Readmission rate is an indicator of the quality of hospital care. The aim of the study is to identify potential preventable factors for paediatric readmission.
Material and methodsA descriptive, analytical, longitudinal, and single centre study was carried out in the Paediatric Hospitalisation ward of a tertiary hospital during the period from June 2012 to November 2015. Readmission was defined as the one that occurs in the first 30 days of previous admission, as very early readmission if it occurs in the first 48h, early readmission in the 2–7 days, and late readmission after 7 days. Preventable readmission is defined as one that takes place in the first 15 days and for the same reason as the first admission. Epidemiological and clinical variables were analysed. A univariate and multivariate study was carried out.
ResultsIn the study period, 5459 patients were admitted to the paediatric hospital, of which 226 of them were readmissions (rate of readmission: 4.1%). When the hospital occupation rate was greater than 70%, the overall percentage of readmissions was significantly higher (8.5% vs 2.5%; P<.001). In the multivariate analysis, it was found that having a chronic disease and the number of visits to emergency care units before admission, are predictive factors of preventable readmission.
ConclusionsThe rate of readmissions is greater in the periods of higher care pressure. The readmission of patients with chronic condition is preventable, and therefore strategies must be designed to try to avoid them.
La tasa de reingresos hospitalarios es un indicador de calidad de la asistencia hospitalaria. El objetivo de este trabajo es describir factores de riesgo de reingreso prevenible en la hospitalización pediátrica.
Material y métodosEstudio analítico, retrospectivo, unicéntrico realizado en las plantas de Pediatría de un hospital terciario (junio de 2012 a noviembre de 2015). Se definió reingreso al que acontecía en los primeros 30 días del ingreso previo: muy precoz (en menos de 48h), precoz (2-7 días) y tardío (a partir de 7 días). Se definió reingreso prevenible al que ocurrió en los primeros 15 días y por la misma causa del primer ingreso. Se analizaron variables epidemiológicas y clínicas. Se realizó un estudio univariante y posteriormente multivariante.
ResultadosEn el período de estudio ingresaron en las plantas de Pediatría General Hospitalaria 5.459 pacientes y reingresaron 226 (tasa de reingreso del 4,1%). Cuando la tasa de ocupación hospitalaria es mayor del 70%, el porcentaje global de reingresos es significativamente mayor (8,5 vs. 2,5%), p<0,001. En el análisis de regresión de Cox se objetivó que la presencia de enfermedad de base y el número de visitas a urgencias desde el alta son factores de predicción de reingreso prevenible.
ConclusionesLa tasa de reingresos es mayor en los períodos de mayor presión asistencial. El reingreso de los pacientes con patología crónica de base es prevenible, y por lo tanto hay que diseñar estrategias para intentar evitarlo.
Hospital readmission rates are an indicator of quality of care in children's hospitals as well as a reflection of the population served by these facilites.1,2 Readmission is defined as admission within 30 days from hospital discharge.1 However, the readmission rate that correlates to quality of care is the rate corresponding to preventable readmissions. In the scientific literature, preventable readmission is defined as readmission within 15 days from discharge for the same reason that caused the previous hospitalization,1 which excludes planned readmissions by definition. The most recent epidemiological studies have found 30-day potentially preventable readmission rates of up to 30%.3 Other studies have found variable rates (range, 8.4–18%) depending on the study design, population under study and definition of readmission applied in the study.4–18 Authors have debated whether these rates are an actual reflection of care quality19,20 or are influenced by underlying chronic diseases.3 In theory, preventable readmissions are related to the quality of the inpatient care received during the previous hospitalization. In contrast, nonpreventable readmissions are mainly related to the disease itself and the complexity of the population served by the hospital. Other factors depend mostly on the outpatient follow-up at the primary care level in the first 24–48h from discharge or on patients themselves and their adherence to prescribed pharmacotherapy or health recommendations received at discharge.3 Previous studies have identified factors associated with preventable paediatric readmissions.1,2,6–8,13,15 Some of these factors are the severity of disease, prematurity, psychiatric morbidity, chronic complex disease or the reason for the previous admission. In patients with no underlying disease, the preventable readmission rate is of 14–18%, depending on the study,3 while the preventable readmission rate in patients with underlying disease (cardiovascular, neurologic) or with special needs (mechanical ventilation or polypharmacy) is as high as 25–35%.2,4
The main objectives of our study were to analyse the characteristics of readmitted paediatric patients, to attempt to identify risk factors for preventable admission and to establish preventive measures.
