (1%) | 1 (1.1%) | NS |
| Death | 0 (0%) | 0 (0%) | NS | 1 (1%) | 0 (0%) | NS |
| Conservative TX | 10 (100%) | 34 (81%) | NS | 6 (85.7%) | 11 (90.9%) | NS |
| With complications/100 catheter days | 1.23 | 6.19 | <.001 | 0.84 | 2.1 | <.05 |
| Variable, n (%) | Femoral vein | ||
|---|---|---|---|
| Correct (n=27) | Incorrect a (n=7) | P | |
| Mechanical complications | 4 (14.8%) | 4 (57.1%); OR, 4.3 (95% CI 1.2–15.4) | <.05 |
| High-osmolarity PN | 17 (63%) | 6 (85.7%) | NS |
| Abdominal ultrasound | 16 (59.3%) | 4 (57.1%) | NS |
| <37weeks’ gestation | 11 (40.7%) | 6 (85.7%) | NS |
| Weight<1500g | 4 (14.8%) | 3 (42.9%) | NS |
| Weight<1000g | 2 (7.4%) | 1 (14.3%) | NS |
| Days (Mdn, IQR) | 7 (4–11) | 1 (0–2) | <.05 |
| Removal when no longer required | 22 (81.5%) | 4 (57.1%) | NS |
| Accidental dislodgment | 1 (3.7%) | 0 (0%) | NS |
| Nonfunctioning | 0 (0%) | 1 (14.3%) | NS |
| Removal due to mechanical problems | 2 (7.4%) | 3 (42.8%) | <.05 |
| Removal due to infection | 2 (7.4%) | 0 (0%) | NS |
| Rupture | 0 (0%) | 0 (0%) | NS |
| Hepatic haematoma | 0 (0%) | 0 (0%) | NS |
| Portal thrombosis | 0 (0%) | 0 (0%) | NS |
| Extravasation | 1 (3.7%) | 1 (14.3%) | NS |
| Ascites | 0 (0%) | 2 (28.6%) | <.05 |
| Significant haemorrhage | 0 (0%) | 0 (0%) | NS |
| Effusion | 0 (0%) | 0 (0%) | NS |
| Cardiac arrest | 0 (0%) | 0 (0%) | NS |
| Death | 0 (0%) | 0 (0%) | NS |
| Conservative TX | 4 (100%) | 3 (75%) | NS |
| With complications/100 catheter days | 1.6 | 40 | <.001 |
IQR, interquartile range; Mdn, median; NS, not significant; PN, parenteral nutrition‘.
As for PICCs, the number of catheters with complications per 100 catheter days was greater for malpositioned catheters (Table 4). Malpositioned femoral vein catheters had more MCs, were inserted for shorter periods of time, were removed more often due to mechanical problems, were associated more frequently with ascites and corresponded to a greater number of catheters with complications per 100 catheter days (Table 4).
Using bivariate logistic regression models, the only variable that correlated to MCs was the correct or incorrect position of the catheter tip, having included as other independent variables sex, gestational age, weight at time of insertion, the number of catheter lumina and the use of high-osmolarity parenteral nutrition (>800mOsm/L) in all comparisons.
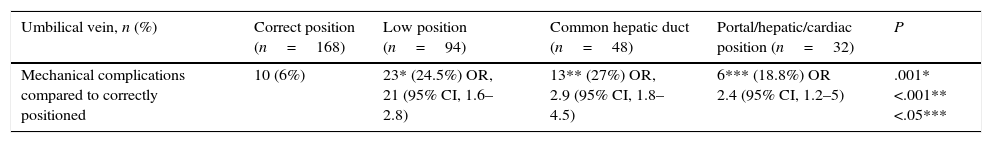
When we compared correctly placed UVCs with various incorrect positions, we found differences in the number of complications for low positions and placement at the common hepatic duct, portal, hepatic or cardiac levels compared with the correct position (Table 5).
Comparison between different incorrect positions.
| Umbilical vein, n (%) | Correct position (n=168) | Low position (n=94) | Common hepatic duct (n=48) | Portal/hepatic/cardiac position (n=32) | P |
|---|---|---|---|---|---|
| Mechanical complications compared to correctly positioned | 10 (6%) | 23* (24.5%) OR, 21 (95% CI, 1.6–2.8) | 13** (27%) OR, 2.9 (95% CI, 1.8–4.5) | 6*** (18.8%) OR 2.4 (95% CI, 1.2–5) | .001* <.001** <.05*** |
| PICC, n (%) | Correct position (n=103) | Midclavicular position (n=54) | Brachial position (n=16) | Iliac position (n=9) | Unknown or RV (n=11) | P |
|---|---|---|---|---|---|---|
| Mechanical complications | 7 (6.8%) | 10* (18.5%); OR, 1.9 (95% CI, 1.2–3) | 0 (0%)** | 1 (11.1%)*** | 1**** | <.05* NS** NS*** NS**** |
| Femoral vein, n (%) | Correct position (n=27) | Iliac position (n=3) | Not localised and other (n=4) | P |
|---|---|---|---|---|
| Mechanical complications | 4 (14.8%) | 3 (100%)* | 1 (25%)** | <.01* NS* |
NS, not significant; PICC, peripherally inserted central catheter; RV, right ventricle.
