Spinal muscular atrophy type 1 (SMA-1) is a progressive and fatal disease that leads to ethical problems for Paediatric professionals. Our objective was to determine the ethical options of Paediatric Intensive Care Unit (PICU) paediatricians as regards a child with SMA-1 and respiratory failure.
Material and methodsA cross-sectional descriptive study was conducted using an anonymous questionnaire sent to PICUs in Spain (which can be accessed through the Spanish Society of Paediatric Critical Care web page).
ResultsOf the 124 responses analysed, 70% were from women, 51% younger than 40 years, 54% from a PICU with more than 10 beds, 69% with prior experience in such cases, and 53% with religious beliefs. In the last patient cared for, most paediatricians opted for non-invasive mechanical ventilation (NIV) and limitation of therapeutic effort (LTE) in case of NIV failure. Confronted with a future hypothetical case, half of paediatricians would opt for the same plan (NIV+LTE), and 74% would support the family's decision, even in case of disagreement. Age, prior experience and sex were not related to the preferred options. Paediatricians with religious beliefs were less in favour of initial LTE. Less than two-thirds (63%) scored the quality of life of a child with SMA-1 and invasive mechanical ventilation as very poor.
ConclusionsFaced with child with SMA-1 and respiratory failure, most paediatricians are in favour of initiating NIV and LTE when such support is insufficient, but they would accept the family's decision, even in case of disagreement.
La atrofia muscular espinal tipo 1 (AME-1) es una enfermedad progresiva e incurable que plantea problemas éticos entre los profesionales de Pediatría. Nuestro objetivo ha sido conocer las opciones éticas de los pediatras de UCIP ante los pacientes con AME-1 y fracaso respiratorio.
Material y métodosEstudio descriptivo transversal, mediante una encuesta anónima enviada a las UCIP de España y accesible en la web de la Sociedad Española de Cuidados Intensivos Pediátricos.
ResultadosAnalizamos 124 respuestas (70% mujeres, 51% menores de 40 años, 54% de UCIP con más de 10 camas, 69% con experiencia previa con estos niños y 53% con creencias religiosas). En el último caso atendido, la mayoría de los pediatras optó por la ventilación no invasiva (VNI), realizando después limitación del esfuerzo terapéutico (LET). Ante un hipotético caso futuro, la mitad de los pediatras apoyarían la misma opción (VNI+LET) y el 74% apoyaría la decisión de la familia, aunque no coincidiera con la suya. No se observaron diferencias según la edad, la experiencia previa o el sexo. Los pediatras con creencias religiosas son menos partidarios de la LET inicial. El 63% considera que la calidad de vida de un niño con AME-1 y ventilación invasiva es muy mala.
ConclusionesAnte un niño con AME-1 y fracaso respiratorio, la mayoría de los pediatras de UCIP están a favor de iniciar la VNI y realizar LET cuando dicho soporte no sea suficiente, pero apoyarían la decisión de la familia aunque no estuvieran de acuerdo con ella.
Spinal muscular atrophy type 1 (SMA-1) is an incurable neuromuscular disease with an autosomal recessive pattern of inheritance in which the degeneration of the motor neurons of the spinal cord leads to progressive and irreversible muscular atrophy. Although patients can maintain respiratory function in the early months of life, most die within one year without some type of ventilatory support.1,2
The decision to initiate ventilatory support (noninvasive ventilation [NIV] or invasive ventilation with tracheostomy)3,4 or to withhold it (limitation of treatment, LTE) has significant ethical connotations and usually raises serious concerns both in health care professionals and in the families of patients.5,6 Although in recent years there have been attempts to standardise palliative care for children with SMA-1, a consensus has not been reached on the indication for ventilatory support and, if offered, its timing and modality.1,3,4,7–12
Since the experiences and opinions of paediatricians usually weigh heavily on decision-making processes pertaining to patients with SMA-1, and no studies on the subject have been previously conducted in Spain, we made a survey on the ethical aspects involved in the initial and long-term care of these children.
Materials and methodsWe conducted a cross-sectional descriptive study by means of a questionnaire that could be completed and submitted directly using an online form that was produced with the Google Drive software.
The questionnaire included questions pertaining to three domains:
- 1.
General information: autonomous community of residence, occupation, work setting, number of beds in the unit, sex, age, established restrictions to the admission of SMA-1 patients, previous experience with these patients, and religious beliefs.
- 2.
