To determine the frequency and magnitude of neonatal hypophosphataemia (<4mg/dL) in a neonatal Intensive Care Unit and to describe risk groups.
Patients and methodsRetrospective study of hospitalised newborns over a 44 month period (phase 1). Retrospective study of <1500g/<32 weeks of gestation newborns over a 6 month period (phase 2). Prospective study of <1500g or 1550–2000g, and intrauterine growth restriction (IUGR) newborns. Measurements were made on the 1st, 3rd, 7th, and 14th days of life (phase 3).
ResultsPhase 1: 34 (2.4%) of 1,394 patients had a diagnosis of hypophosphataemia, 76% of them ≤32 weeks of gestation and <1500g, and 24% >32 weeks with weightmg/dL in 5 (6.8%). Eight (75%) of those with hypophosphataemia had IUGR, and 4 (25%) weighed <1000g. Five cases had associated hypokalaemia, and three hypercalcaemia. Phase 3: 9 (45%) of 20 patients had hypophosphataemia, all of them <1000g or <1200g and weight percentile <10. Thirty-three percent of samples on days 1, 3, and 7 showed hypophosphataemia, four of them <2mg/dL. There was mild hypokalaemia in 5 (55%), and mild hypercalcaemia in 2 (22%) cases. Hypophosphataemia was associated with lower enteral nutrition and higher parenteral amino acid intake in the early days of life.
ConclusionsHypophosphataemia is common, and can be severe, in the first week of life in premature infants <1000g, and newborns <1200g with foetal malnutrition and receiving amino acids in early parenteral nutrition.
Conocer la frecuencia y la magnitud de la hipofosforemia neonatal (<4mg/dl) en una UCIN y definir los grupos de riesgo.
Pacientes y métodosEstudio retrospectivo en neonatos hospitalizados, en periodo de 44 meses (fase 1). Estudio retrospectivo en <1.500g/<32 semanas de gestación en período posterior de 6 meses (fase 2). Estudio prospectivo en <1.500g o CIR con peso 1.500-2.000g. Determinaciones en días 1, 3, 7 y 14 de vida (fase 3).
ResultadosFase 1: 34 de 1.394 pacientes (2,4%) fueron diagnosticados de hipofosforemia, 76% de ellos ≤32 semanas de gestación y <1.500g, y 24% >32 semanas con pesomg/dl. De ellos 8 fueron CIR y 4 <1.000g. Cinco pacientes asociaron hipopotasemia y 3 hipercalcemia. Fase 3: 9 de 20 pacientes (45%) presentaron hipofosforemia, todos <1.000g o con peso al nacer <1.200g y percentil <10. El 33% de las muestras de los días 1, 3 y 7 mostraron hipofosforemia, <2mg/dl en 4 muestras. Asociaron hipopotasemia leve 5 casos (55%) e hipercalcemia leve 2 (22%). La hipofosforemia se asoció a menor nutrición enteral y más aporte parenteral de aminoácidos en los primeros días.
ConclusionesLa hipofosforemia es frecuente y puede ser crítica en la primera semana en prematuros <1.000g y en los nacidos con desnutrición fetal y peso <1.200g que reciben aminoácidos en la nutrición parenteral precoz.
Hypophosphataemia is an electrolyte disturbance that has been overlooked by neonatology reference books and protocols for the management of ill newborns until very recently.1,2 Before year 2000, reports of hypophosphataemia were limited to cases associated with the bioavailability of the inorganic phosphates formerly used in parenteral nutrition,3 and it was not until 2006 that cases of hypophosphataemia in newborns potentially associated with refeeding syndrome were first reported.4
In our unit, we started administering amino acids (Primene 10%®) parenterally to preterm newborns with birth weights of less than 1500g from the first day of life in 2001. Around the middle of that decade, hypophosphataemia started to be detected in newborns as a chance finding in blood tests performed for unrelated reasons. In 2010, due to the frequency and severity of some of the episodes of hypophosphataemia, our hospital developed a protocol for screening at-risk newborns and for the prevention and management of hypophosphataemia. The lack of relevant research in neonatology posed a challenge in the development of this initial protocol, for which we resorted to the extrapolation of data on treatment of adults with refeeding syndrome.5–8 The first reports of hypophosphataemia in very low birth weight preterm newborns were published in 2012, and different authors started to propose refeeding syndrome as a potential aetiology.9–11 Subsequent publications have described its pathophysiology, an association with a high amino acid intake and a potential increase in the risk of sepsis that would compound the direct and possibly fatal effects of severe hypophosphataemia.12–14
The objectives of our study were to define the risk groups for hypophosphataemia in our hospital and to determine the frequency, severity and temporal distribution of early episodes of hypophosphataemia in the first 2 weeks of life.
