Family access to NICUs has benefits for the newborn (NB) and family, as the main way of humanised care.
ObjectiveTo determine the current state of parents and families access to NICUs in Latin America.
MethodsA cross-sectional study was conducted in 15 countries using two questionnaires: (1) directed at head nurses with management and supervision activities, and (2) nurses with care tasks. The features and modes of functioning were examined; the use access guides, personal opinion on the rights to enter, risks, interference, or collaboration as regards the patient, and nursing role in decisions. Nursing leaders of each country identified contacts and obtained authorisation under the regulations of each country. The responses were analysed centrally with the participants remaining anonymous.
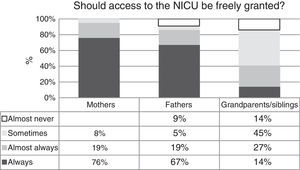
ResultsOut of 640 questionnaires issued, responses were received by 226 (35%). Among 52 NICU, 63% have a place for mothers to stay (only 27% overnight), and in 31 (60%) there are notices with fixed schedules for visiting the NB. Unrestricted access exists in only 19 NICU (36%), but for siblings and grandparents it is more restricted (it is not possible in 29%). Among the 174 nurses that responded, 76% feel that mothers should always have access, but these percentages decrease for fathers, siblings and grandparents. A large majority (77%) believe that nursing staff would favour access, and 35% would make it difficult. In addition, 48% believed that access interferes with nursing care.
ConclusionA cultural change is needed in the NICUs in Latin America in order to respect the rights of newborns and their families during hospitalisation.
El ingreso de la familia en UCIN trae beneficios al RN y su familia, como eje de la atención humanizada.
ObjetivoConocer el estado actual sobre acceso de padres y familias en UCIN de Iberoamérica.
MétodosEstudio transversal en 15 países de Iberoamérica. Dos cuestionarios: 1) para enfermeros jefes con tareas de gestión y conducción, y 2) para enfermeros en tarea asistencial. Se exploró sobre características y modalidades de funcionamiento; uso de guías de acceso, opinión personal sobre derecho a ingresar, riesgos, interferencias o colaboración relacionadas al ingreso, y papel de enfermería en las decisiones. Líderes de enfermería de cada país identificaron contactos y obtuvieron autorización según regulaciones de cada país. Las repuestas fueron analizadas en forma centralizada sin identificación del participante.
ResultadosSeiscientos cuarenta cuestionarios; respuesta en 226 (35%). Entre 52 UCIN, el 63% dispone de lugar para estancia de madres (solo el 27% durante la noche); en el 31 (60%) existen carteles que indican sobre horarios fijos para «visitas» de padres. El ingreso irrestricto existe en solo 19 UCIN (36%); para hermanos y abuelos es más restringido (en el 29% no es posible). Entre las 174 enfermeras, el 76% considera que las madres deben acceder siempre, pero estos porcentajes disminuyen para padres, hermanos y abuelos; el 77% opina que enfermería favorece y el 35% que dificulta el acceso. Adicionalmente, el 48% opina que el ingreso interfiere con tareas de enfermería.
ConclusiónEs necesario un cambio cultural en las UCIN de Iberoamérica para que se respeten los derechos de los RN y sus familias durante la internación.
Healthy newborns (NBs) start to develop an intimate attachment to their parents in the delivery room, after which they move into the rooming-in area without separating from their families. Conversely, preterm or ill NBs require care in neonatal care units with various human and technological resources and levels of complexity depending on the severity of their condition.
Newborns stay in such Neonatal Intensive Care Units (NICUs) from a few days to months to undergo diagnostic and therapeutic interventions aiming at resolving or improving their problems. This environment, populated by health care professionals, equipment, noises and lights, among others, is often intimidating to the family. Thus, the hospitalisation of the neonate interferes in varying degrees with the bonding of NBs and their families.