Experience with the most recently managed case of SMA-1: previous information on the disease, direct care delivery, direct intervention in providing information, disagreements regarding treatment among health professionals or in the family, preferred treatment approach by each professional group and the family, whose opinion weighed most heavily in decision-making.
- 3.
Attitude towards a potential future case: preferred approach, support of the family's decision, patient quality of life, setting where the child should live and die.
An initial version of the questionnaire was validated in a group of 15 paediatricians and nurses employed in a paediatric intensive care unit (PICU) and revised by the authors to improve comprehension of the questions and their order. Since patients with SMA-1 that experience respiratory failure are usually managed in PICUs, the survey was published in the website of the Spanish Society of Paediatric Intensive Care (Sociedad Española de Cuidados Intensivos Pediátricos [SECIP]) and was also sent by electronic mail to Spanish PICUs. Responses to the survey were anonymous, and the survey was made available between December 1, 2014 and March 31, 2015, and initially addressed to paediatricians, medical residents and nurses working in PICUs. To prevent biases in the analysis, we excluded questionnaires completed from outside of Spain, and those submitted by nurses and medical residents due to the low number of responses obtained from these collectives (39 nurses and 15 residents).
We conducted the statistical analysis using the software SPSS version 20 (SPSS, Inc., Chicago, USA).
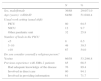
ResultsWe analysed the responses of 124 paediatricians from the 15 autonomous communities of peninsular Spain. The number of responses per autonomous community was greater than 10 for Andalusia, Catalonia, Madrid and Galicia. Table 1 summarises the general data of the survey.
General data for the survey (N=124).
| N | % | |
|---|---|---|
| Sex, male/female | 36/88 | 29.0/71.0 |
| Age (years): <40/≥40 | 64/60 | 51.6/48.4 |
| Usual work setting (usual shift) | ||
| PICU | 80 | 64.5 |
| NICU | 12 | 9.7 |
| Other paediatric unit | 32 | 25.8 |
| Number of beds in the PICU | ||
| <5 | 8 | 6.5 |
| 5–10 | 49 | 39.5 |
| >10 | 67 | 54.0 |
| Do you consider yourself a religious person? | ||
| Yes/no | 66/58 | 53.2/46.8 |
| Previous experience with SMA-1 patients | 85 | 68.5 |
| Had adequate knowledge of the disease | 76 | 89.4 |
| Involved in direct care | 80 | 94.1 |
| Involved in providing information | 61 | 71.7 |
Table 2 shows the responses of the 85 paediatricians that had been involved in the care of children with SMA-1 in the past regarding their experience with the most recent case. Of these paediatricians, 31.4% acknowledged that there were disagreements between parents and paediatricians, and 60.5% reported some type of disagreement in the most recent case (between health professionals/family, paediatricians/nurses or mother/father).
Opinions regarding the most recently managed case of SMA-1, as recalled by surveyed paediatricians (N=85).
| N | % | |
|---|---|---|
| Disagreement between parents and health professionals | 27 | 31.4 |
| Disagreement between paediatricians and nursing staff | 16 | 18.6 |
| Disagreement between the mother and father | 9 | 10.5 |
| Pressure on parents by other members of the family regarding decision-making | 17 | 19.7 |
| Who had the most weight on decision-making? | ||
| The family | 40 | 46.5 |
| The paediatricians in charge of the patient | 38 | 44.2 |
| The Health Care Ethics Committee | 1 | 1.2 |
| Does not know | 6 | 7.0 |
Table 3 shows the treatment options chosen by paediatricians and recalled by paediatricians as having been chosen by the nursing staff and the family in the most recent case. We found statistically significant differences between the opinions of paediatricians and the opinions of nurses and families recalled by paediatricians. The most frequent choice of paediatricians was initiation of NIV followed by LTE if NIV proved ineffective. In contrast, the choices of nurses (as reported by paediatricians) were LTE in one third and NIV+LTE in one third, with the other third remaining undecided. On the other hand, 43% of families (as reported by paediatricians) were in favour of using NIV+LTE, and a significant 31% wished for full life-sustaining support in the long term.
