Multiple pregnancy has increased in prevalence in the last few years, which could lead to more foetal and maternal morbidity issues. The aim of this study is to describe the trend of multiple pregnancy deliveries in Castilla y León during the last 13 years and the subsequent impact on foetal and maternal health.
Material and methodsData was collected from the hospital discharge reports registered in the Regional Health-care database (SACYL: Health care in Castilla y León) between 2001 and 2013. A cross sectional descriptive study was conducted, including trend analysis with log-linear joint point model, a rhythm metric study, as well as a risk assessment with multivariate analysis.
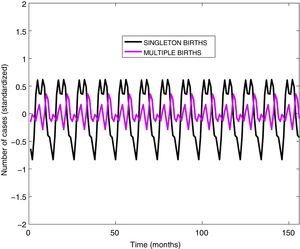
ResultsA pronounced upward trend was observed in the proportion of multiple deliveries in this time period, compared to single ones, with an annual percentage change of 3.4% (95% CI: 2.5–4.4). Multiple pregnancy was significantly correlated with advanced maternal age, abnormal glucose tolerance, dystocia and caesarean section delivery, premature birth, foetal malposition, foetal macrosomia, stillbirth, in vitro fertilisation, and hypertensive episodes of pregnancy. In vitro fertilisation showed a 9.3 fold increased risk in multiple pregnancy (95% CI: 7.4–11.5), with maternal age increasing the risk up to 5% per year of age (OR: 1.05: 95% CI: 1.04–1.05). No seasonal rhythm was observed in multiple deliveries compared with single ones.
ConclusionMultiple pregnancy has experienced a continuous increase, with no seasonal trend, and is associated with the increase in assisted reproductive technology and advanced maternal age. This involves more problems regarding foetal and maternal morbidity and mortality.
La prevalencia del embarazo múltiple está experimentando un ascenso en los últimos años, lo que conlleva un aumento de la morbimortalidad fetal y de la morbilidad materna. El objetivo de este estudio es analizar la evolución de los partos múltiples en Castilla y León durante 13 años y sus implicaciones maternas y fetales.
Material y métodosEstudio de asociación cruzada, sobre el conjunto mínimo básico de datos (CMBD), de altas hospitalarias de la red Sanidad de Castilla y León (SACYL) entre 2001 y 2013. Se realizó un análisis de tendencias mediante regresión lineal de joinpoint, un análisis ritmométrico y un análisis multivariante mediante regresión logística binaria.
ResultadosA lo largo de los 13 años de estudio se observa una tendencia creciente en la proporción de partos múltiples, en contraste con los únicos, con un porcentaje anual de cambio del 3,4% (IC del 95%: 2,5-4,4%). Se encontró asociación estadística entre la edad materna, la tolerancia anormal a la glucosa, el parto operatorio, la macrosomía fetal, el parto prematuro, la muerte fetal, las malposiciones fetales, la fecundación in vitro y los estados hipertensivos maternos y el parto gemelar, destacando que la fecundación in vitro se asocia con un exceso de riesgo de 9,3 veces de parto múltiple (IC del 95%: 7,4-11,5), así como la edad de la madre se asocia con un exceso de riesgo del 5% por cada año de edad (OR: 1,05; IC 95%: 1,04-1,05). No se evidenció estacionalidad en los partos múltiples en contraposición con los únicos.
ConclusionesLos partos múltiples experimentaron un continuo ascenso, sin seguir un ritmo estacional, asociados a la extensión del uso de las técnicas de reproducción asistida y al retraso en la edad de la maternidad, lo que conlleva mayor morbimortalidad fetal y materna.
The frequency of multiple pregnancy has been increasing steadily. According to the Sociedad Española de Ginecología y Obstetricia (Spanish Society of Gynaecology and Obstetrics), the prevalence of twin pregnancy is of 1–2%, although in recent years it has been increasing progressively in developed countries, reaching prevalences of up to 3% and 4%.1,2
This increase in multiple pregnancies is mainly due to 2 phenomena: the increase in maternal age caused by women waiting longer to become mothers, and a more widespread use of assisted reproductive technologies.3,4
Compared to singleton pregnancies, multiple pregnancies carry a higher risk of complications (congenital defects, preterm birth, intrauterine growth restriction, cerebral palsy and perinatal mortality) and their increase has contributed to differences in morbidity and mortality in children and adolescence both through time and between geographical regions.5,6
Multiple pregnancy also carries a higher risk of maternal complications such as hypertensive disorders, gestational diabetes, caesarean delivery and postpartum haemorrhage.7–9
The aim of our study was to analyse the trends in multiple pregnancies in the Spanish region of Castilla y León over 13 years, and their impact on the foetuses and mothers.
