Cat-scratch disease (CSD) is a benign and self-limiting disease caused by Bartonella henselae. It typically presents with regional lymphadenopathy, but it can have a systemic presentation in 5–15% of cases1 and is part of the differential diagnosis of fever of unknown origin (FUO). We present 2 patients with disseminated CSD managed at Nationwide Children's Hospital of Columbus, Ohio (United States).
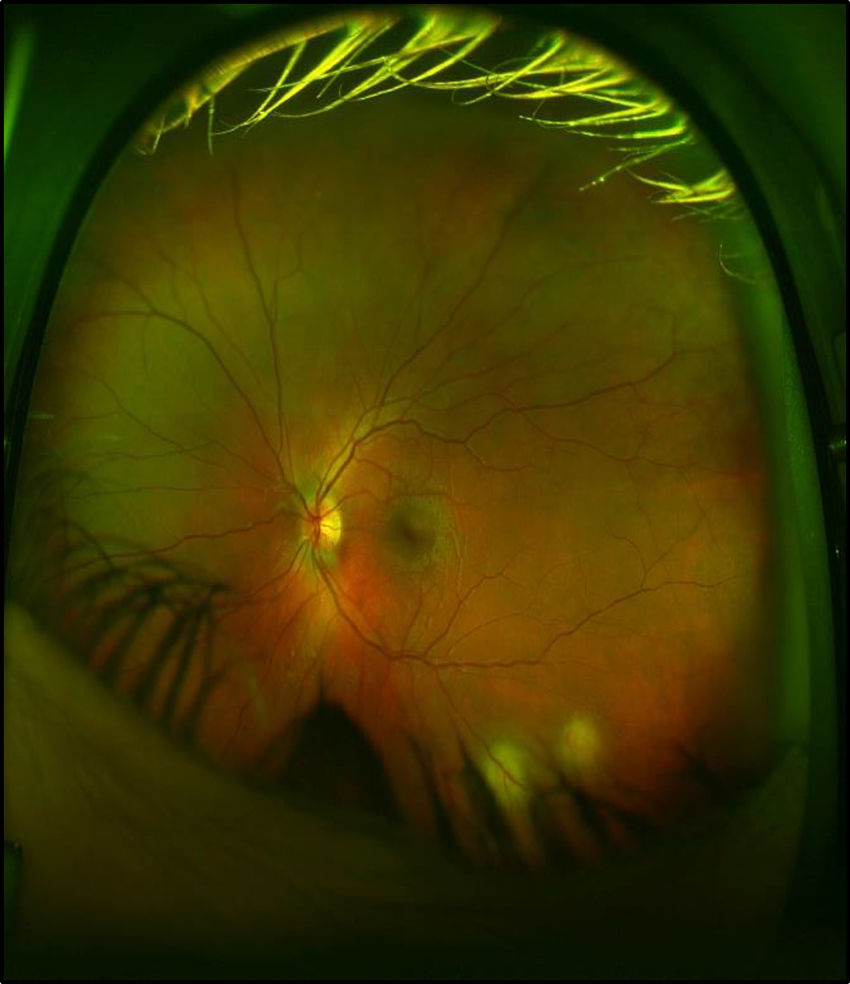
The first patient was a male of 14 years of age , otherwise healthy, presenting with fever of 16 days’ duration, asthenia, headache and weight loss. He reported pain in the right hip , shoulder and abdomen in the past week. The patient had contact with dogs and turtles. The main finding on the physical examination was pain on passive movement of the right shoulder. An abdominal ultrasound revealed multiple hypoechoic foci in the spleen, a finding that led to suspect CSD and referral for an ophthalmologic evaluation was placed that led to the detection of granulomas in the left retina and optic disk (Fig. 1). A shoulder MRI scan detected multifocal osteomyelitis involving the right scapula and the proximal region of the humerus as well as myositis. At this point, the patient did report contact with cats.
As part of the evaluation for FUO, the patient tested positive for B. henselae (Table 1). A diagnosis of disseminated CSD was made based on the presence of splenic microabscesses, granulomatous retinitis and multifocal osteomyelitis, and treatment was initiated with gentamicin, rifampicin and doxycycline (RIF/DOX), with resolution of fever at day 3. The patient completed 7 weeks of RIF/DOX and had a favourable outcome.