When it came to PICCs, there were more complications in midclavicular catheters compared to correctly placed ones. These differences were not found in comparison to other positions (Table 5). When we compared correctly placed femoral catheters compared to those in the iliac position, we found more MCs in the latter.
Only 20 UACs were inserted, and MCs were found in three cases (one nonfunctioning catheter and two cases of arterial spasm), which were managed with conservative measures. Of the 10 jugular vein catheters that were inserted, there were complications in four – two local extravasations and two accidental dislodgments – that were managed conservatively.
DiscussionThe management of CCs is still based on indications that are not supported with evidence.7 There is a general trend towards a less frequent use of the umbilical vein, although UVCs continue to be used most frequently in our unit. The implementation of training activities and the standardisation of the use of umbilical catheters is associated with a decrease in the number of infants that undergo catheterisation that is not accompanied by an increase in the use of PICCs or poorer outcomes.8 Other authors have found no benefits in the use of PICCs following the use of UVCs compared to keeping the UVC inserted for longer periods of time.9
Studies on CCs usually focus on infectious complications and tend to neglect MCs.3 There is broad variability in defining which complications fall into this category, there are few reports of such complications leading to poor outcomes, and the association between catheter position and the incidence of complications is seldom studied. A study of 1285 umbilical catheters reported two cases of pleural effusion and twenty-six instances of accidental dislodgement that were not clinically relevant.10 Another study that analysed data for 489 umbilical catheters also found no relevant MCs.11 A study12 of 939 PICCs found insertion-site or mechanical complications in 21.8%, consisting mainly of phlebitis (9.5%), accidental dislodgment (7.1%) and extravasation (0.4%), none of which were severe.
In our study, the percentage of MCs was 14.2%, similar to the frequencies reported in the literature, which range between 15% and 39%.9
Mechanical complications have been associated with the type of catheter used, gestational age, the number of lumina, the weight at the time of insertion and the duration of use, and one of the best-known risk factors for MCs is incorrect tip position.5,13 Accurate placement of the tip at the actual midline is a very important aspect, as studies in cadavers of extremely low birth weight preterm newborns show a significantly smaller outer diameter of the subclavian vein in relation to the brachiocephalic position (2.6 and 2.5mm for the left and right subclavian veins; and 3.3 and 4mm for the right and left brachiocephalic veins).14 Jain et al.5 analysed the data on 319 PICCs comparing correct placement with the midclavicular, brachiocephalic and iliac positions, and found a higher incidence of MCs in midclavicular catheters compared to the other categories, as we did in our study. Other authors15 have found fewer complications in centrally-positioned catheters compared to the rest, although they considered the midclavicular position to be a central position. A study of 980 PICCs16 found phlebitis in 30.3% and two deaths. One retrospective study that analysed 61 PICCs17 found phlebitis in 21.3%, accidental dislodgment in 3.2%, proximal rupture in 3.2%, two cases of pleural effusion and one of rupture of the metallic guide wire.
In our study, we found a significantly higher incidence of MCs in UVCs, femoral catheters and PICCs that were not positioned in the midline.
