The admission of minors into adult psychiatric units is a problem due to the lack of adequate resources and epidemiology data.
ObjectiveThe aim of this study is to describe and analyse the sociodemographic and clinical characteristics of minors that were admitted into the Short-Stay Psychiatric Hospitalisation Unit of Caceres, Spain.
Materials and methodsA retrospective, observational, and descriptive study was conducted on a sample of patients between 12 and 18 years-old admitted to the Psychiatric Unit. The study period was between 1 January 2014 and 31 December 2018.
ResultsA total of 79 patients, with a mean age of 15.72 (±1.65) years, were included. Almost all of them (93.6%) had a personal psychiatric history. The most common diagnoses at discharge in males were disruptive, impulse-control and conduct disorders, and mood disorders in females. A history of substance consumption was present in 40.6%, and was more common in males, which led to a worse prognosis. The mean stay was 5.4 (±4.7) days. Prolongation of the mean stay was associated with a history of previous psychiatric admissions, the number of diagnoses at discharge, a greater number of drugs at discharge, and those that received long-acting injectable antipsychotic drugs (P < .005 in all cases).
ConclusionsThe study identified the sociodemographic and clinical profile of the minor admitted to the Psychiatric Unit, and how the hospital stay was associated with previous psychiatric history, as well as diagnostic and clinical complexity.
El ingreso de menores en unidades de hospitalización de psiquiatría de adultos constituye un problema debido a la ausencia de recursos adecuados y de datos epidemiológicos.
ObjetivoDescribir y analizar las características sociodemográficas y clínicas de los menores que ingresaron en la Unidad de Hospitalización Breve de Psiquiatría en Cáceres.
Sujetos y MétodosEstudio observacional, descriptivo y retrospectivo. La muestra estuvo definida por pacientes de edades comprendidas entre los 12 y 18 años, hospitalizados en la unidad de psiquiatría. El periodo de evaluación fue entre el 1 de enero de 2014 y el 31 de diciembre de 2018.
ResultadosSe incluyeron 79 pacientes. La edad media fue de 15,72 (±1,65) años. El 93,6% presentaron antecedentes psiquiátricos personales. El diagnóstico al alta más frecuente en los varones fueron los trastornos destructivos del control de impulsos, y en las mujeres, los trastornos afectivos. El 40,6% presentaron antecedentes de consumo de sustancias, siendo más frecuente en varones, lo cual empeoraba el pronóstico. La estancia media fue de 5,4 (± 4,7) días. La prolongación de la estancia media se relacionó con los antecedentes de ingresos psiquiátricos previos, el número de diagnósticos al alta, un mayor número de fármacos al alta y aquellos que recibieron antipsicóticos inyectables de liberación prolongada (p < 0,005 en todos los casos).
ConclusionesEl estudio identifica el perfil sociodemográfico y clínico del menor ingresado en la unidad de psiquiatría y como la estancia hospitalaria se asoció a antecedentes psiquiátricos previos y una complejidad diagnóstica y clínica.
Approximately 10%–20% of children and adolescents in Spain suffer from mental health disorders,1 which are severe in 4%–6%.2,3 In minors, these disorders are most commonly managed at the outpatient level in mental health centres specialised in this age group. Patients that have poor outcomes with outpatient care or that have more severe symptoms may require inpatient psychiatric care. As early as 2006, the Mental Health Strategy of the National Health System4 noted that delivery of high-quality community-based mental health care to the paediatric population required a network of services that should include at least a mental health unit, a short stay unit and day hospital services. Regional governments in Spain have developed resources in varying degrees, and many autonomous communities still lack the basic services required to care for this population.5,6 In Extremadura, there are no specific inpatient resources, and patients have to be admitted to adult inpatient units that are not structured or organized to care for underaged patients.7 There is also no automated system to collect and standardize clinical and health care data to gain a better understanding of this issue. The only datum available about the number of minors managed in the psychiatric unit in Caceres is from 2012, when there were 12 admissions, the highest number among all units in the region of Extremadura.8
Thus, there may be differences in the sociodemographic and clinical characteristics of patients depending on the study, both in Spain and in the international literature. While some studies report that the most frequent reasons for admission are suicide attempts and conduct disorders,9–11 other studies report a predominance of eating disorders.12 There are also studies that report personality disorder diagnoses13,14 or substance use disorders.9
Psychiatric hospitalization in the paediatric population is most effective when the stay is not brief and when the patient exhibits a positive response to treatment of the disorder during the stay.15,16 Still, a study conducted by Zeshan et al.17 with the ultimate aim of improving the quality and cost-effectiveness of inpatient care found that the factors associated with longer lengths of stay were multiple psychiatric diagnoses, the use of restrictive measures, not living with biological parents, family history of mental illness, legal problems, substance use and schizophrenia spectrum disorders.