It is not uncommon for NICUs to operate in ways that tend to restrict the presence of parents and other family members by the sick child. However, the evidence on the importance of the mother's presence next to the baby and the need to promote family-centred care has been growing since the 1980s.1–4
Among other things, unrestricted access during hospitalisation helps parents regain their central role, improve the self-esteem that may have been lost with the arrival of a child that was not as they had imagined, and shift feelings of anticipatory grief, conceiving the real possibility of a fulfilling present and future life. Furthermore, research has shown that the close presence of parents in the NICU facilitates the recovery of the NB and is associated with a reduction in the length of stay of preterm NBs.5 In spite of this, recent studies conducted in Europe have shown that unrestricted parental access is not yet widely practised or accepted.6 A programme that allows the unrestricted access of parents to the NICU should be supplemented with additional actions that foster family bonding, such as directed sibling and grandparent visits. These are all key experiences that provide significant emotional support to the parents and are very rewarding for health care professionals.7
Today, it is indisputable that hospitalised NBs have the right to be accompanied by their family as much as possible, and that the unrestricted access of the mother to the NICU is a cornerstone of upholding the rights of the mother and child. The morbidity and mortality rates vary widely between countries in Latin America, and it is not known whether there is also variability in how health care teams approach the access of families to the NICU.
The quality and outcomes of neonatal care are directly correlated to having enough nursing professionals on staff with adequate training, attitudes and behaviours. It is likely that this is also necessary for humane care to become the norm. Within the Sociedad Iberoamericana de Neonatología (Ibero-American Society of Neonatology [SIBEN]), the Nursing Chapter carries out an extensive educational activity through a network of nurses that operate in different countries of Latin America and Spain. Within this framework, and with the support of the SIBEN, we decided to conduct a study with the aim of learning the current approach to family access to the NICU in Latin American countries. More specifically, we explored the organisational approaches to access to the NICU and analysed the opinions of nurses regarding family rooming-in and the potential role of the nursing staff in leading the changes required to eliminate barriers to access.
Materials and methodsWe conducted a cross-sectional study, administering questionnaires to nurses employed in Latin American NICUs between May 1 and July 30, 2014.
We developed two different questionnaires using a standardised process that consisted in defining the dimensions and then developing, reviewing and reducing the questions by consensus. We conducted a pilot test to assess the comprehension and consistency of all questions. Finally, we edited the questionnaires and produced the final version that was administered online.
We categorised the recipients or respondents of each questionnaire into two groups:
- –
Head nurses in management and leadership roles: to assess organisational, functional and environmental factors that facilitate or hinder parental access to each NICU.
- –
Nurses that deliver patient care: to learn the opinions and attitudes regarding the presence of parents and family members in the NICU, and how nurses perceive their role in the facilitation or promotion of potential changes.
The questionnaire for head nurses consisted of 26 multiple-choice questions organised in two dimensions: unit characteristics (infrastructure and family-friendly features) and approaches (rules regarding access, family involvement in the care of the NB and decision-making processes). The questionnaire for nurses involved in patient care consisted of 24 items with answers on a Likert scale8 (ranging from “totally agree” to “totally disagree”) on the use of access guidelines, personal opinion on who should be granted access to the NICU, risks and interferences related to access, and the role of nurses in decision making.
We sent the invitation to participate in the study by electronic mail from the coordinating centre. The message included a link to the website where each of the questionnaires could be completed in a confidential and anonymous manner, and the only data that linked each response to the respondent were the country and the type of unit.
We requested the participation of nurses working in the NICUs of maternity units in Latin America that attend more than 1500 deliveries and/or have more than 250 neonatal admissions per year. The units were selected with the help of nursing leaders in each country that identified the units and contacts in each city; we provided these leaders with a full copy of the study protocol so they could obtain approval for the study in compliance with the current legislation and regulatory bodies in each country.
We entered all the answers in a database and made a descriptive analysis of the data by means of frequency tables and graphs, using percentages, means and standard deviations or medians and ranges as appropriate.
ResultsWe sent out 640 questionnaires. We obtained 226 completed responses (35%). Table 1 shows the frequency of questionnaire submissions and responses per country, reflecting a high variability.
