Inappropriate habits in the storage of potentially toxic substances, such as the use of non-original containers, may facilitate unintentional acute poisonings in the paediatric age group1 and have been associated with a potentially greater severity,2 although few studies provide evidence on this subject.
The main aim of our study was to analyse whether unintentional acute paediatric poisonings by substances stored in non-original containers are more severe than the rest of poisonings. Our secondary objective was to learn the characteristics of these poisonings.
We conducted a descriptive study based on a prospective register of the cases of poisoning documented in the 59 paediatric emergency departments (PEDs) that participate in the Observatorio Toxicológico (Toxicology Surveillance System) of the Sociedad Española de Urgencias de Pediatría (Spanish Society of Paediatric Emergency Medicine) between October 2008 and September 2014. We determined severity based on diagnostic tests, the treatment received, admission to hospital or the paediatric intensive care unit, sequelae and fatalities.
The study was approved by the Committee of Ethics and Clinical Research of the Basque Country.
The participating hospitals are listed in Appendix 1.
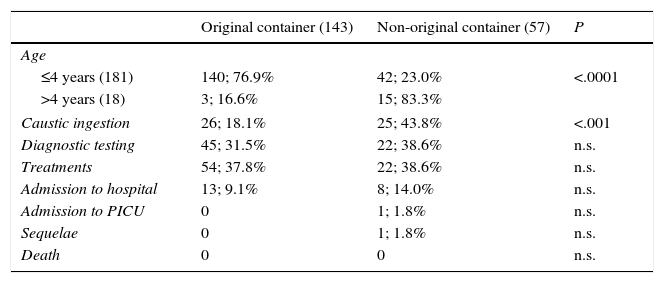
During the period under study, the 59 PEDs received 339086 visits, of which 902 corresponded to poisonings. Out of all poisoning cases, 639 were unintended, and the type of container in which the substance was stored was documented in 611 (95.6%). In 100 of these cases (16.3%), the toxic substance had not been stored in its original container, a circumstance that was more common in cases of poisoning with household products (57/200 [28.5%]; 95% CI, 22.2%–34.7%) than in cases of poisoning with medications (31/341 [9.0%]; 95% CI, 5.9%–12.0%). Table 1 compares the characteristics of the 200 unintentional acute poisonings with household products based on the type of container used for storage.
Characteristics of unintentional acute poisonings with household products by type of storage.
| Original container (143) | Non-original container (57) | P | |
|---|---|---|---|
| Age | |||
| ≤4 years (181) | 140; 76.9% | 42; 23.0% | <.0001 |
| >4 years (18) | 3; 16.6% | 15; 83.3% | |
| Caustic ingestion | 26; 18.1% | 25; 43.8% | <.001 |
| Diagnostic testing | 45; 31.5% | 22; 38.6% | n.s. |
| Treatments | 54; 37.8% | 22; 38.6% | n.s. |
| Admission to hospital | 13; 9.1% | 8; 14.0% | n.s. |
| Admission to PICU | 0 | 1; 1.8% | n.s. |
| Sequelae | 0 | 1; 1.8% | n.s. |
| Death | 0 | 0 | n.s. |
When it came to poisoning with medications, those that involved substances stored in non-original containers corresponded more frequently to combined drug intoxications (6/31 [19.3%] compared to 13/310 [4.2%] of unintentional poisonings with medications stored in their original containers; P<.005), and involved psychotropic drugs more frequently (12/31 [38.7%] compared to 56/310 [18.0%]; P<.05), with no differences between age groups or in severity. When we analysed the data for cases in which the setting of the poisoning was documented, we found that these poisonings occurred most frequently in the parents’ bedroom (8/31 [25.8%] vs 33/297 [11.1%]; P<.05).
The percentage of the total of unintentional acute paediatric poisonings associated with inappropriate storage was not insignificant, especially for poisonings involving household products.
In spite of preventive campaigns, up to 15% of unintentional acute poisonings result from the ingestion of products stored in non-original containers. Our study raises a red flag on the frequency of this type of poisonings, even though it is rare for them to be studied specifically.3,4 While there is no evidence on the impact of health education on the prognosis of acute paediatric poisonings,5 we believe that it is important to inform the population and paediatricians on this type of unintentional poisonings. These poisonings are particularly common in patients aged more than 4 years, in whom more than 90% of poisonings with household products are associated with inappropriate storage, especially of caustic substances. This fact may be related to the inappropriate habit of adults of storing such toxic substances in containers as common as plastic bottles, which children associate with harmless contents.