The complications described in the literature include cases of portal hypertension, vessel perforation, air embolism,3,13 catheter tip migration, extravasation, venous thrombosis, hepatic lesions, intestinal necrosis, pulmonary embolism, arrhythmia, SVC syndrome, low cardiac output secondary to tip placement in the left atrium,18 retroperitoneal abscess, extravasation in the renal pelvis,19 spinal cord compression, ascites and death20 secondary to peripherally-inserted or femoral catheter tip placement in the ascending lumbar vein,21 among others. There are cases of catheter rupture in which fragments remain inside the heart, requiring heart surgery or percutaneous approaches for their removal, or in which removal is very difficult despite the catheter remaining in one piece.22,23. In our study, we observed two cases of pleural effusion (0.3%), one of which required pleural drainage. There have been descriptions of catheter migration to the pulmonary artery and sometimes the pulmonary veins through the left atrium or through perforation of intrathoracic vessels.24
There were two cases of pericardial effusion in our series (0.3%), both in PICCs placed in an upper limb, one of which was associated with cardiac tamponade and required pericardiocentesis. Pericardial effusion/tamponade occur in between 1% and 3% of inserted lines,25 although it is believed that their incidence is underestimated. There is disagreement as to whether intra-atrial tip placement is associated to their development. A study conducted in response to four deaths due to cardiac tamponade26 found only one such case (0.05%) in a total of 2186 PICCs,27 out of which the tip was located in the right atrium in 56%. Still, most authors consider that there is a higher risk of cardiac tamponade if the catheter tip is positioned at an angle due to the resulting trauma and pressure on the cardiac wall. The literature includes descriptions of cases of pericardial effusion associated with correctly placed UVCs,28 which has led other authors to propose that the tip should not only remain outside the heart, but also outside the intrapericardial region of the venae cavae, at least 1cm away in preterm newborns and 2cm away in infants born to term.5,6 The website of the Food and Drug Administration recommends that the tip be placed outside the heart.29
Many published studies do not provide data on thrombosis, as assessments for this complication are not performed routinely. In our study, we found five cases (0.8%) of portal or hepatic thrombosis, and did not find any others. One study that used serial ultrasound30 found clinically silent portal vein thrombosis in 43% of participants, with sonographic resolution in 55.5% at 73 days’ followup. Other authors have found an incidence of portal thrombosis as low as 1%.31
Most complications required conservative management, such as catheter removal or replacement. Complications such as hepatic haematoma or portal thrombosis may tend to develop late. There is evidence of the risk of portal hypertension in neonates secondary to portal thrombosis due to UVC use, with a prevalence of outcomes such as portal hypertension or left lobar atrophy of up to 27%.32
A study of 42 femoral vein catheters placed in newborns33 found that 64% were removed when they were no longer required. Another study in 34 newborns34 found four MCs that required removal of the catheter and four cases of transient venous congestion of the distal limb.
Umbilical arterial catheters are rarely used in our unit. While some authors recommend their use in infants born at fewer than 26 weeks’ gestation,8 we use them based on clinical severity.
The percentage of successful UVC placement ranges between 85% and 95%,35 although a clear definition of what is meant by correct placement is rarely given. The percentage found in our series was 48.7%, which was probably due to a more stringent definition. Other authors36 have found a sensitivity of 45% and a specificity of 87% in the use of chest radiography to verify the actual position of the catheter tip. The estimation of catheter tip position based on external landmarks and mathematical equations has little validity for the determination of the final position,37 and some authors recommend the use of bedside ultrasound to localise the tip of UVCs or PICCs, as it is more effective in localising the catheter tip than plain radiography, even when it is performed by neonatal clinicians.38
The classification of correct final placement is a dynamic concept. At times, the catheter migrates as it is being secured after performance of the X-ray. Catheters inserted peripherally through the basilic, cephalic or axillary vein can move up to 2cm with arm abduction and adduction or flexion of the elbow, so that a correctly placed catheter could inadvertently end in an intracardiac position. This means that placement should be verified through time39 or that radiographic confirmation should be performed in the maximum-depth position. Umbilical vein catheters can migrate to more central positions due to the retraction and atrophy of the umbilical cord in the first days of life. There have also been reports of the spontaneous correction of the position of incorrectly placed catheter tips. Other authors have found an association between the frequency of complications in PICCs as a function of the site of insertion,40 with the incidence being lowest in catheters inserted in the axillary vein.
The complications of UACs were similar to those of UVCs, and also included vasospasm, seen in two catheters, although we did not observe thrombosis in any, possibly due to the low number of UACs.
There are limitations to our study. In addition to those characteristic of a descriptive study, it is possible for some catheters to have migrated after having been categorised as correct or incorrect. Ultrasound was rarely used to verify tip placement (<2%) and the potential presence of intracardiac thrombi was not assessed routinely. In many cases, we could not determine whether the catheter had migrated before complications arose in catheters that had been placed correctly. The position of the arm at the time of radiographic examination was not documented. Furthermore, we included the data of all catheters placed in each child, as opposed to only the first one, which may have influenced the complications that developed in subsequent catheters. We did not analyse late complications.
ConclusionsIn our study, the use of CCs was associated with mechanical complications, many of which had to do with the position of the catheter tip. Incorrect tip placement was associated with a higher frequency of MCs, removal due to mechanical problems, extravasation, pleural and pericardial effusion, hepatic haematoma and ascites.
Midclavicular PICCs were associated with a higher risk than PICCs with the tip in the midline or in a brachiocephalic position. Low positions and other incorrect positions of UVCs were associated to a higher frequency of MCs.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Lloreda-García JM, Lorente-Nicolás A, Bermejo-Costa F, Fernández-Fructuoso JR. Complicaciones mecánicas asociadas a la localización de la punta de catéteres centrales en una unidad neonatal. An Pediatr (Barc). 2016;85:77–85.
Previous presentations: This study was presented as an oral communication to gain full membership in the Sociedad Española de Neonatología (Spanish Society of Neonatology) at XXV Congreso Nacional de Neonatología y Medicina Perinatal, May 2015, Seville, Spain.