Materials and methodsWe conducted a single centre observational and analytical study. We collected data retrospectively for the period of June 2012–November 2015 corresponding to the paediatric ward of a tertiary care level hospital in Madrid, Spain, that has 38 general paediatrics beds and manages 1800 paediatric admissions per year. Within this period, we included all patients aged 0–16 years admitted to the paediatric inpatient ward. We excluded patients admitted to other units (neonatology, surgery, oncology, nephrology and cardiology) or those in whom readmission was planned. We defined readmission as admission happening within 30 days of a previous discharge. Depending on the time elapsed before readmission, we classified readmissions as follows: very early readmission (within 48h of discharge), early readmission (within 2–7 days of discharge) and late readmission (7–30 days after discharge). We defined preventable readmission as readmission occurring in the first 15 days post discharge for the same reason that prompted the previous admission or a clinically related reason. We obtained information on the mean length of stay of readmitted patients and occupancy rates from the Department of Admissions of the hospital. We collected data on different variables to assess the characteristics of readmissions: demographic variables (age, sex, nationality, social risk), clinical variables (diagnosis, number of procedures, length of stay in prior admission and in readmission, personal history and number of visits to the emergency department since the last discharge). We consulted the Horus platform of the health care system of the Community of Madrid to determine whether the patient had been assessed by their paediatrician after the first discharge from hospital.
We assessed the severity of readmission based on the need of high-flow oxygen therapy or admission to the intensive care unit during the stay. We defined chronic patient as a patient with underlying disease lasting longer than 3 months21 and complex chronic patient as a chronic patient whose management was more complex due to special needs (home oxygen therapy, home enteral nutrition) with shifts requiring continuous monitoring in clinics of different specialities and at different levels of care.
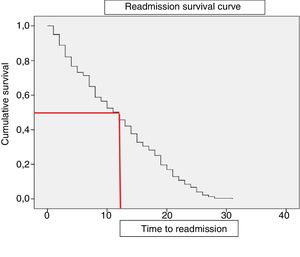
The statistical analysis was performed with the software SPSS version 21.0. (SPSS Inc., Chicago, IL, USA). We have summarised quantitative variables as mean and standard deviation or median and interquartile range (IQR) depending on whether the data followed a normal distribution. We have expressed qualitative data as percentages. We compared categorical variables by means of the chi square and Fisher exact tests, and continuous variables by means of the Mann–Whitney U and Kruskal–Wallis tests. We assessed the correlation between quantitative variables by means of the Spearman test. For the analysis of the time elapsed to readmission, we computed Kaplan–Meier survival curves. Subsequently, we performed a multivariate analysis by means of Cox regression to identify predictors associated with preventable readmission, including in the model all variables that were statistically significant in the univariate analysis or clinically relevant. We calculated the hazard ratio for each independent variable with the corresponding 95% confidence intervals. We also evaluated potential colinearity and interactions between different variables under study. Statistical significance was defined as a P-value of less than .05
ResultsReadmission rateIn the period under study, 5459 patients were admitted to the paediatric ward, of who 226 had been readmitted. Thus, the readmission rate was of 4.1%, with 1% (n=50) corresponding to early readmission and 0.6% (n=36) to very early readmission. Based on the established definitions, 69.1% of readmissions were late readmissions, 22.1% early readmissions and 15.9% very early readmissions.
In the months when occupancy was highest, greater than 70% (Fig. 1), the readmission rate was higher, a difference that was statistically significant (8.5% vs 2.5%; P<.01). The median time elapsed to readmission was 12 days (IQR, 10.1–13.8) as can be seen in the survival curve presented in Fig. 2. All patients had met the discharge criteria stipulated in the clinical protocols of the hospital at the time of discharge in the previous admission. However, only 27.4% of these patients had had a follow-up visit with their primary care paediatricians within 72h from discharge. We found no differences based on age, sex, underlying disease, proportion of preventable readmissions or need of admission to PICU between patients that followed up with their paediatrician after the initial discharge and patients that did not.
Discharge occurred during the weekend in 22 patients (0.8% of the sample). We did not find significant differences based on whether the patient was originally discharged during the weekend or on a weekday in the proportion of preventable readmissions (4.42% vs 5%, P=.50) or the time elapsed to readmission (8.5 days vs 11 days, P=.95).
Patient characteristicsThe median age of readmitted patients was 8 months (2–24 months), and 57.5% were male (n=130). Sixty-five percent of these patients (n=147) had some form of underlying or chronic disease, most frequently a respiratory disorder (35.8%; n=81), followed by prematurity (22.1%; n=50) and neurologic disorders (20.4%; n=46). Of all readmitted patients, 12.8% (n=29) had special needs, the most frequent of which were gastrostomy or nasogastric feeding (8%; n=18). The mean length of stay in the previous admission had been of 4.07 days, while the mean length of stay in the readmission was 4.7 days, a difference that was statistically significant (P=.04). Of the preceding admissions, most had been for moderate disease (69.9%, n=358), while 13.7% were for severe disease (n=31).