Materials and methodsWe performed a cross-sectional study by analysing data obtained from the hospital discharge summaries (“Conjunto Mínimo Básico de Datos” [CMBD], or minimum basic data set) of hospitals in Castilla y León in the database of the Public Health Network of Castilla y León (Red Sanidad de Castilla y León [SACYL]) covering the period between 2001 and 2013. We selected patients with a diagnostic code for singleton birth or multiple birth in the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-MC), which were grouped in the database according to the all-patients diagnosis-related group (AP-GRD) system, version 25.0, under codes 370–375 and 650–652.
The ICD-9-MC codes applied in delivery-related obstetric procedures were 72.xx through 74.xx, and the codes applied to multiple pregnancy were 651.xx, V27.2, V27.3, V27.4, V27.5, V27.6, V27.7, V31, V32, V33, V34, V35, V36 y V37. We collected data for the dependent variables used in the logistic regression analysis based on the ICD-9-CM codes featured in the CMBD: Hypertension complicating pregnancy childbirth and the puerperium [642.xx]; onset (spontaneous) of delivery or premature labour with onset of delivery before 37 completed weeks of gestation [644.2x]; other current conditions in the mother classifiable elsewhere but complicating pregnancy childbirth or the puerperium, including diabetes mellitus [648.0x] and abnormal glucose tolerance of mother [648.8x]; malposition and malpresentation of foetus [652.x]; other known or suspected foetal and placental problems affecting management of mother, including intrauterine death after completion of 22 weeks’ gestation [656.4x], poor foetal growth (“thin for gestational age”, “small for gestational age”) [656.5x]; excessive foetal growth (“large for gestational age”) [656.6x]; postpartum haemorrhage [666.0x, 666.1x]; pregnancy resulting from assisted reproductive technology [V23.85]; forceps, vacuum and breech delivery [72.xx] and caesarean delivery [74.x].
Statistical analysisAll the tests conducted were two-tailed for a 95% confidence level. We calculated the birth rate per 1000 inhabitants per year corresponding to all the births managed in hospitals of the SACYL network. We also calculated the rate of multiple birth per 1000 births per year in the SACYL network.
We used joinpoint linear regression to analyse temporal trends and determine whether there had been statistically significant changes in prevalence. This method can identify temporal patterns in selected patient series. In this analysis, the joinpoints or breakpoints reveal statistically significant shifts in trends (upward or downward).
Graphically, joinpoint models representing prevalence on a logarithmic scale display a series of connected segments. Any point where these segments connect is a joinpoint and represents a statistically significant change in trend. Furthermore, for each trend and segment, we calculated the annual percent change by means of generalised linear models, assuming a Poisson distribution and calculating the corresponding P-values and 95% confidence intervals (95% CI). We used the free-access software of the Surveillance, Epidemiology, and End Results programme of the National Cancer Institute of the United States.10
In addition to conducting univariate analyses with calculation of odds ratios to assess the risk associated with each dependent variable, we performed a multivariate analysis using binary logistic regression to assess the association of the type of delivery with different variables while controlling the potential effect of several cofounders. We built the model using backward elimination based on likelihood ratios. We coded the dependent variable of multiple birth as 1 (present) or 0 (absent). The independent variables in the final maximum model included the categorical variables (coded as 1 if present and 0 if absent) diabetes mellitus, abnormal glucose tolerance, instrumental delivery, caesarean delivery, macrosomia, preterm birth, foetal death, in vitro fertilisation, hypertension during gestation, delivery and puerperium, postpartum haemorrhage, malpresentation of the foetus, intrauterine growth restriction, and the continuous variable of maternal age (in years).
Analysis of trend rhythmsTo assess the presence of rhythms in each time series and compare groups, we started with an initial exploration of the dominant rhythms by means of a fast Fourier transform. We then applied the multiple-component cosinor method proposed by Alberola-López et al.11
ResultsBetween 2001 and 2013, there were a total of 251411 births in Castilla y León according to data from the Instituto Nacional de Estadística (National Institute of Statistics, INE), of which 216640 (86.2%) were managed in the SACYL hospital network. Among them, there were 3991 multiple births (1.9%), of which 97.5% were twin births.