Despite the importance of mental health disorder in minors as the leading cause of health-related disability and its long-lasting effects through the lifespan, the mental health needs of this age group continue to be neglected. At the same time, the studies published to date exhibit substantial variability in their results due to differences in the age composition of study samples and the methodology used. In short, it is difficult to obtain an accurate perspective on the current situation of paediatric mental health services in Spain, which in turn makes it difficult to develop measures to improve it.5
The aim of our study was to describe and analyse the sociodemographic and clinical characteristics of children and adolescents admitted to the psychiatric short stay unit (SSU) in Caceres, Spain, and identify potential risk groups within this population.
Sample and methodsWe conducted a retrospective, observational and descriptive study in the psychiatric SSU of the Complejo Hospitalario Universitario de Cáceres. This hospital serves a population of 193 971 inhabitants, of who 33 946 are aged less than 20 years.18 The SSU is meant for the hospitalization, treatment and temporary management of patients (usually adults) with acute psychiatric problems with the aim of reducing the symptoms, and is part of the mental health care network of Extremadura.7 Since there is no specific resource for the hospitalization of minors with mental health problems, they are admitted to the SSU.8
The sample consisted of patients aged 12–18 years admitted to the SSU. The study period comprehended 5 years, from January 1, 2014 to December 31, 2018.
We retrieved data from the discharge reports stored in the official electronic health records database of the Department of Health of Extremadura (JARA®). We collected data on sociodemographic variables (age, sex, residential setting, composition of family of origin, siblings, birth order, adoption, educational attainment, academic performance, school attendance), personal history (medical disease, substance use, mental health problems, psychiatric hospitalization or mental health/substance use), clinical variables (day, month and year of admission, length of stay, reason for admission, legal status of patient concerning admission) and treatment variables (pharmacotherapy, restrictive measure4s, destination/referral after discharge). The principal discharge diagnosis was coded applying the criteria of the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5).19
The study adhered to current law and regulations and the principles of the Declaration of Helsinki at all times, including Organic Law 3/2018, of December 5, on Data Protection and Guarantee of Digital Rights, anonymizing personal data by encoding patient names, thus preventing identification and safeguarding the confidentiality of patients. The study was also approved by the Research Ethics Committee of Caceres.
Statistical analysisWe performed a descriptive analysis of all the variables under study. We summarised categorical variables as percentages and quantitative variables as mean and standard deviation (SD).
We assessed the association between qualitative variables with the χ2 or Fisher exact test. We compared quantitative variables with parametric tests (Student t and ANOVA) or nonparametric tests (Mann–Whitney U and Kruskal–Wallis) based on whether the data followed a normal distribution (Kolmogorov–Smirnov test), and also the Spearman correlation coefficient.
The analysis was performed with the software SPSS version 18.20 Statistical significance was defined as a p-value of less than 0.05 (two-tailed tests).
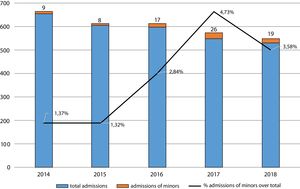
ResultsThe sample consisted of 79 patients admitted to the SSU. Fig. 1 presents the distribution of admissions per year. Overall, admissions of minors amounted to 2.77% of the total admissions in the unit.