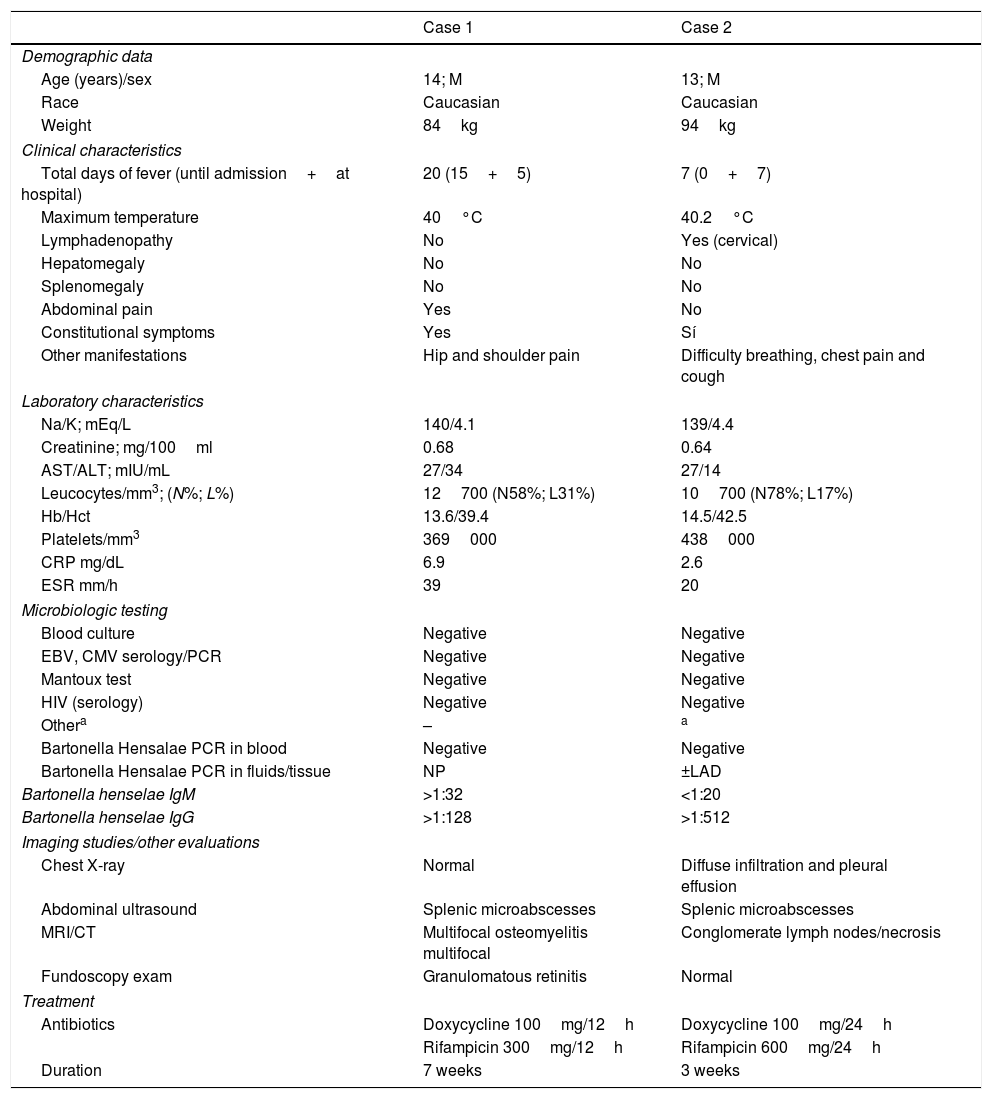
Clinical, diagnostic and management characteristics.
| Case 1 | Case 2 | |
|---|---|---|
| Demographic data | ||
| Age (years)/sex | 14; M | 13; M |
| Race | Caucasian | Caucasian |
| Weight | 84kg | 94kg |
| Clinical characteristics | ||
| Total days of fever (until admission+at hospital) | 20 (15+5) | 7 (0+7) |
| Maximum temperature | 40°C | 40.2°C |
| Lymphadenopathy | No | Yes (cervical) |
| Hepatomegaly | No | No |
| Splenomegaly | No | No |
| Abdominal pain | Yes | No |
| Constitutional symptoms | Yes | Sí |
| Other manifestations | Hip and shoulder pain | Difficulty breathing, chest pain and cough |
| Laboratory characteristics | ||
| Na/K; mEq/L | 140/4.1 | 139/4.4 |
| Creatinine; mg/100ml | 0.68 | 0.64 |
| AST/ALT; mIU/mL | 27/34 | 27/14 |
| Leucocytes/mm3; (N%; L%) | 12700 (N58%; L31%) | 10700 (N78%; L17%) |
| Hb/Hct | 13.6/39.4 | 14.5/42.5 |
| Platelets/mm3 | 369000 | 438000 |
| CRP mg/dL | 6.9 | 2.6 |
| ESR mm/h | 39 | 20 |
| Microbiologic testing | ||
| Blood culture | Negative | Negative |
| EBV, CMV serology/PCR | Negative | Negative |
| Mantoux test | Negative | Negative |
| HIV (serology) | Negative | Negative |
| Othera | – | a |
| Bartonella Hensalae PCR in blood | Negative | Negative |
| Bartonella Hensalae PCR in fluids/tissue | NP | ±LAD |
| Bartonella henselae IgM | >1:32 | <1:20 |
| Bartonella henselae IgG | >1:128 | >1:512 |
| Imaging studies/other evaluations | ||
| Chest X-ray | Normal | Diffuse infiltration and pleural effusion |
| Abdominal ultrasound | Splenic microabscesses | Splenic microabscesses |
| MRI/CT | Multifocal osteomyelitis multifocal | Conglomerate lymph nodes/necrosis |
| Fundoscopy exam | Granulomatous retinitis | Normal |
| Treatment | ||
| Antibiotics | Doxycycline 100mg/12h | Doxycycline 100mg/24h |
| Rifampicin 300mg/12h | Rifampicin 600mg/24h | |
| Duration | 7 weeks | 3 weeks |
BH, Bartonella henselae; Hb, haemoglobin; Hct, haematocrit; M, male; NP, not performed.