In the 13-years period under study, we found an increasing trend in the overall number of births per 1000 inhabitants through year 2008, followed by a progressive decrease (Fig. 1). The annual percent change in the 2001–2008 interval was 3.2%, followed by a 3.8% decrease per year from 2008 through 2013.
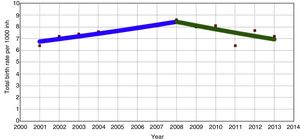
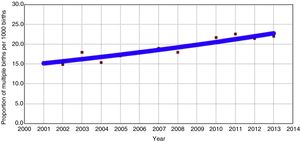
Fig. 2 represents the changes in the number of multiple births per 1000 births in the years under study, evincing an increasing trend with an annual percent change of 3.4%.
Table 1 presents the data for categorical variables summarised as percentages with the corresponding estimates of the associated risk (odds ratios) of singleton vs multiple pregnancy found in the univariate. It also presents the results of the difference of means test for maternal age, the only continuous variable analysed in the study.
Characteristics of the population under study.
| Variable | Singleton birth, n (%) | Multiple birth, n (%) | Crude odds ratio (95% CI) | Adjusted odds ratio (95% CI) |
|---|---|---|---|---|
| Age in years (mean±standard deviation) | 31.4±5.3 | 33.3±5 | Difference of means: −1.9 (95% CI, 2.1 to −1.7) | 1.05 (1.04–1.05) |
| In vitro fertilisation | 494 (0.2) | 191 (4.8) | 21.2 (17.9–25.1) | 9.26 (7.44–11.52) |
| Preterm birth | 9479 (4.50) | 1594 (39.90) | 14 (13.1–14.9) | 9.80 (9.06–10.50) |
| Foetal death | 780 (0.40) | 60 (1.50) | 4.1 (3.1–5.3) | 2.32 (1.71–3.14) |
| Intrauterine growth restriction | 4242 (2) | 280 (7) | 3.6 (3.2–4.1) | 0.96 (0.79–1.10) |
| Macrosomia | 2477 (1.20) | 15 (0.40) | 0.3 (0.2–0.5) | 0.34 (0.20–0.57) |
| Foetal malpresentation | 9976 (4.80) | 1636 (41) | 13.8 (12.9–14.8) | 6.54 (6.05–7.06) |
| Caesarean delivery | 51069 (24.50) | 2956 (74.10) | 8.8 (8.2–9.5) | 4.81 (4.41–5.24) |
| Instrumental delivery | 25604 (12.30) | 238 (6) | 0.45 (0.4–0.5) | 1.61 (1.38–1.87) |
| Hypertensive disorder | 4980 (2.40) | 334 (8.40) | 3.7 (3.3–4.2) | 1.39 (1.21–1.59) |
| Diabetes mellitus | 645 (0.30) | 12 (0.30) | 0.9 (0.6–1.7) | 0.33 (0.18–0.61) |
| Abnormal glucose tolerance | 6289 (3) | 182 (4.60) | 1.5 (1.3–1.8) | 1.03 (0.87–1.23) |
| Postpartum haemorrhage | 1247 (0.60) | 47 (1.20) | 2 (1.5–2.7) | 1.97 (1.41–2.77) |
| Number of births | 208560 (98.10) | 3991 (1.90) |
We performed a multivariate logistic regression analysis to assess the association between multiple birth and various variables related to maternal morbidity and foetal morbidity and mortality, controlling for potential confounders. Table 1 presents the associations between the variables under study and the presence or absence of multiple birth. We ought to highlight the particularly strong association between in vitro fertilisation, preterm birth, foetal malpresentation and caesarean section.
We also performed a chronobiological analysis that revealed the presence of a circannual rhythm in singleton births (P<.0001). We found a percent rhythm of 25.5%, with the acrophase on September 9 (95% CI, May 11–September 28) and the batiphase on February 27 (95% CI, September 28–May 15).
We did not find a circannual rhythm in multiple birth (P=.8). The percent rhythm was 3% (Fig. 3).
We compared rhythms by means of the amplitude-acrophase test and found differences between both groups (P=.003).
DiscussionOur study found an increase in the total number of deliveries managed in the SACYL network until 2008, the year that the number peaked, followed by a gradual descent (Fig. 1).