The mean age of patients was 15.72 ± 1.65 years, with a minimum age of 12 years. Table 1 summarises the sociodemographic characteristics of the sample. Of the 79 minors, 17.4% (n = 12) were only children. Only 3.8% (n = 3) had been adopted. Behavioural problems were the most frequent reason for admission (51.9%; n = 41), while disruptive, impulse-control and conduct disorders were the most frequent discharge diagnoses. Forty-nine patients (62%) had a single discharge diagnosis, and the rest had 2 or more. Table 2 presents clinical and treatment variables in the sample.
Sociodemographic characteristics of minors admitted to the psychiatric short stay unit of Caceres (2014–2018).
| n (%) | |
|---|---|
| Sex | |
| Male | 37 (46.8%) |
| Female | 42 (53.2%) |
| Residential setting | |
| Urban | 45 (57%) |
| Rural | 34 (43%) |
| Personal history of medical illness | |
| Yes | 3 (3.8%) |
| No | 76 (96.2%) |
| Personal history of mental illness | |
| Yes | 73 (93.6%) |
| No | 5 (6.4%) |
| Previous psychiatric treatment | |
| Yes | 62 (79.5%) |
| No | 16 (20.5%) |
| Previous psychological treatment | |
| Yes | 55 (80.9%) |
| No | 13 (19.1%) |
| History of previous psychiatric hospitalization | |
| Yes | 21 (26.9%) |
| No | 57 (72.2%) |
| Living situation | |
| Both parents | 36 (46.2%) |
| One parent | 25 (32.1%) |
| Other relatives | 2 (2.6%) |
| Emergency shelter | 10 (12.8%) |
| Living alone | 1 (1.3%) |
| Shared flat | 2 (2.6%) |
| Special education centre | 1 (1.3%) |
| Group home | 1 (1.3%) |
| Educational attainment | |
| Year 1 ESO | 2 (4.9%) |
| Year 2 ESO | 9 (22%) |
| Year 3 ESO | 6 (14.6%) |
| Year 4 ESO | 10 (24.4%) |
| Year 1 Bachillerato | 4 (9.8%) |
| Year 2 Bachillerato | 3 (7.3%) |
| Vocational school | 4 (9.8%) |
| University | 3 (7.3%) |
| Academic performance | |
| Grade appropriate for age | 18 (34%) |
| Held back | 35 (66%) |
| School attendance | |
| Regular attendance | 33 (55.9%) |
| Not attended in the past few months | 16 (27.1%) |
| Dropped out completely | 10 (16.9%) |
Bachillerato, non-compulsory secondary education; ESO, compulsory secondary education.
Clinical and treatment variables in the hospitalization of minors in the psychiatric short stay unit of Caceres (2014–2018).
| n (%) | |
|---|---|
| Reason for admission | |
| Behavioural problems | 41 (51.9%) |
| Suicidal ideation | 26 (32.9%) |
| TCA | 6 (7.6%) |
| Psychotic symptoms | 3 (3.8%) |
| Anxiety/depression symptoms | 2 (2.5%) |
| Under evaluation | 1 (1.3%) |
| Principal psychiatric diagnosis at discharge | |
| Disruptive, Impulse Control and Conduct Disorders | 24 (30.4%) |
| Depressive/anxiety disorders | 15 (19%) |
| Personality disorders | 11 (13.9%) |
| Substance use disorders | 9 (11.4%) |
| Feeding and eating disorders | 7 (8.9%) |
| Neurodevelopmental disorders | 6 (7.6%) |
| Diagnosis deferred | 6 (7.6%) |
| Schizophrenia and other psychotic disorders | 1 (1.3%) |
| Pharmacological treatment | |
| No pharmacological treatment | 3 (3.8%) |
| Antidepressants | 2 (2.5%) |
| Anti-anxiety drugs | 3 (3.8%) |
| Antipsychotics | 18 (22.8%) |
| ADe + AAn | 19 (24.1%) |
| APs + AAn | 6 (7.6%) |
| APs + ACo | 7 (8.9%) |
| APs + ADe | 6 (7.6%) |
| APs + ADe + AAn | 2 (2.5%) |
| ADe + ACo + AAn | 6 (7.6%) |
| APs + amphetamine | 1 (1.3%) |
| APs + ACh | 1 (1.3%) |
| APs + ADe + ACo | 1 (1.3%) |
| APs + ADe + ACo + AAn | 1 (1.3%) |
| APs + ADe + ACo + ACh | 1 (1.3%) |
| APs + ACo + AAn | 2 (2.5%) |
| Number of drugs | |
| No drugs | 3 (3.8%) |
| 1 drug | 22 (27.8%) |
| 2 drugs | 36 (45.6%) |
| 3 drugs | 15 (19%) |
| 4 drugs | 3 (3.8%) |
AAn: anti-anxiety drug; ACh: anticholinergic drug; ACo, anticonvulsant drug; ADe, antidepressant drug; APs, antipsychotic drug; FED, feeding and eating disorders.