Materials and methodsDesignWe conducted a single-centre descriptive study in a IIIC level unit, organised in three phases:
- -
Phase 1: retrospective observational study between January 2010 and September 2013, with collection of data on discharge diagnoses of hypophosphataemia among all the newborns admitted to neonatal intensive care. Other variables under study were duration of gestation, birth weight and birth weight percentile.
- -
Phase 2: retrospective observational study between July and December 2014 (6 months) in newborns with birth weights of less than 1500g or born before 32 weeks’ gestation. Variables under study: birth weight, duration of gestation, prenatal diagnosis of intrauterine growth restriction (IUGR) with signs of placental insufficiency, diagnosis of hypophosphataemia, detection of low phosphate levels, diagnosis of hypokalaemia (<4mEq/L) or hypercalcaemia (≥11mg/dL) in association with hypophosphataemia.
- -
Phase 3: prospective cohort study between March and November 2014 of two populations: newborns delivered in our hospital with a birth weight of less than 1500g, and newborns delivered in our hospital with a diagnosis of intrauterine growth restriction and a birth weight of 1500–2000g. In this phase, we excluded patients with major congenital anomalies or perinatal asphyxia with moderate or severe encephalopathy, and those whose parents refused or withdrew consent for participation.
- -
Maternal and gestational variables: placental insufficiency or preeclampsia during gestation, maternal disease, maternal pharmacological treatment, multiple gestation, prenatal administration of corticosteroids and prenatal administration of magnesium sulfate.
- -
Birth variables: duration of gestation, birth weight and birth weight z-score, sex, resuscitation with positive-pressure ventilation and Apgar score at 5min.
- -
Peripheral or arterial blood chemistry values at days 1, 3, 7 and 14 post birth: phosphate (hypophosphataemia if level <4mg/dL; moderate, 3–3.9mg/dL; severe, 2–2.9mg/dL; critical, <2mg/dL); calcium (hypercalcaemia if level >11mg/dL); potassium (normal range, 4–5mEq/L); sodium (normal range, 135–145mEq/L); chloride (normal range, 90–110mEq/L); alkaline phosphatase (normal range, 100–400IU/L); creatinine (normal range <0.95mg/dL).
- -
Actual administration of nutritional supplements (not calculated based on prescription): enteral nutrition from day 1 to 14 post birth in mL/kg/day. Parenteral nutrition from day 1 to 14 post birth (amino acids, glucose and lipids in g/kg/day; phosphorus in mmol/kg/day; calcium, potassium and sodium in mEq/kg/day).
- -
Morbidity at discharge: treated patent ductus arteriosus, days of invasive mechanical ventilation, retinopathy of prematurity, bronchopulmonary dysplasia and, where present, grade of dysplasia, enterocolitis, late-onset sepsis confirmed by blood culture, clinical late-onset sepsis, periventricular leukomalacia, haemorrhagic stroke, intraventricular haemorrhage.
Minimal enteral nutrition was initiated in the first 24h post birth with maternal colostrum or pasteurised donor human milk unless medically contraindicated. Artificial formula was used if human milk was not available in newborns delivered at 32 weeks’ gestation or later with birth weights of more than 1500g. Maternal and pasteurised donor milk were supplemented with FM85® once enteral feedings had advanced to 100mL/kg/day. Parenteral nutrition, standard or individualised, was initiated in the first 24h of life (as it can be administered via a peripheral vein and contributes 2g/kg/day of amino acids). Intravenous administration of sodium, potassium and phosphorus (as glycerophosphate) started from 48h post birth. Supplementation with calcium started from birth. The recommended phosphorus intake (mmol/kg/day) was 0.5–0.8 in the first week and 0.5–1.5 starting from 7 days post birth. The recommended calcium intake was 1.5–2mEq/kg/day the first week and 2–3.5mEq/kg/day thereafter. The Ca:P molar ratio was approximately 1.6.