One salient finding of our study was the characteristics of medication poisonings related to inappropriate storage. The percentage of combined drug intoxications was significantly higher in these patients. The fact that such poisonings occur in the parents’ bedroom and frequently involve benzodiazepines emphasises the need to improve health education efforts in our population.
There are various limitations to our study. The prospective register did not document the type of container used by families to store the substances involved in the poisonings. This information would be helpful to design more specific preventive interventions, although its absence did not compromise the aims of the study.
While this type of storage is not associated with a potentially greater severity in poisoning cases, preventive strategies should contemplate providing health education on the storage and conservation of household products.
H. Alto Deba: Agustín Rodríguez; H. del Tajo, Aranjuez: Carlos García-Vao; H.U. Arnau de Vilanova, Lleida: Neus Pociello; H.U. Basurto: Javier Humayor; H. Cabueñes: Ramón Fernández; H.U. Carlos Haya: Silvia Oliva Rodríguez-Pastor; Complejo Hospitalario de Jaén: Tomás del Campo; C. Asistencial Universitario de León: Ana Gloria Andrés; Corporación Sanitaria Parc Taulí, Sabadell: Mireia Pérez; H.U. Cruces: Paula Santiago, Nerea Bilbao; H.U. Doce de Octubre: Sofía Mesa; H.U. Donostia: José Angel Muñoz Bernal; H.U. Dr. Peset. Valencia: J. Rafael Bretón Martínez; H.U. Fuenlabrada: Rocío Rodríguez; H. Francesc de Borja de Gandía: Carlos Miguel Angelats; Fundació Sant Hospital de la Seu d’Urgell: Pablo Javier Ercoli; H. Universitario Fundación Alcorcón: Alberto Barasoain; H. General Universitario de Alicante: Olga Gómez Pérez; H.U. Gregorio Marañón: Paula Vázquez; H. Infanta Cristina, Parla, Madrid: Begoña de Miguel; H. de Terrassa: Judit Barrena; H. Laredo: Ana Jorda; H.U. Lucus Augusti: Sandra Yáñez; H. Mendaro: Laura Herrero; H.U. Mutua Terrassa: Elena May Llanas; H.U. Niño Jesús: Juan Carlos Molina; H. Materno-infantil de Las Palmas de Gran Canaria: Lily Mangione; H. Materno-infantil de Badajoz: Paz Hurtado; H. Ntra. Sra. de Sonsoles, Ávila: Helvia Benito; H. Montepríncipe, H. Sanchinarro, H. Torrelodones, Madrid: Silvina Natalini; H. Príncipe de Asturias, Alcalá de Henares: M. Angeles García Herrero; H.U. Puerta de Hierro Majadahonda: Consuelo Benito Caldés; H. Rey Juan Carlos: Pablo Bello Gutiérrez; H.U. San Agustín: Juan Cózar Olmo; H.U. Río Hortega, Valladolid: Roberto Velasco; H. Sant Joan de Déu, Xarxa Hospitalaria i Universitaria de Manresa. Fundació Althaia: Eva Botifoll García; H.U. Sant Joan de Déu: Lidia Martínez Sánchez; H. Sant Joan de Reus: María Rimblas; H. San Pedro: Laura Martínez; H. Miguel Servet: Carmen Campos Calleja; H.U. Son Espases, Palma de Mallorca: Victoria López Corominas; H. Son Llàtzer: Carmen Vidal Palacios; H.U. Central de Asturias, Oviedo: Julián Rodríguez; H. Universitario de Salamanca: Javier López Ávila; H.U. Virgen de la Arrixaca: Carlos Pérez; H. Virgen de la Salud, Toledo: Esther Crespo Rupérez; Complejo Hospitalario de Navarra: Miriam Palacios; H. Zumarraga: Amalia Pérez; Fundación H. de Nens, Barcelona: Amalia Arce Casas; H. Quirón, Bizkaia: Itziar Iturralde; H. Clínico U. Lozano Blesa: Gonzalo González García; H.U. Puerta del Mar, Cadiz: Arturo Hernández; H. Clínico U. de Valladolid: Elena Urbaneja Rodríguez; Complejo Asistencial de Segovia: H. General: Rebeca Garrote; H.U. y Politécnico La Fe de Valencia: Rafael Señer; Hospital de Mataró: Joaquim Martorell Aymerich; H.U. Marqués de Valdecilla: José Lorenzo Guerra; H. Sierrallana: José Lorenzo Guerra; H. Gernika-Lumo: Alicia Gutiérrez.
Please cite this article as: Bilbao N, Santiago P, Azkunaga B, Mintegi S. Intoxicaciones agudas no intencionadas asociadas a recipientes no originales. An Pediatr (Barc). 2016;85:102–104.