We found statistically significant differences in clinical characteristics between male and female patients. When it came to the reason for admission, behavioural problems were more frequent in male patients (n = 25; 31.6%), while suicidal ideation was more frequent in female patients (n = 17; 21.5%) (Fisher exact test, P = .046). As for the psychiatric discharge diagnosis, in male patients, disruptive, impulse-control and conduct disorders were most frequent (n = 14; 17.7%), followed by substance use disorders (n = 9; 11.4%) and neurodevelopmental disorders (n = 6; 7.6%). In female patients, the most frequent diagnoses corresponded to mood disorders (n = 11; 13.9%), followed by personality disorders (n = 8; 10.1%) and eating disorders (n = 7; 8.9%) (χ2 = 29.19; P < .001). The diagnosis was deferred in 7.6% of patients (n = 6).
When it came to pharmacological treatment, the active ingredients used most frequently in each therapeutic class were risperidone (n = 26), fluoxetine (n = 18) and lorazepam (n = 20). Six patients (7.6%), all male, received a long-acting injectable (LAI) antipsychotic. The use of physical restraint was necessary to control the behaviour of 16 patients (21.8%). After the hospital stay, 79.8% (n = 63) of the patients were discharged home, and the rest were referred back to the special education centre, residential facility or legal placement where the patient was staying prior to admission.
The most frequent pattern of substance use was the combination of alcohol, tobacco and cannabis use in a single patient (18.8%), followed by the combination of tobacco and cannabis (8.7%), tobacco (7.2%) and alcohol (7.2%). Table 3 presents the differences between groups in the consumption of legal substances (including tobacco and alcohol) and illegal substances. We were unable to determine whether the patient used any substances in 10 cases (12.7%). Consumption of illicit substances was documented in 40.6% of the sample (n = 28) and was more frequent in male patients than in female patients (P = .001). Poor academic performance was more frequent in the group that consumed substances (P = .026), as was dropping out of school (28.6% vs 12.9%), although the latter difference was not statistically significant. When we compared the reasons for admission, we found that most patients that used illegal drugs were admitted due to behavioural problems. The most frequent discharge diagnoses in patients that used substances were disruptive, impulse-control and conduct disorders. In addition, patients that used illegal substances were more likely to have 2 or more discharge diagnoses.
Comparison of minors that consumed legal substances versus minors that used illegal substances admitted to the psychiatric short stay unit in Caceres, Spain (2014–2018).