Data analysisWe have described discrete variables as proportions and continuous variables as the mean or median with the corresponding standard deviation or range. We compared discrete variables by means of the chi square test. We used nonparametric tests to compare continuous variables between groups. We compared repeated measures using the repeated measures GLM procedure in SPSS. All tests were two-tailed with statistical significance defined as a P-value of less than 0.05.
Ethics and confidentialityThe study was approved by the clinical research ethics board of our hospital (reference 13/343). We obtained the written informed consent of the parents of all newborns who participated in the prospective study (phase 3). We retrieved the data for phases 1 and 2 from the electronic health records database of the department of neonatology, removing personally identifiable information.
ResultsPhase 1: of a total of 1,394 newborns admitted to the NICU in this period, 34 (2.4%) had received a diagnosis of hypophosphataemia during their stay. Of these, 26 (76%) had been born at 32 weeks’ gestation or earlier, and 26 also weighed less than 1500g at birth. All the rest had birth weights below the 10th percentile and had been born between 33 and 40 weeks’ gestation, and the highest birth weight among the patients with a diagnosis of hypophosphataemia was 2300g.
Phase 2: of a total of 73 preterm newborns with birth weights of less than 1500g or born before 32 weeks’ gestation, 12 (16.4%) developed hypophosphataemia, which was severe in 7 (9.6%) and critical in 5 (6.8%). All cases of critical hypophosphataemia (serum phosphate <2mg/dL) occurred in the first 3 days post birth. Nine cases (75%) occurred in patients with a history of intrauterine growth restriction with abnormalities in blood flow distribution. The other three corresponded to patients born with weights of less than 1000g. Hypophosphataemia was associated with hypokalaemia in 5 cases (42%) and hypercalcaemia in 3 (25%).
Phase 3: a total of 37 patients met the inclusion criteria, and we received parental consent for the participation for 20, of who 16 had birth weights of less than 1500g. Two patients died during their stay due to morbidity associated with prematurity. Table 1 summarises the characteristics of the patients in the cohort.
Characteristics of the cohort studied in phase 3.
| Description | Details | |
|---|---|---|
| Prenatal variables | ||
| Multiple pregnancy | 6 (30%) | 5 twin and 1 triplet |
| Maternal disease | 70% | Other: coeliac disease and psoriatic arthritis |
| Preeclampsia | 5 (25%) | |
| PROM/chorioamnionitis | 6 (30%) | |
| Gestational diabetes | 1 (5%) | |
| Other | 2 (10%) | |
| Maternal pharmacological treatment during gestation | 9 (45%) | Labetalol, furosemide, nifedipine. Anti-D immunoglobulin, progesterone, atosiban, ampicillin, erythromycin, ampicillin o amoxicillin, prednisone, bronchodilators |
| Prenatal corticosteroids | 18 (90%) | 1 dose: 4; 2 doses: 10; 3 doses: 4 |
| Magnesium sulphatea | 4 (25%) | |
| Male | 13 (65%) | |
| Newborn variables | ||
| Gestational age (median) | 30 weeks | Range, 24 to 36 |
| Mean birth weight (g) | 1129.5 (SD, 431.25) | Range, 510 to 1890 |
| Mean birth weight z-score | −1.19 (SD, 1.2) | Range, −3.8 to 1.04 |
| Resuscitation with ventilationb | 14 (70%) | |
| 5min Apgar <7 | 4 (20%) | |
| Treated PDA | 0 | |
| Invasive mechanical ventilation | 4 (25%) | 1 to 8 days |
| Bronchopulmonary dysplasia | 1 (5%) | Severe |
| Necrotising enterocolitis | 1 (5%) | |
| Nosocomial infection | 3 (15%) | Sepsis |
| Periventricular leukomalacia | 3 (15%) | Grades 1, 2 and 4 |
| Intraventricular haemorrhage | 1 (5%) | Grade 2 |
| Retinopathy of prematurity | 0 | |
| Exitus | 2 (10%) | |
IUGR, intrauterine growth restriction; PDA, patent ductus arteriosus; PROM, premature rupture of membranes; SD, standard deviation.