This trend was consistent with the overall pattern observed in Spain in the same period, as, based on data from the INE, birth rates in Spain have exhibited a declining trend since 2009, after a peak in 25 years in the number of births in 2008 following the lowest trough observed in the past 50 years.12
A factor that contributed to the initial progressive increase in births was the growth of the immigrant population, which was consistent with the rest of Spain. The immigrant population is characterised by a high birth rate. Thus, in Spain, according to data from the INE, births by immigrant mothers increased by 16.4% in 2007 with a total of 92992 births, which amounted to nearly 20% of the total births in Spain.13
However, in 2013 there were 425390 births in Spain, corresponding to a reduction of 18.1% compared to year 2008, when there were 519779 birhts.14
In the same period of time, the crude birth rate (number of births per 1000 inhabitants) had dropped to 9.1 in 2013 from 11.3 in 2008, a declining trend that is sustained.15
The definitive data published by the INE for year 2016 show that there were 410583 births, which represented a decrease of 21% compared to 2013.16
The decline in the number of births is due to a drop in the fecundity rate (in Spain, the main indicator of fecundity, the “number of children per woman”, decreased from 1.44 in 2008 to 1.27 in 2013).
The progressive decline in the number of women of reproductive age also contributes to this trend, with a decline in the number of women aged 15–49 years in Spain since 2009 owing to women that are reaching these ages belonging to smaller generations born during the “baby bust” of the 1980s and early 1990s.
The reduction in immigration and the increase in emigration in recent years have also contributed to this decrease in birth rate.
In our study, we found a proportion of 1.9% of multiple births over the total births. This proportion is similar to the one reported by the INE of 2.24% for all of Spain in 2014.17
Contrary to births overall, multiple births exhibit a sustained increasing trend, reaching rates of up to 23 per 1000 births (Fig. 2).
This proportion is smaller compared to the proportion reported by Martin et al.18 for the United States in 2013 of 33.9 twin births per 1000 births, the highest reported in that country. Subsequently, the most recent data, corresponding to births in year 2016, showed a decrease in this proportion, although it was not statistically significant (33.4 twin births per 1000 births).19
In Europe, the PERISTAT report published in 2013 with data from 2010 described variations in the frequency of multiple births, ranging from low rates between 9 and 13 per 1000 births in countries like Romania, Latvia, Lithuania and Poland, to rates of more than 20 per 1000 births in countries like, Spain, Belgium, Czech Republic, Denmark, Cyprus and Malta.20
There are 2 main reasons for this increase: late motherhood and the widespread use of assisted reproductive technologies.
The impact of advanced maternal age in multiple birth is widely accepted in the literature.2,21 We also observed this association in our study, with a 5% increase in the probability of twin birth for every additional year of maternal age (OR, 1.05 [95% CI, 1.04–1.05]).
This delay in motherhood observed in our study and in most developed countries could be related, on one hand, to women having greater knowledge of and access to birth control methods, and, on the other, to a change in the aspirations of women concerning their life trajectory, as they increase their educational attainment and join the workforce in massive numbers.
On the other hand, the use of assisted reproductive technologies has contributed to the increase in the number of multiple pregnancies in recent years. In the United States, 36% of twin pregnancies and 77% of higher order pregnancies occurred following the use of these technologies.2,20
In our study, we found a strong association between pregnancy product of in vitro fertilisation and multiple birth, with an adjusted OR of 9.34 (95% CI, 7.51–11.70).
A phenomenon of utmost importance is the increase in foetal morbidity and mortality associated with multiple birth. The variable with the strongest association was preterm birth, with an OR of 9.8 (95% CI, 9.1–10.5). It is the most frequent negative event associated with multiple pregnancy and it is associated with increases in perinatal mortality and short- and long-term morbidity due to its complications (respiratory problems, patent ductus arteriosus, intracranial bleeding, hypoxic-ischaemic encephalopathy, etc.).
Preterm birth is the factor that has the most impact on perinatal morbidity and mortality, and its frequency increases with the number of foetuses.
In the United States, the estimated proportion of twin pregnancies that end in preterm birth is 57%, with 11% of these births occurring before 32 weeks’ gestation.22 In our study, the crude preterm birth rate was 39.9%, compared to 4.5% in singleton pregnancies.