Negative serologic tests for fungi and antigen tests for histoplasmosis in blood/urine samples. Immunologic testing with antibody tests (IgG, IgM, IgA and IgE), vaccine titre tests (pneumococcus and tetanus) and basic immunophenotyping of T and B cells (CD3, CD4, CD8 and CD19) all within normal ranges, HIV-negative.
The second case corresponded to a male age 13 years with underlying asthma that presented with swelling in the left side of the neck, loss of appetite and asthenia of 3 weeks’ duration. The patient had no fever. He was diagnosed with CSD in the outpatient setting (Table 1) and received treatment with azithromycin, with initial improvement of symptoms until day 4 when he developed respiratory distress requiring admission to the PICU. The patient lives with 10 cats. The main findings of physical examination were tachypnoea and a painless conglomerate of enlarged cervical lymph nodes without erythema that required drainage, with subsequent detection of B. henselae by PCR. The chest X-ray revealed interstitial infiltrates and bilateral pleural effusions requiring drainage. After 72h of treatment with levofloxacin and vancomycin, the patient showed clinical improvement and was transferred to the paediatric ward, where he developed fever and enlargement of the cervical mass that required a second drainage, after which he remained afebrile. An abdominal ultrasound revealed hypoechoic lesions in the spleen, which led to the addition of rifampicin, while azithromycin was replaced by doxycycline because of a prolonged QT interval.
The patient was diagnosed with disseminated CSD with an atypical presentation including extensive lymphadenopathy and lung involvement as well as splenic microabscesses, thus he underwent a basic immunologic work-up, with negative results (Table 1). The patient was followed as an outpatient and completed a 3-week course of RIF/DOX, with a good response.
Cat-scratch disease is a common disease worldwide, although its actual incidence is unknown.2 It presents more frequently in the form of an isolated, subacute cervical lymphadenopathy, which is usually afebrile. However, a small proportion of affected individuals develop disseminated CSD, which can have involvement of the liver, spleen, retina or osteoarticular system.3 In these cases, the most frequent reason to seek medical attention is FUO (1–3 weeks), which occurred in one of our patients. This diagnosis should be suspected from the initial history and the physical examination, with emphasis on past contact with cats, as especially kittens, are the main reservoir of B. henselae.4 The microbiologicdiagnosis is based on the detection of high titres of antibodies (IgG/IgM) against B. henselae in the acute phase of disease. Nevertheless, if there is a high suspicion of CSD and the initial antibody titers are negative, they should be repeated in 2–3 weeks. Another available option is PCR for detection of B. henselae in blood, tissue and other fluis .
The diagnosis of CSD in patients with an atpical presentation poses a challenge. In patients with FUO and suspected CSD, performance of an abdominal ultrasound is a prudent measure while awaiting the results of serologic tests, as this is a non invasive test that can detect the characteristic microabscesses in the liver or spleen, in addition to an eye fundoscopy, whose findings can not only guide the differential diagnosis of rheumatologic diseases but can also support the diagnosis of CSD.5 We also ought to underscore that there should be a high index of suspicion of osteomyelitis in these cases, as the findings of the physical examination may be unremarkable and the levels of inflammatory markers within normal range.6
The optimal antibiotic treatment for disseminated CSD is still under debate, although courses lasting 2–6 weeks are generally recommended depending on the extent of disease.1 Our patients received combined therapy with RIF/DOX, antibiotics that have been found to achieve adequate control of the disease in the past. In brief, we present 2 cases of disseminated CSD that responded to antibitic therapy, emphasising the importance of taking a detailed history , with emphasis on the investigation of epidemiologic factors, and a thorough physical examination to assess the possibility of CSD and avoid unnecessary tests when the diagnosis of FUO is being considered.
Please cite this article as: Maiques-Tobias E, Tomatis-Souverbielle C, Watson J, Ramilo O, Mejias A. Enfermedad diseminada por arañazo de gato: el amplio espectro de la presentación. An Pediatr (Barc). 2019;90:393–395.