Recollection of the treatment approach preferreda by PICU providers in a past case of SMA-1 (N=85).
| Option | Surveyed paediatricians | Option preferred by nursesa | Option preferred by familya | P |
|---|---|---|---|---|
| Limitation of treatment | 14 (16.5%) | 28 (32.9%) | 11 (13.0%) | 0.003 |
| Initiation of noninvasive ventilation, with limitation of treatment once invasive support is required | 56 (66%) | 28 (32.9%) | 37 (43.5%) | <0.001 |
| Use every possible measure to prolong life, including long-term invasive mechanical ventilation | 8 (9%) | 3 (3.5%) | 27 (31.7%) | <0.001 |
| Present the case to the Health Care Ethics Committee | 3 (3.5%) | 0 | 0 | 0.04 |
| Does not know | 4 (5%) | 26 (30.6%) | 10 (11.8%) | <0.001 |
Results expressed as absolute frequency (percentage).
Table 4 compares the treatment approach taken in a past case with the approach to a potential future case. Half of respondents with previous experience in the management of SMA-1 (49%) would choose the combined, time-limited trial option (NIV+LTE), the approach chosen by 56% of respondents without prior experience. Seventy percent of respondents with experience and eighty-five percent of respondents without experience would support the family's decision in a future case, even if they did not agree with it, while twenty-one percent of respondents with experience and fifteen percent of respondents without experience answered that they would only support the family's decision if directed to do so by the Health Care Ethics Committee.
Treatment option paediatricians would choose in a hypothetical future case of SMA-1.
| Future case | |||
|---|---|---|---|
| Option | Most recent case (N=85) | Paediatricians with experience (N=85) | Paediatricians without experience (N=39) |
| Limitation of treatment | 14 (16.5) | 15 (17.7) | 3 (7.7) |
| Initiation of noninvasive ventilation, with limitation of treatment once invasive support is required | 56 (65.9) | 42 (49.4) | 22 (56.4) |
| Long-term invasive mechanical ventilation (initially delivered by endotracheal tube and eventually by tracheostomy) | 8 (9.4) | 3 (3.5) | 0 |
| Long-term noninvasive ventilation | – | 8 (9.4) | 4 (10.2) |
| Undecided | 4 (4.7) | 17 (20.0) | 10 (25.7) |
| Consult HCEC | 3 (3.5) | – | – |
| Would you support the family's decision even if you did not agree with it? | |||
| Yes | 59 (69.4) | 33 (84.6) | |
| No | 7 (8.2) | 0 | |
| Only if dictated by HCEC | 19 (22.4) | 6 (15.4) | |
Results expressed as absolute frequency (percentage).
HCEC, Health Care Ethics Committee.
Table 5 shows the results of the choices that would be made in a future case by sex, age, religious beliefs and previous experience of the respondents. The only statistically significant difference that we found based on sex was a lower proportion of undecided in male respondents. When it came to age, respondents aged less than 40 years leaned more towards the long-term use of NIV than respondents of older age. Paediatricians that identified as religious were more likely to choose NIV+LTE and less likely to choose LTE from the outset than their non-religious colleagues.
Preferred treatment option for future cases by sex, age, religious beliefs and previous experience in the management of these patients.
| Sex | Age | Religious | ||||
|---|---|---|---|---|---|---|
| Option | F | M | <40 years | >40 years | Yes | No |
| N | 88 | 36 | 64 | 60 | 66 | 58 |
| Limitation of treatment | 10 (11) | 8 (22) | 9 (14) | 9 (15) | 6 (9)* | 18 (21) |
| Time-limited NIV and LTE when no longer efficient | 46 (52) | 18 (50) | 32 (50) | 32 (53) | 38 (58)* | 64 (45) |
| Long-term NIV | 7 (8) | 5 (14) | 8 (12.5) | 4 (7)* | 2 (3)* | 12 (17) |
| Long-term IMV | 3 (3) | 0 | 1 (1.6) | 2 (3.3)* | 2 (3) | 1 (1.6)* |
| Undecided | 22 (25) | 5 (14)* | 14 (22) | 13 (22) | 18 (27) | 9 (15)* |
Results expressed as absolute frequency (percentage over the total of each group).
F, female; IMV, invasive mechanical ventilation; LTE, limitation of treatment; M, male; NIV, noninvasive ventilation.
Salient findings are presented in boldface.
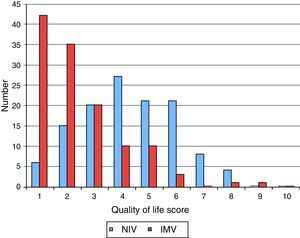
Fig. 1 shows the results of the estimation by respondents of the quality of life of a child with SMA-1 on long-term ventilatory support, be it NIV or invasive mechanical ventilation (IMV), assessed on a scale from 1 (very poor) to 10 (very good). When it came to NIV, 56% assigned quality of life a score of less than 5 points, while for IMV, 63% assigned a score below 3.