Of all participants, 45% had at least one episode of hypophosphataemia (9 out of 20). Table 2 presents a description of these 9 patients. Severe or critical hypophosphataemia occurred in 5 of the patients (25%), adding up to 8 episodes. Table 3 shows the temporal distribution of the episodes of hypophosphataemia.
Description of hypophosphataemia cases and associated abnormalities in serum calcium and potassium levels.
| Weeks of gestation | Birth weight (g) | Birth weight z-score | Episodes of hypophosphataemia (day post birth) | Abnormal potassium levels (mEq/L) | Abnormal calcium levels (mg/dL) | ||
|---|---|---|---|---|---|---|---|
| Moderate | Severe | Critical | |||||
| 26 | 510 | −2.6 | 0 | 1 (3) | 1 (7) | No | No |
| 28 | 520 | −2.7 | 1 (3) | 1 (1) | 0 | HypoK (3.9) | No |
| 32 | 580 | −3.8 | 2 (3 and 7) | 0 | 1 (1) | No | HyperCa (11.6) |
| 32 | 1140 | −1.9 | 1 (7) | 0 | 2 (1 and 3) | No | No |
| 32 | 1160 | −2.2 | 1 (7) | 2 (1 and 3) | 0 | HypoK (3.7) | No |
| 24 | 600 | −0.5 | 1 (1) | 0 | 0 | HypoK (3.7) | HypoCa (5.7) |
| 25 | 720 | −0.5 | 1 (1) | 0 | 0 | HypoK (3.8) | HypoCa (5.8) |
| 30 | 1060 | −1.4 | 2 (3 and 7) | 0 | 0 | None | No |
| 28 | 790 | −1.3 | 1 (7) | 0 | 0 | HypoK (3.8) | HyperCa (11.5) |
HyperCa: hypercalcaemia; HypoCa: hypocalcaemia; HypoK: hypokalaemia.
Frequency of moderate, severe and critical hypophosphataemia in tests performed at days 1, 3, 7 and 14 post birth.
| Days post birth (measurement) | Serum phosphate 3–3.9mg/dL | Serum phosphate 2–2.9mg/dL | Serum phosphate <2mg/dL | Total (% blood samples) |
|---|---|---|---|---|
| 1 (n=17) | 2 | 2 | 2 | 6 (35%) |
| 3 (n=18) | 3 | 2 | 1 | 6 (33%) |
| 7 (n=17) | 5 | 0 | 1 | 6 (35%) |
| 14 (n=15) | 0 | 0 | 0 | 0 |
| Total (n=67) | 10 | 4 | 4 | 18 (27%) |
Of all patients with hypophosphataemia, 55% also had mild hypokalaemia, and 44% changes in serum calcium levels (half of them significant hypocalcaemia and the other half mild hypercalcaemia). Table 4 presents the results of the remaining serum measurements. We found statistically significant increasing trends in the levels of calcium, phosphate and alkaline phosphatase and decreasing trends in the levels of sodium, chloride and creatinine with the passage of time. Twenty percent of the patients developed mild hypernatraemia, with a peak sodium level of 155mEq/L.
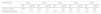
Results of measurements of serum sodium, potassium, phosphate, calcium, creatinine and alkaline phosphatase levels, expressed as the mean with the standard deviation in parentheses. Analysis by multivariate repeated measures general linear model.