Preventable readmissionWhen we analysed the cohort of patients readmitted for the same reason as the previous admission (n=164), 62 were readmitted less than 7 days after discharge and 30 within 48hours of discharge, which corresponded to a proportion of preventable readmission of 1%. Of the reasons for readmission, the most common type was respiratory illness (n=131), followed by infection (n=79), gastrointestinal illness (n=62) and neurologic disorders (n=27). Nearly half of readmissions were classified as preventable (46.4%), and 27% of these patients did not have underlying disease. We performed a comparative analysis of preventable and nonpreventable readmissions (Table 1). We did not find statistically significant differences in the demographic characteristics (age, sex) of these groups, but the bivariate analysis revealed that a higher proportion of patients with severe disease or that required admission to the PICU were readmitted between 7 and 15 days after the previous discharge (preventable readmission). In addition, children admitted for gastrointestinal diseases were more likely to be readmitted in the first 48h post discharge (P<.01), while patients with respiratory illness were more likely to be readmitted after 15 days post discharge (P<.01). Patients with chronic special needs (gastrostomy, home cardiorespiratory monitoring, mechanical ventilation, etc.) that were readmitted early were readmitted in the first 48h more frequently (P=.04).
Comparison of preventable and nonpreventable readmissions.
| Preventable(n=104) | Nonpreventable(n=122) | P | ||
|---|---|---|---|---|
| ≤7 daysn=43 | 7–15 daysn=61 | ≥15 daysn=122 | ||
| Age | 8 (2–37) | 9 (3–36) | 14 (2.5–36) | .2 |
| Male sex | 48% | 60% | 58.8% | .13 |
| Mean length of stay>3 days | 31% | 49% | 58.8% | .46 |
| Severe disease | 4.8% | 25.4% | 13% | <.01* |
| Admission to PICU | 13% | 37% | 21% | <.01* |
| Chronic disease | 56% | 72% | 67% | .09 |
| Underlying respiratory disease | 51% | 65% | 62% | .47 |
| Gastrointestinal reason for admission | 67% | 38% | 15% | <.01* |
| Respiratory reason for admission | 50% | 45% | 86% | <.01* |
| Chronic special needs | 1.5% | 10% | 6% | .16 |
Lastly, in the Cox regression analysis we found 2 covariates that were independently associated with preventable readmission: the presence of underlying disease (hazard ratio=1.51; 95% confidence interval [CI], 1.07–2.27; P=.04) and the number of emergency visits after discharge (hazard ratio=1.66; 95% confidence interval [CI], 1.11–2.48]; P=.01) (Table 2).
Predictors of preventable readmission in a Cox regression model.
| Predictors | Preventable readmissionHR (95% CI) | P |
|---|---|---|
| Age | 1.02 (0.9–1.06) | .32 |
| Severity | 1.27 (0.73–2.13) | .38 |
| Underlying disease | 1.51 (1.07–2.27) | .04* |
| Emergency visits | 1.66 (1.11–2.48) | .01* |
| Mean LOS | 1.01 (0.95–1.07) | .68 |
| Respiratory admission | 0.69 (0.47–1.01) | .06 |
| Gastrointestinal admission | 1.18 (0.69–2.01) | .52 |
CI, confidence interval; HR, hazard ratio; LOS, length of stay.
We analysed age and mean length of stay as continuous variables, and all other variables as dichotomous variables. Values marked with an asterisk were statistically significant.
This is the first study focused on readmissions in a general paediatrics ward, and it contributes data on some clinical factors that could be used to prevent readmission, although we did exclude postoperative complications, unlike what has been done in previous studies. We found that the unplanned readmission rate was significantly lower compared to previous studies (4.1% vs 29%).3 This discrepancy may be due to the study design, as we excluded patients admitted to other paediatric specialty units, such as cardiology, oncology, etc, which were included in other studies. The 2 risk factors for preventable readmission found in our study were the presence of underlying disease and the number of emergency visits post discharge, subsets of patients that clearly need to be taken into account in the development of prevention strategies.
In our sample, readmissions seemed to be associated with the level of occupancy, as we found an increase in readmission rates with increasing occupancy. These results are consistent with the findings of previous studies in adult patients, which found that occupancy rates greater than 95% were significantly associated with an increase in nonpreventable readmissions. One of the proposed explanations is that high occupancy rates resulting from increased caseloads could motivate early discharges due to the demand for beds for other patients, which would increase unplanned readmissions.10–12 We have found no studies in the paediatric population analysing the association of readmission with health care caseloads. Such early discharges could have an impact on the time devoted to explaining to the patient the discharge recommendations and ensure adherence to treatment and special care based on the patient's condition.