Access of Families to Inpatient Neonatal Units in Latin America: in need of improvement.
| Country | Sent questionnaires | Responses | Response rate (%) |
|---|---|---|---|
| Argentina | 92 | 38 | 41.3 |
| Bolivia | 8 | 5 | 62 |
| Brazil | 3 | 0 | 0 |
| Chile | 32 | 20 | 62 |
| Colombia | 21 | 13 | 62 |
| Costa Rica | 2 | 0 | 0 |
| Cuba | 15 | 15 | 100 |
| Ecuador | 4 | 2 | 50 |
| El Salvador | 18 | 5 | 28 |
| Spain | 139 | 36 | 26 |
| Honduras | 1 | 1 | 100 |
| Mexico | 23 | 10 | 43.5 |
| Peru | 106 | 37 | 35 |
| Uruguay | 33 | 13 | 39.4 |
| Venezuela | 143 | 30 | 21 |
| Total | 640 | 226 | 35.3 |
We obtained responses from 52 head nurses from NICUs in 13 countries: Argentina (11), Spain (10), Uruguay (9), Mexico (5), Chile (4), Peru (3), Bolivia (2), Colombia (2), El Salvador (2), Venezuela (1) Honduras (1), Cuba (1) and Ecuador (1). Their units attended an average of 4020 deliveries per year, and 42% had more than 500 neonatal admissions per year.
Sixty-three percent of respondents (33 NICUs) reported having a specific area to accommodate families, but only 27% of these spaces were available overnight, while 29% of respondents considered that the available space was insufficient. Thirty-three NICUs (63%) had areas for rooming-in and forty NICUs (78%) had lactation rooms. Thirty-one units (60%) had posted notices indicating the fixed “visiting” hours for parents, and 48% had intercoms that could be used to request access. Furthermore, forty-four NICUs (84%) handed out written materials (such as pamphlets) informing of the rules regarding access (Table 2).
Features of the organisation of 52 NICUs in Latin America.
| Feature | NICUs that report having this feature N (%) |
|---|---|
| Space for families during the day | 33 (63) |
| Space for families at night | 14 (27) |
| Sufficient space | 15 (29) |
| Rooming-in | 33 (63) |
| Lactation room | 40 (77) |
| Posters showing the hours access is allowed | 31 (60) |
| Intercoms | 25 (48) |
| Written information regarding access rules | 44 (84) |
There was wide variability in the policies regarding family access to the NICU, and we classified them into four categories for the descriptive analysis: unrestricted access (24h a day requiring no prior notice), unscheduled (24h a day, after obtaining permission), with fixed schedules, or with fixed schedules only in the daytime. Table 3 presents the types of access granted to mothers and fathers, showing that only 36% of respondents reported unrestricted access to their unit. Half of the units informed parents at scheduled times. Access was generally more limited for siblings and grandparents; only 36% of the units (n=19) allowed access every day of the week; 29% (n=15) allowed them access once a week; 6% (n=3) allowed access exceptionally, and the remaining 29% (n=15) never allowed them access.
As for the participation of parents in the care of the baby, 48 NICUs (92%) allowed it, and it mainly involved activities related to NB feeding and hygiene. However, the participation or presence of parents during procedures was minimal (22% of respondents reported that parents were never allowed to accompany their child, 26% only allowed their presence in minor procedures, and 34% allowed their presence only in exceptional occasions). Only nine units (18%) allowed parents to be present in any of the procedures if they requested it.
Eighty percent of participants reported that there were specific guidelines regarding the access of families to the NICU, but only ten percent reported that nurses had been involved in the development of these guidelines.
The second questionnaire was completed by 174 nurses involved in patient care in 12 Latin American countries; 74% worked in public health systems and 96% were female. Fig. 1 presents their opinion on granting unrestricted access to the NICU to mothers, fathers, grandparents or siblings. While 76% answered that mothers should always be granted access, the percentages were progressively lower for fathers, grandparents and siblings. Of all respondents, 48% believed that the presence of parents interferes with nursing tasks and 41% that the presence of the mother interferes with the sleep of the NB. When we explored the involvement of parents in the NICU, 40% of respondents reported that parents always participate in the care of the NB and 46% believed that this was important for patient safety.
Finally, we explored how nurses perceived their role, and the extent to which they believed their approach facilitated or obstructed (posed barriers to) parental access to the NICU: 77% stated that they facilitated access, and 35% that they obstructed it (Table 4).
Of the 174 nurses, 118 (68%) considered that ultimately the decision to grant access rests with the nurses, and 89 (51%) believed they were in a position to change the rules regarding family access to their units. More than 80% believed that physicians were aware of the rules and believed that they agreed with them, but 77% reported that they did not adhere to the rules.