| Legal substances (n = 41) | Illegal substances (n = 28) | P | |
|---|---|---|---|
| n (%) | n (%) | ||
| Sex | |||
| Male | 12 (17.4%) | 20 (29%) | .001a |
| Female | 29 (42%) | 8 (11.6%) | |
| Academic performance | |||
| Grade appropriate for age | 13 (27.1%) | 2 (4.2%) | .026a |
| Held back | 17 (35.4%) | 16 (33.3%) | |
| Reason for admission | |||
| Behavioural problems | 16 (23.2%) | 19 (27.5%) | .02 |
| Suicidal ideation | 18 (26.1%) | 5 (7.2%) | |
| Psychotic symptoms | 0 (0%) | 3 (4.3%) | |
| Eating disorder | 4 (5.8%) | 1 (1.4%) | |
| Anxiety/depression symptoms | 2 (2.9%) | 0 (0%) | |
| Evaluation | 1 (1.4%) | 0 (0%) | |
| Number of diagnoses | |||
| 1 | 31 (44.9%) | 12 (17.4%) | .011a |
| 2 or more | 10 (14.5%) | 16 (23.2%) | |
| Principal psychiatric diagnosis at discharge | |||
| Neurodevelopmental disorder | 2 (2.9%) | 1 (1.4%) | |
| Schizophrenia/other psychotic d. | 1 (1.4%) | 0 (0%) | |
| Mood disorder | 12 (17.4%) | 2 (2.9%) | .003 |
| Feeding/eating disorder | 4 (5.8%) | 1 (1.4%) | |
| Disruptive, impulse-control conduct d. | 11 (16%) | 12 (17.4%) | |
| Substance use disorder | 0 (0%) | 9 (13%) | |
| Personality disorder | 6 (8.7%) | 3 (4.3%) | |
d., disorder.
The mean length of stay was 5.42 ± 4.8 days, with a range of 1–28 days. The length of stay varied between subgroups in the sample, as can be seen in Table 4. The mean length of stay was longer in patients with a past history of psychiatric hospitalization and patients that had 2 or more psychiatric diagnoses. In relation to the drugs prescribed at discharge, we found that minors given prescriptions for LAI antipsychotics had longer lengths of stay, a difference that was statistically significant in the comparison with patients that did not receive any pharmacological treatment. We also found that the length of stay in days increased proportionally with the number of drugs prescribed at discharge (r = 0.468, P < .01).
Comparison of length of stay (in days) in different groups of minors admitted to the psychiatric short stay unit of Caceres (2014–2018).
Last of all, we found statistically significant differences in the number of drugs prescribed at discharge based on the past history of psychiatric hospitalization. Thus, while patients without a past history of psychiatric hospitalization (n = 57; 73.1%) were treated with a mean of 1.75 ± 0.8 drugs, patients with a past history of psychiatric hospitalization (n = 21; 26.9%) were treated with a mean of 2.43 ± 0.8 drugs (U = 346; P = .002).
DiscussionAt present, there is insufficient epidemiological data on the number of minors that require inpatient psychiatric care. As we observed in this unit in Caceres, although the total number of admissions declined in the study period, the number of admissions corresponding to minors did increase. We also found evidence of this increasing trend in psychiatric admissions in paediatric patients when we analysed the Minimum Basic Discharge Data Set (Conjunto Mínimo Básico de Datos de las Altas Hospitalarias [CMBD]) nationwide database of Spain21 for the 2004–2013 period, which showed a 4.17-fold increase in admissions due to child and adolescent mood disorders that stabilised in the last few years. This trend should be investigated further in studies of larger scope with participation of other inpatient units at the regional and national level.
The typical sociodemographic profile of minors admitted to the psychiatric SSU of Caceres was a female patient aged 15.72, residing in an urban setting and currently managed at the outpatient level. This was consistent with the findings of several previous studies.9,12,13,17,22,23 We also found a significant proportion of patients with poor academic performance, which was also documented by Cabrejos et al.,24 which underscores the need to deliver comprehensive care to minors, including interventions that address educational challenges.
However, when we analysed variables related to the household, we found contradictory results. While our data for Caceres, consistent with other studies,13,25,26 showed that most patients lived in a nuclear family (with 1 or 2 parents), a recent study found that most paediatric patients admitted to a psychiatric inpatient ward lived in foster homes, which could be considered a risk factor for hospital admission.27 These disparities could be explained by differences in sampling.
The most frequent reasons for admission were behavioural changes in male patients and suicidal ideation in female patients. Broadly speaking,23,28 mood disorders are more prevalent in female individuals while conduct disorders are more prevalent in male individuals. These differences based on sex were recently described by Marchant et al.,29 who found that hospital admission following a suicide attempt was more frequent in girls and young women, especially in the 10-15 years age group.