| Day 1 | Day 3 | Day 7 | Day 14 | P | |
|---|---|---|---|---|---|
| Sodium (mEq/L) | 140.85 (6.6) | 143 (3.9) | 139.4 (6.1) | 137.2 (3.7) | 0.028 |
| Potassium (mEq/L) | 4.73 (0.80) | 4.76 (0.55) | 5.11 (0.78) | 5.05 (0.33) | 0.1 |
| Chloride (mEq/L) | 108.6 (5.5) | 112.8 (6.5) | 106.2 (5.1) | 105.1 (3.3) | 0.041 |
| Calcium (mg/dL) | 8.55 (1.76) | 9.45 (1.39) | 9.51 (1.97) | 9.88 (1.51) | 0.013 |
| Phosphorus (mg/dL) | 4.43 (1.5) | 4.49 (1.36) | 4.48 (1.32) | 5.85 (0.87) | 0.024 |
| Creatinine (mg/dL) | 0.71 (0.18) | 0.48 (0.24) | 0.52 (0.16) | 0.38 (0.21) | 0.059 |
| Alkaline phosphatase (IU/L) | 155.8 (42.5) | 225.5 (76) | 311.7 (141) | 302.4 (68.5) | 0.014 |
The birth weight and the z-score for birth weight were significantly lower in patients with hypophosphataemia (Mann–Whitney U test, P=0.001 and 0.014, respectively), but there was no difference in gestational age (P=0.18).
We did not find differences between patients with hypophosphataemia and patients without based on sex, type of life support, history of maternal preeclampsia or prenatal administration of magnesium sulphate.
Patients with hypophosphataemia received smaller enteral nutrition volumes in the first 2 weeks and therefore higher doses of parenteral nutrition (Table 5), with higher intravenous doses of amino acids, glucose and lipids. However, we did not find differences in the intravenous doses of calcium and phosphorus in the first 5 days (Table 6). Starting at 6 days, the size of the differences rendered the analysis inconsequential. None of the patients received insulin.
Mean doses of micronutrients delivered enterally or parenterally (IV) in mL/kg/day. Comparison of patients who had hypophosphataemia (HypoP) and patients who did not (NP).
| Dose/kg/day | Days 1 and 2 | Days 3–6 | Days 7–14 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| NP | HypoP | P | NP | HypoP | P | NP | HypoP | P | |
| Enteral nutrition (mL) | 15.3 | 8.7 | 0.003 | 62.6 | 11.9 | 0.001 | 140 | 49.2 | 0.004 |
| IV AA (g) | 1.29 | 2.36 | 0.013 | 1.45 | 2.52 | 0.014 | 0.15 | 1.89 | 0.001 |
| IV glucose (g) | 5.28 | 7.44 | 0.08 | 3.94 | 8.99 | 0.012 | 0.18 | 5.08 | 0.04 |
| IV lipids (g) | 0.74 | 0.89 | ns | 0.93 | 1.89 | 0.016 | 0.04 | 1.42 | 0.04 |
ns: not significant.
Mean intravenous dose of calcium and phosphorus in the first week of life. Comparison of patients that developed hypophosphataemia (hypoP) versus patients that did not (NP). The differences were not statistically significant (Mann–Whitney test).
| Dose/kg/day | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| NP | HypoP | NP | HypoP | NP | HypoP | NP | HypoP | NP | HypoP | |
| Calcium (mEq) | 0.88 | 0.91 | 0.97 | 1.16 | 1 | 1.06 | 0.94 | 0.9 | 0.67 | 0.84 |
| Phosphorus (mmol) | 0 | 0.12 | 0.27 | 0.47 | 0.49 | 0.59 | 0.48 | 0.61 | 0.42 | 0.70 |
Recent studies have consistently identified foetal malnutrition, birth weight of less than 1000g and high intake of amino acids early after birth as risk factors for the development of hypophosphataemia in the first week of life.10,12,14 Our study corroborated these associations and found a high incidence of hypophosphataemia in the prospective phase, with low phosphate levels detected in approximately one third of the blood tests performed at days 1, 3 and 7 post birth, of which 22% were in the range of critical hypophosphataemia. The incidence was highest in newborns with birth weights of less than 1000g or with birth weights of less than 1200 and a history of foetal malnutrition. Data from adult studies describe the development of symptoms when levels drop below 1.5mg/dL, or before if the decline is rapid.8 In newborns, serum phosphate levels are higher compared to adults, and they can drop very quickly after cord clamping unless phosphorus is administered with enteral or parenteral nutrition. We observed some cases in extremely small newborns with serum phosphate levels of 0.5mg/dL that required doses of up to 3.5mmol/kg/day to correct the hypophosphataemia, as reported by other authors.9 These patients are at immediate risk of losing their lives, but other patients with hypophosphataemia are also at risk of suffering the clinical repercussions described in adults and critically ill children15 as well as newborns.12,16
This surge in hypophosphataemia seems to have 2 well-described causes. On the one hand, there is refeeding syndrome, as observed in adult critical patients in the first 3 days of refeeding, which in newborns would result from intrauterine malnutrition14 in the context of rapid foetal growth combined with aggressive parenteral nutrition after birth, and especially with the administration of high doses of amino acids.17,18 On the other hand, there is the practice of withholding administration of intravenous sodium or potassium in the first 48h of life in very low birth weight preterm newborns, which limits the intake of phosphate salts in the first 2 days and exacerbates the hypophosphataemia. There is also the calcium-to-phosphorus molar ratio of 1:1.6 that has been used this far, which is probably inadequate. Retaining 1g of amino acids requires 10mg (0.33mmol) of phosphorus, so in the situation that we have described, a molar ratio of 1.2:1 to 1:1 seems more appropriate from a physiological perspective. Needless to say, once hypophosphataemia develops, the necessary replacement of phosphorus will invert this ratio.