Searching for differences or heterogeneous practices between countries was not an a priori objective of our study, since, as we explained in Methods and at the beginning of this section, participation was voluntary and varied widely. We did a post hoc analysis of potential variations between regions for some of the questions. Table 5 summarises the attitudes regarding granting access to mothers, fathers and grandparents by country and overall, and shows variability, although in most countries fathers were considered to be less entitled than mothers to access, and the rights of grandparents were seldom acknowledged (0–45%). Table 6 assessed whether there were differences between countries in the degree to which nurses facilitated or hindered access.
Perception of nurses regarding unrestricted access to the NICU for mothers, fathers, and grandparents by country (n=174 responses).
| Country | Number of nurses that answered | Answered mothers should “always” have access | Answered fathers should “always” have access | Answered grandparents should “always” have access |
|---|---|---|---|---|
| Argentina | 26 | 92% | 81% | 29% |
| Bolivia | 3 | 100% | 100% | 0% |
| Chile | 17 | 82% | 76% | 12% |
| Colombia | 11 | 91% | 90% | 45% |
| Cuba | 14 | 57% | 7% | 0% |
| Ecuador | 2 | 100% | 100% | 0% |
| El Salvador | 3 | 100% | 100% | 0% |
| Spain | 26 | 54% | 65% | 7% |
| Mexico | 5 | 60% | 60% | 0% |
| Peru | 34 | 88% | 68% | 9% |
| Uruguay | 4 | 75% | 75% | 0% |
| Venezuela | 29 | 65% | 58% | 14% |
| Mean±SD, 80±17% Median 85% | Mean±SD, 73±26% Median 76% | Mean±SD, 10±14% Median 4% |
Nurses as facilitators or barriers to family access to the NICU by country (n=174 responses).
| Country | Number of nurses that answered | Answer: nurses “always” facilitate access | Answer: nurses “always” obstruct access |
|---|---|---|---|
| Argentina | 26 | 48% | 7% |
| Bolivia | 3 | 67% | 0% |
| Chile | 17 | 41% | 12% |
| Colombia | 11 | 82% | 18% |
| Cuba | 14 | 21% | 43% |
| Ecuador | 2 | 100% | 0% |
| El Salvador | 3 | 33% | 0% |
| Spain | 26 | 27% | 0% |
| Mexico | 5 | 40% | 0% |
| Peru | 34 | 59% | 3% |
| Uruguay | 4 | 25% | 25% |
| Venezuela | 29 | 41% | 7% |
| Mean±SD, 49±24% Median 41% | Mean±SD, 10±13% Median 5% |
There is much left to do to protect the rights of NBs and their families in Latin American NICUs. The data show that while the infrastructure and organisational approach of the units pose some barriers, there is also a great variability in the attitudes of nurses. Building new units or modifying structures to meet published standards9 for promoting the wellbeing of the family is certainly costly, but research has proven that family-centred practises such as kangaroo care do not depend on the availability of material resources.10 It has been said that each NICU is, in a way, a culture of its own, and that some NICUs also have subcultures corresponding to different nursing shifts. It is difficult to change a culture without changing personal attitudes and approaches.
Overall, the results of our study show that the situation of parents, grandparents and siblings is less favourable than that of the mothers of NBs, who are necessarily involved in some basic aspects of care, for instance in maintaining lactation. The key role of the mother in the household is unquestionable,11 but we cannot ignore the roles and needs of other family members.