In terms of diagnoses, we found a high proportion of minors with personality disorders, as previously reported by other authors.13,14,30 This is a controversial issue, as international diagnostic classifications suggest that the use of these diagnoses should be restricted in the paediatric age group. Thus, the DSM-5 proposes that they can be applied to children or adolescents in exceptional cases when the maladaptive pattern is pervasive, persistent and unlikely to be limited to a particular developmental stage or an episode of another type of mental health disorder.19 This aspect should be investigated thoroughly to establish an adequate diagnosis in these stages of development, which would improve the approach to treatment.
As for the restrictive measures applied during admission, we found that 21.8% of patients required physical restraint, mainly due to psychomotor agitation. This is a high percentage compared to a study conducted in Finland that reported use of physical restraint in only 4% of hospitalised patients, in most cases due to aggressive behaviour.31 Therefore, the current protocols applied in the SSU of Caceres should be revised, searching for alternatives that would allow a reduction in the use of restrictive measures.32
Consumption of illegal substances was frequent in male patients, with cannabis being the most frequently consumed drug, in agreement with other studies.33,34 The association between substance use and severe mental illness is well known. It is correlated to a poorer psychosocial adjustment and response to treatment, and therefore to poorer outcomes and rates of recovery.35 Thus, the subset of patients admitted to the SSU that used substances performed worse in school, with a higher proportion of patients that had been held back a year or dropped out of school. At the time of discharge, substance use was significantly associated with the number of discharge diagnoses, as the proportion of patients with 2 or more diagnoses was greater compared to the group that did not use substances. Overall, use of illegal substances was a predictor of poorer outcomes in minors admitted to the psychiatric SSU in Caceres, highlighting the need to establish preventive strategies to address this particular issue.36
Last of all, the mean length of stay was short, which is consistent with the goal of controlling acute psychiatric decompensations and reducing the impact of hospitalization in minors and their social environment.26,27 The length of stay varies based on the type of study, the profile of patients included in the sample and the type of unit where patients are hospitalised. Thus, the length of stay tends to be longer in specialised child and adolescent psychiatric units, as the care setting is different and the objectives of hospitalization may not be limited to the control of decompensations, but may also include establishing long-term therapeutic interventions.10
In our sample, the mean length of stay was longest in patients with a past history of psychiatric hospitalization, patients with 2 or more psychiatric diagnoses at discharge and patients treated with LAI antipsychotics. We also found a moderate correlation between the length of stay and the number of prescribed drugs. The past history of hospitalization is most important among all these factors,13 as these are also the patients with the greatest number of drugs prescribed at discharge. Similarly, Palma et al. found higher levels of anxiety in patients with a previous history of psychiatric hospitalization compared to patients admitted to a psychiatric unit for the first time.37 Thus, close follow-up of paediatric patients is recommended following discharge, with interventions specifically aimed at promoting recovery and preventing additional admissions associated with a poorer prognosis.
The main limitation of the study is the small number of patients included in the sample. Nevertheless, the findings reflect the clinical characteristics and situation in our area and are based on real-world patients with diverse backgrounds. On the other hand, the retrospective nature of the study precluded investigation of other clinical variables or the use of standardised assessment tools to fully evaluate the symptoms of hospitalised patients. In any case, the obtained evidence allows the formulation of initial hypotheses to be tested in future studies.
In conclusion, the typical profile of minors admitted to the psychiatric SSU of Caceres is that of a female patient, aged 15 years, with a mood disorder, a personal history of psychiatric disease, currently treated at the outpatient level and with poor academic performance. The most frequent diagnoses in male patients corresponded to disruptive, impulse-control and conduct disorders. Efforts must be made to reduce the use of restrictive measures. Substance use is associated with poorer outcomes. A previous history of psychiatric hospitalization and clinical complexity seemed to be associated with a longer length of stay.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Molina-Castillo JJ, Leonés-Gil EM, López-Espuela F. Análisis descriptivo de los ingresos de menores de edad en una unidad de psiquiatría. An Pediatr (Barc). 2021;94:11–18.