Hospital readmissions have an impact not only on quality of care, but also on health care expenditure. Previous studies have described associated costs amounting to 3.4 billion dollars of the total annual inpatient charges.7 Furthermore, as evinced in our study, the mean length of stay is longer in readmissions compared to the previous admission, which further contributes to the increase in inpatient care costs.
Although most readmissions were late readmissions, nearly 50% of these were considered preventable, so this percentage needs to improve if we are to improve the quality of care. None of the baseline demographic characteristics, including age, was associated with the risk of preventable admission in our study, unlike other studies where readmissions were more frequent in infants aged less than 1 year.4 However, many children with underlying chronic diseases were readmitted within a few days (65%). The multivariate analysis showed that complex chronic disease was associated with preventable readmission independently of other clinical factors, such as patient age or disease severity. This finding was consistent with those of other previous studies that found how chronic disease progression and complications of health care procedures were the most common reasons for readmission.1,7,9,13–20,22
The clinical reason for readmission has been investigated as a possible patient-related predictor of preventable readmission. In our study, readmissions due to gastrointestinal disorders seemed to occur earlier and be preventable in a higher proportion of cases compared to those due to other medical conditions. In opposition, readmissions due to respiratory diseases seemed to occur later, which diverged from other studies where respiratory decompensation is a factor involved in preventable readmission. This discrepancy is probably due in part to epidemiological and cultural differences in care delivery between countries.
Some of the strategies used to prevent paediatric readmissions are discharge planning and post-discharge follow-up in coordination with primary care. A salient finding in our study was that only 27.4% of discharged patients had a follow-up visit with their primary care paediatrician. This could be a risk factor for readmission, but it did not seem to have an impact on preventable readmissions. Recent studies focused on the prevention of readmission recommend investigating predictors of preventable readmission by means of interviews with parents, patients aged more than 12 years and primary care physicians.3,16,17
Our strategies to prevent these readmissions must mainly focus on patients with underlying chronic disease, as the latter is associated with preventable readmission. However, they should also consider patients discharged after admission for gastrointestinal disease or that had severe diseases or required admission to the PICU, as these carried a higher probability of preventable readmission, even if these variables were not significant predictors in the multivariate analysis. Some of the strategies implemented recently after performance of this study were coordination with primary care through a link nurse system to plan the discharge and subsequent follow-up of the patient. New paper-based and online documentation has been attached to the discharge summary with clinical recommendations after discharge and recommendation for the care of the patient with special needs. We have also implemented a “hospital follow-up visit 24h post discharge” policy for patients with preventable risk factors for readmission (mainly patients with chronic disease), with scheduling of a visit within 1 week of discharge to prevent readmission and ensure adherence to treatment. For patients with underlying disease and reduced mobility, we have established a “telemedicine consultation” that allows the hospital paediatrician to get in touch with the patient at home. The post-discharge follow-up of these patients could not only reduce the readmission rate, but also decrease the number of emergency visits after discharge, as we found in our study. It can also have a substantial impact on care quality and inpatient care costs, although the actual results of these strategies have yet to be evaluated.
There are limitations to our study due to its retrospective design, as we could not verify, among other aspects, whether the patients in the sample were readmitted in a different hospital. Thus, we cannot assess the risk of readmission in patients, but rather compare readmission rates in different periods and therefore different patients. Furthermore, we could not obtain data on the social situation of the patients or any potential language barriers of parents, which could be factors influencing readmission. Also, the sample only included children admitted to the general paediatrics ward, which may limit the generalization to other hospitals with different models of care delivery. However, we identified a need to pay especial attention to the follow-up of chronic patients, which is a care quality strategy shared by different health care institutions.
ConclusionsFifty percent of the readmissions in our study were potentially preventable on account of hospital- and patient-related factors related to the quality of care and the characteristics of the served population. In our sample, underlying chronic disease was a predictor for readmission, which highlights the need to develop strategies for the follow-up of these patients with the purpose of improving the quality of their care and prevent readmissions.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pérez-Moreno J, Leal-Barceló AM, Márquez Isidro E, Toledo-del Castillo B, González-Martínez F, González-Sánchez MI, et al. Detección de factores de riesgo de reingreso prevenible en la hospitalización pediátrica. An Pediatr (Barc). 2019;91:365–370.
Previous presentations: this study was presented at the Congress of the Sociedad Española de Calidad Asistencial, October 19, 2016; Cordoba, Spain; and at the 64th Congress of the Asociación Española de Pediatría, June 2–4, 2016, Valencia, Spain.