Last of all, 96% of paediatricians considered that children with SMA-1 that are in stable condition should stay at family home and not at the hospital. We did not find statistically significant differences based on the autonomous community where paediatricians resided.
DiscussionSpinal muscular atrophy type 1, also known as Werdnig–Hoffman disease, is characterised by the degeneration of motor neurons in the spinal cord that results in muscular atrophy and leads to neuromuscular respiratory failure within a few months, with no functional impairment in the brain or other organs.7 When these patients develop respiratory failure, health care professionals and families face a situation in which decision-making has a significant ethical component. Although the incidence of SMA-1 is low (approximately 1/10,000 births),13 most paediatricians that manage critically ill infants or children have or will come across some of these patients and their families in the course of their careers, so they should be prepared to provide the best possible care, not only technically, but also ethically.
At present, from a technical standpoint, it is possible to support or substitute respiratory function in these children in the long term by means of mechanical devices, both noninvasive (with a variety of available interfaces) and invasive (by means of tracheostomy).3,14 However, it is not clear whether such support is adequate or, conversely, the most appropriate approach is initiating a LTE process, which could be adopted from the outset or once NIV becomes ineffective.3
Decision-making processes in patients with SMA-1 are influenced by multiple aspects (cultural, moral, social, economic and religious, among others) that may give rise to ethical dilemmas in care delivery and hinder the development of treatment guidelines with widespread agreement. For instance, a committee of experts from the United States attempted to standardise the management of these children but failed to reach a consensus regarding respiratory support,1 and in 2010 a consensus group in the United Kingdom recommended against invasive ventilation, proposing NIV as a third approach.4 Several surveys of health care professionals from the United States, the Commonwealth and Japan have been published recently,7–10 demonstrating the great variability that exists in the attitudes towards this issue based on culture and geographical area. For all of the above, and considering the absence of similar studies in Spain, we thought it was important to explore the attitudes of Spanish paediatricians that manage or may eventually manage children with SMA-1.
Our findings suggest that most children with SMA-1 are admitted to the PICU, at least once they develop respiratory failure. However, there are some units that restrict the admission of these patients, possibly because they are not considered eligible for intensive care, but rather for palliative care, which can be delivered in other units of the hospital. In contrast, only 48% of patients with SMA-1 in Australia8 were admitted to a PICU, a percentage that declined to 25% once the diagnosis was confirmed by molecular testing.
Shared decision-making by the health care team and the family is the model most widely accepted as ethically appropriate to set up a treatment plan when there are different treatment options, each of them with its own set of risks and benefits.15 In the case of SMA-1, health professionals must be prepared to work in situations in which the family chooses options that do not match those preferred by the provider. Although this applies to all paediatricians, this need for “preparation” is particularly relevant in paediatricians that have never encountered a patient with this condition (based on our survey, nearly 1 in 3), since based on the recollections of colleagues that have managed cases in the past, disagreements are frequent, especially between parents and clinicians (nearly in one third of cases).
Although they were aware that disagreements often arise between health professionals and parents, paediatricians and nurses, or mothers and fathers, very few paediatricians (1% of respondents) brought cases to the Health Care Ethics Committee to attempt to resolve these conflicts, which reveals a certain lack of understanding by both health professionals and patients of the functions and benefits of ethics committees.
The fact that paediatricians acknowledged that they had the most weight in the decision-making process in 44% of the cases reveals the persistence of a somewhat paternalistic attitude in the clinical relationship. On the other hand, when paediatricians were asked whether they would support the choices of the family even if they did not agree with their own opinion, nearly three out of four answered in the affirmative, which suggests a growing acknowledgement of the autonomy of the patient, in agreement with the principles of health care ethics and with current legislation.16
When it came to the preferred treatment approach in past cases of SMA-1, paediatricians reported that nurses most frequently preferred LTE from the beginning of respiratory failure, while paediatricians most frequently preferred to use time-limited trials of NIV followed by LTE once the patient required invasive support.17 This option was also most frequently preferred by families, although a substantial 31% of families wished to use every possible option to prolong the life of the child, even if this involved long-term mechanical ventilation via tracheostomy.
When we asked about treatment options for a hypothetical future case, we included long-term NIV because in recent years, the NIV technology has advanced greatly with improvement in devices, interfaces18 and training of health care professionals, leading to its increased use both in PICU and home settings.