Numerous authors have concluded that perinatal and child mortality are greater in multiple pregnancies compared to singleton ones due to associated comorbidities (higher frequency of preterm birth, abnormalities in foetal development, congenital anomalies and other obstetric complications).23
The probability of foetal death or stillbirth was up to 2.3 times greater in multiple pregnancies (OR: 2.3 [95% CI, 1.7–3.1]) compared to singleton pregnancies in our series, with a relative frequency of 1.5%. Similar studies have found that in developed countries, the number of stillbirths in multiple pregnancies increases by 8.8 per 1000 births.24
It is known that inadequate foetal growth (including low weight for gestational age and intrauterine growth restriction) is associated with increased perinatal morbidity and mortality. In our study, the additional risk in the raw data corresponded to an OR of 3.6 (95% CI, 3.2–4.1), which is consistent with the reports of other authors.9,25,26 On the other hand, when we performed the multivariate analysis and calculated adjusted ORs taking into account potential confounders, the association with this variable was not statistically significant and thus was not included in the final model.
We found an inverse association with foetal macrosomia (OR: 0.3 [95% CI, 0.2–0.6]), with a 3.3-fold reduction in the risk of macrosomia in multiple pregnancies compared to singleton pregnancies, which suggests that macrosomia is infrequent in cases of multiple pregnancy in the population under study, with a stronger association with singleton pregnancy.
As we mentioned above, we obtained the data on macrosomia and preterm birth from maternal health records. More detailed information may be found in the health records of newborns that are officially admitted to hospital. This may result in a small but statistically insignificant bias in the estimation of the proportions of preterm birth and foetal macrosomia.
When it comes to maternal morbidity, we ought to highlight the strong association we found between multiple pregnancy and caesarean delivery (OR, 4.8 [95% CI, 4.4–5.2]), instrumental delivery (OR, 1.6 [95% CI, 1.4–1.9]), hypertensive disorders of pregnancy (OR, 1.4 [95% CI, 1.4–1.6]) and postpartum haemorrhage (OR, 1.9 [95% CI, 1.4–2.8]), which was consistent with the previous literature.1,7,8,27–29
Foetal malposition (coded as foetal malpresentation) is a variable that is also consistently associated with multiple gestation based on the results of our analysis, with an OR of 6.6 (95% CI, 6.1–7.1). Foetal presentation is an essential factor in choosing the mode of delivery, and therefore influences the frequency of birth by caesarean section.
In the period under study, based on the crude data, the proportion of caesarean deliveries was clearly higher in multiple pregnancies, tripling that of singleton pregnancies (74.1% vs 24.1%), an increase that is consistent with the findings of other studies.30
The literature analysing rhythmicity in births is scarce, and there are even fewer studies on the subject specifically focused on multiple births. Cancho-Candela et al.31 found that seasonal patterns in births disappeared at the end of a 60-year series, contrary to our study, where we found a seasonal pattern in singleton births.
Few authors have found seasonal patterns in multiple pregnancy.32,33 In Spain, for instance, Hernández et al.32 found a seasonal pattern in multiple pregnancies between 1801 and 1900 in Tortosa, contrary to our study, in which we found no evidence of seasonality. This could be due to the fact that the Hernández study was conducted in a population that was mainly rural at the time, when births were associated with the agricultural cycle in an attempt to prevent interference with farm work and when assisted reproductive technologies had not yet been introduced. In contrast, the use of these technologies is currently widespread in Spain in both the public and private health systems throughout the calendar year, which would account for the absence of seasonal patterns in our study.
Based on the findings of our study, we conclude that multiple births, compared to singleton births, continue to increase in frequency and do not exhibit any chronobiological rhythms.
Furthermore, multiple birth is associated with an increase in foetal morbidity and maternal complications, which we corroborated in the multivariate analysis with the calculation of odds ratios adjusted for various confounders.
Since the increase in the prevalence of multiple pregnancy is due to delayed motherhood and the use of assisted reproductive technologies, we would recommend the implementation of policies to promote earlier motherhood and interventions aimed at preventing multiple pregnancies in the context of assisted reproductive technologies.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the Department of Health of the Government of Castilla y León and the General Directorate of Innovation and Outcomes in Health for their collaboration by allowing us to access the information in the Hospital Discharge Minimum Basic Data Set (CMBD) database.
Please cite this article as: Siesto Murias P, Martín Armentia S, García-Cruces Méndez J, López-Menéndez Arqueros M, Garmendia Leiza JR, Alberola López S, et al. Evolución temporal de los partos múltiples en Castilla y León durante 13 años. An Pediatr (Barc). 2019;90:386–392.