It is worth noting that a high percentage of nurses believed that nurses are capable of promoting change and making decisions regarding access, and therefore strategies for raising awareness and educating nurses could have an actual impact on the protection of the rights of children and their families. Two studies conducted in Spain (2006 and 2013) suggest that this aspect can be improved by means of training and awareness-raising.12,13
The disparities found in this study confirm what we could infer from other publications from different periods in some countries in Latin America. For instance, starting in 1988, some authors in Argentina implemented the unrestricted access of parents to the NICU (especially the mother) by setting up areas where babies that were still unwell could be with their mothers around the clock with the purpose of promoting attachment and facilitating the transition from the NICU to the home, which they called “neonatal recovery” areas.14 However, a survey conducted in Argentina 22 years later15 still showed a high variability in the protection of NB rights. A study conducted in Madrid16 measured the time that mothers spent each day with their hospitalised NBs, and 85% of mothers stated that they wanted to spend more time with their children. Another study in Spain12 reported that 82% of the 27 units under study already offered unrestricted access to parents. The unrestricted access of parents and their increased participation in the care of their children has spread rapidly through units in the United States, Canada, Australia and Western Europe.17
However, studies conducted recently in American countries such as Mexico18 have reported that the only types of access offered consist of restricted access after obtaining permission, and that maternal involvement in care is limited and takes place within strict schedules in the absence of a defined programme. As occurs in the units from several countries that participated in our study, mothers in Mexico provide some basic feeding and hygiene care, but their participation in procedures is not considered a health care standard.
The presence of parents during the performance of procedures in children is highly controversial. A study conducted in Argentina19 showed that despite being aware of the benefits of having a family member accompany the child, most centres only allowed the presence of parents in minimally invasive procedures and systematically excluded them from more invasive procedures because their presence could cause anxiety in the provider performing the procedure.20 While many providers consider that parents may be traumatised by watching their children undergo procedures, others believe that being unable to be by their children when they are suffering, in pain or under stress may be much more traumatic to parents.21 Recent studies22,23 have shown a strong correlation between parental participation in the care of the child and parental satisfaction. Furthermore, there is evidence that the incidence of post-traumatic stress in mothers is greatly reduced if they are allowed frequent contact with their ill children, and that the outcomes of neonatal care are good when the care is family-centred and parents are the main caregivers of the NBs.24,25
There are some limitations to our study. The response rate only reached 35%, and we cannot be certain that the results would be similar if the remaining nurses that chose not to participate had responded. We were also unable to determine what motivated these nurses to not answer, as access to the platform was very simple and confidentiality and anonymity were guaranteed in all cases, as a central coordinator unlinked the email address immediately after receiving the questionnaire and no personal identifiers were included in the database of the analysis. We can only assume that if the reason for not answering in some cases had been a lack of interest in the subject, the results would probably be even more alarming.
Furthermore, as occurs in studies with this type of design, we have no way to ascertain that the answers are an accurate reflection of the attitudes and behaviours in actual clinical practice. There may be a bias towards answering according to what is considered to be correct. Although we planned for and had the collaboration of local nursing leaders to recruit nurses and nurse supervisors in each region, we obtained a convenience sample, so it is uncertain that the sample is representative or its results can be generalised to all other units.
We also believe that there are strengths, given the participatory approach of many units in several countries. The possibility of participating in the activity of a society such as SIBEN, which links nursing and medicine professionals devoted to neonatal care in different regions of Latin America to promote cooperation, offers an unparalleled opportunity to become acquainted with and reflect on aspects of the quality of care received by NBs in our region, and to contribute to improving its quality in Latin American countries.
We have come to the conclusion that:
- –
The unrestricted access of parents to the NICU is a cornerstone of human neonatal care, yet it is not practised in a high percentage of Latin American units.
- –
A cultural change in the attitude of health care professionals ought to happen in the short-term to pursue universal unrestricted access.
- –
Nurses play a key role and can be leaders in this change.
The authors have no conflict of interests to declare.
We want to thank the health care professionals (nurses and supervisors) that work in neonatal units in the different countries that participated in the survey.
María del Carmen Fontal (Uruguay), Aldana Ávila (Argentina), Cristina Segovia (Spain), Noemí Ruiz Lavado (Peru), Irama López (Venezuela), Laura Álvarez (Mexico), Amparo del Socorro Acosta Polo (Colombia) and Zandra Grosso (Colombia).
Please cite this article as: Montes Bueno MT, Quiroga A, Rodríguez S, Sola A, miembros del Capítulo de Enfermería de SIBEN. Acceso de las familias a las unidades de internación de Neonatología en Iberoamérica: una realidad a mejorar. An Pediatr (Barc). 2016;85:95–101.
The participants that were members of the Nursing Chapter of the SIBEN are listed in Appendix A.
Previous presentations: This study has been presented at the XI Congreso Anual and IX Congreso del Capítulo de Enfermería de SIBEN; August 20–23, 2014; Mexico DF, Mexico.