We asked paediatricians about their preferences in a hypothetical future case, and compared the responses of paediatricians with previous experience (PEs) with those of paediatricians with no experience (PNEs). The combined option (initial NIV followed by LTE) continues to be preferred option of paediatricians (49% of PEs and 56% of PNEs), while we found differences regarding LTE, which would be the choice of 18% PEs compared to only 8% of PNEs, although nearly 20% of PEs and 26% of PNEs stated that they are not sure which option they would prefer, which is consistent with the difficulties expressed in consensus documents published in other countries in regard to choosing the best option in these cases, and the course of action that would be most widely accepted in the present.1,3,4
We collected data to assess the potential influence of variables such as sex, age, religious beliefs or previous experience in the choice between different options for the management of patients with SMA-1. The most salient findings of our analysis were that paediatricians with religious beliefs were less inclined to adopt LTE as the initial approach, and that paediatricians aged less than 40 years were more likely to promote the long-term use of NIV. Although we do not know the reasons underlying these differences, it is possible that individuals with religious beliefs find the use of LTE as the initial approach less acceptable from a moral standpoint, although they would find it acceptable once the condition of the patient has deteriorated to the point of requiring invasive ventilation. As for the preference of young paediatricians for long-term NIV, we believe that it may be explained by a more extensive knowledge of this technique and a greater confidence in its possibilities, as the use of NIV has grown exponentially in recent years.19
An essential factor to consider in making decisions regarding LTE is the present and future quality of life of the patient, taking into account that its assessment is always subjective, that the assessment made by the patient (if it can be known) should prevail over all others, and that the studies conducted to date show that health care professionals generally tend to make more negative estimates of quality of life than patients and their families.18,20 At any rate, there seems to be widespread agreement that there are circumstances in which quality of life is “too low”, so that LTE would be an appropriate approach.3,4,18 On this point, our survey showed that most paediatricians estimated that the quality of life of a child with SMA-1 on mechanical ventilation is very low (scored at less than 3 on a 10-point scale), while the quality of life could be acceptable with the use of NIV (approximately half of respondents gave it a score slightly above 5 in the same scale). Although we do not have these data, it would be interesting to know how parents of patients with SMA-1 would score it, or even the score that would be given by patients that survived to adolescence or adulthood with the help of invasive mechanical ventilation.
One aspect that is under debate is the degree of involvement of nursing staff in the process of making decisions that pose ethical challenges.21 While there are European guidelines that recommend involving nurses in the decision-making process,22 there is great variability in their actual involvement, with reported figures as varied as 96% in the United Kingdom, 52% in a European study, and 16% in a Canadian study.15 In our study, while 81% of paediatricians reported that there were no overt disagreements with the nursing staff, we could not ascertain whether nurses were actually consulted. There are no data on the degree of involvement of nurses in this type of processes in Spain, but we believe that efforts are increasingly made in PICU settings to reach collective agreement in decision-making, and that the opinions of nurses are increasingly being taken into account.
Our study has the intrinsic limitations of surveys, which can be biased due to various factors (the sample obtained, the means by which it is conducted, the type of questions, the characteristics of the individuals that choose to complete it, etc.). In this particular instance, we estimate that the number of responses we obtained corresponded to approximately 50% of the population under study. This fact must be taken into account in the interpretation of results. On the other hand, since we only analysed the opinions given by paediatricians, we may have obtained a biased representation of what actually happened in past cases as regards both their own opinions and their recall of the opinions of the family and the nursing staff. Thus, it would be interesting to conduct a similar survey in nurses working in paediatric and neonatal intensive care units and, ideally, to explore the experiences, attitudes and choices of the parents of children with SMA-1, including parents of children that died following LTE or due to complications, and of children that survived with ventilatory support. Since SMA-1 is a rare disease, recruiting a significant number of parents would require a multicentre, prospective and prolonged study with a specific methodology for data collection and analysis.
To conclude, when confronted with a child with SMA-1 and respiratory failure, most paediatricians in Spanish PICUs would encourage initiation of NIV and LTE if this type of support was not sufficient, and would support the family's decision even if they disagreed with it.
FundingThis study has not received funding from any public or private institutions.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Agra Tuñas MC, Hernández Rastrollo R, Hernández González A, Ramil Fraga C, Cambra Lasaosa FJ, Quintero Otero S, et al. Actitudes éticas de los pediatras de Cuidados Intensivos ante pacientes con atrofia muscular espinal tipo 1. An Pediatr (Barc). 2017;86:151–157.