There were several limitations to our study, including it having been conducted in a single centre, the small size of the prospective sample, the high proportion of parents that refused to participate (probably due to the greater number of blood samples drawn in study participants compared to standard care) and the retrospective design of phases 1 and 2. It is very likely that hypophosphataemia was underdiagnosed in these two retrospective phases, and it was not possible to establish when hypophosphataemia had started in the patients included in phase 1. Although it is likely that the pattern was similar to the one observed in phase 3, we found cases of late-onset hypophosphataemia associated with sepsis or refeeding after enterocolitis. Furthermore, there were conspicuously high proportions of maternal disease during gestation and of twin pregnancies in the phase 3 cohort. Lastly, the morbidity in this small group cannot be deemed representative of overall morbidity in the population of infants born with weights of less than 1500g or before 32 weeks’ gestation in our unit. Due to all of the above, it is difficult to infer the clinical repercussions of hypophosphataemia in this small sample of newborns.
Despite these limitations, our results warranted changes to our practices regarding parenteral nutrition, electrolyte supplementation and performance of blood chemistry tests in our patients. First of all, we established routine monitoring of serum phosphate levels in the first week of life in this at-risk group (birth weight <1000g and newborns with a history of IUGR with a birth weight z-score <−2)19 and in critical patients undergoing refeeding after the first week of life. It was also decided that initiation of sodium and phosphorus supplementation would not be delayed past 24h post birth. In cases where an intake of 2–3g of amino acids is desirable since birth, supplementation with phosphorus should probably also start in the first day of life with doses of 0.5–1mmol/kg/day. Although further research is required to evaluate the safety and efficacy of these changes, there is also evidence that a moderate intake of sodium is well tolerated since birth18 and is not associated with an increase in the incidence of hypernatraemia as long as electrolyte and fluid balances are properly controlled.
To conclude, this small study demonstrates that hypophosphataemia frequently develops in newborns weighing less than 1000 or 1200g and with a history of foetal malnutrition receiving amino acid supplementation in parenteral nutrition from the first day of life. Hypophosphataemia may reach critical levels, so monitoring of phosphate levels should probably become routine practice in this group of patients, with consideration of electrolyte supplementation in the first 2 days of life.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Bustos Lozano G, Hidalgo Romero Á, Melgar Bonis A, Ureta Velasco N, Orbea Gallardo C, Pallás Alonso C. Hipofosforemia precoz en recién nacidos de riesgo. Frecuencia y magnitud. An Pediatr (Barc). 2018;88:216–222.
Previous presentation: This study has not been presented in any congresses. Álvaro Hidalgo Romero presented part of the results as part of his thesis for the Bachelor's degree in Medicine in June 2014, titled Frecuencia del síndrome de realimentación en recién nacidos de riesgo.
Partial preliminary results presented in a clinical session held in Hospital 12 de Octubre in 2015 and in the presentation titled Los nuevos trastornos iónicos en el prematuro extremo included in the course Cuidado diferencial del niño prematuro extremo en sus primeros días de vida offered at Hospital 12 de Octubre on May 27, 2016.