Despite similar disease severity scores; we found a higher crude death rate in the group of immigrant children compared to the group of native children in a paediatric intensive care unit. Our study aimed to compare descriptive data and standardised mortality ratios (SMR) in order to analyse differences in mortality.
Material and MethodsWe conducted a retrospective study comparing demographic characteristics, diagnostic data, disease severity scores and mortality in immigrant children of Syrian descent and children of Turkish descent. We included data for the medical and surgical patients admitted in 1 year. The sample included 1283 patients.
ResultsWe compared the age and sex distribution, presence of underlying disease, frequency of community-acquired infectious diseases, length of say, PRISM scores, SMR and crude death rates in the 2 groups.
There were 1077 patients in the Turkish group and 206 patients in the immigrant group. The proportion of patients with underlying disease was greater in the Turkish group (42% vs 37.4%). The proportion of patients with a community-acquired infectious disease as the presenting complaint was similar in both groups (52.9% vs 47.4%). The mortality in patients with infectious disease was higher in the immigrant group (19.3% vs 9.8%). There was not significant difference in the mean PRISM score between the 2 groups. We found a higher mortality in the immigrant group (16% vs 11%). The standardised mortality ratio was 0.32 in the total sample, group; 0.4 in the immigrant group and 0.24 in the Turkish group.
ConclusionsIn our study, we found an association between community-acquired infectious disease and increased mortality in the immigrant group. The underlying mechanism for this increase remains to be explained and further research is required to determine whether parameters related to infection should be added to this severity score for its use in this specific population.
A pesar de tener puntuaciones similares en la escala de gravedad, en una unidad de cuidados intensivos pediátricos se observó una tasa cruda de mortalidad superior en el grupo de niños inmigrantes sirios en comparación con el grupo de niños autóctonos turcos. El objetivo del estudio fue comparar datos descriptivos y la tasa estandarizada de mortalidad (TEM) para analizar diferencias en la mortalidad.
Materiales y MétodosEstudio retrospectivo con comparación de características demográficas, datos diagnósticos, puntuaciones de gravedad y mortalidad en niños inmigrantes de origen sirio y niños de origen turco. Se incluyeron en el análisis datos de pacientes médicos y quirúrgicos ingresados en un período de un año. La muestra incluyó 1283 pacientes.
ResultadosSe compararon la edad y sexo de los pacientes, la presencia de enfermedad de base, la frecuencia de infecciones adquiridas en la comunidad, la estancia en la UCIP, las puntuaciones PRISM, la TEM y la tasa cruda de mortalidad en los dos grupos.
El grupo turco lo formaron 1077 pacientes y el grupo inmigrante 206 pacientes. La proporción de pacientes con enfermedad subyacente era mayor en el grupo turco (42% vs. 37,4%). La proporción de pacientes en que el motivo de ingreso fue una infección adquirida en la comunidad fue similar en ambos grupos (52,9% vs. 47,4%). La mortalidad en pacientes con enfermedad infecciosa fue mayor en el grupo inmigrante (19,3% vs 9,8%). No se observaron diferencias significativas en las puntuaciones de la escala PRISM entre los dos grupos. La mortalidad fue mayor en el grupo de pacientes inmigrantes (16% vs. 11%). La TEM fue 0,32 en la muestra total, 0,4 en el grupo inmigrante y 0,24 en el grupo turco.
ConclusionesEl estudio detectó una asociación entre la presencia de infección adquirida en la comunidad y una mayor mortalidad en el grupo inmigrante. El mecanismo subyacente queda por determinar, y son necesarios estudios adicionales para establecer si deberían añadirse parámetros infecciosos a esta escala de gravedad para su uso en esta población.
The information derived from epidemiological data is essential for the administration and organisation of healthcare systems. This information may be even more critical in the management of the immigrant population, since genetic and socioeconomic factors in this collective may differ significantly from the population that health care providers are familiar with. Although there are a number of reports about the health status, diseases and relevant factors in immigrant populations, there is a dearth of data. These reports are mainly from countries where large immigrant populations form gradually through migration over a long period of time.1,2 Massive displacement of populations over a shorter time period, such as in times of war or other disasters, is fortunately not very common, but as a result there is a lack of relevant data that makes managing these populations more difficult.
The Turkish authorities have reported that as of August 2017, 7.6 million Syrians had been displaced due to armed conflicts and civil war in the country, with approximately 5.1 million people taking refuge in neighbouring countries. Turkey adopted an open-door policy in 2011 and provides free health care for Syrian asylum-seekers.3
There is an increasing number of patients who need intensive care every year for both medical and surgical indications.4 Difficulties in communication arising from language barriers, the lack of medical records and social and psychological factors stemming from war conditions all increase the burden of critical illness for both these patients and the health care staff.5
Disease severity scores are used not only for prognostication but also as indicators of care quality in the intensive care setting by analysing their correlation to mortality in the total patient population admitted over a given time interval. The standardised mortality ratio (SMR) is the ratio of the observed number of deaths over the expected number of deaths, and the latter is calculated based on disease severity scores applying statistical methods. Standardised mortality ratios and crude mortality rates are calculated periodically in critically ill patient populations.6,7
Since immigrant children are a unique population from a genetic and environmental perspective, the scores used for the native patient population in the paediatric intensive care setting may not be informative in immigrant children. In this study, we compared the demographic characteristics, diagnoses, underlying diseases, mortality, disease severity scores and SMR in immigrant children and children of Turkish descent. In addition to calculating and comparing descriptive statistics and SMRs, we aimed to analyse the reasons underlying any observed differences.
Material and methodsWe conducted a study in a 49-bed paediatric intensive care unit that admits both medical and surgical patients. At the time of the study, it was the largest paediatric intensive care unit in the city. The unit serves both Turkish and immigrant patients, as it is a public health care facility. To the best of our knowledge, there was no bias related to disparities in access to care or management between the native population and any other population in our facility, and the government covered health care costs for both Turkish and Syrian children. The hospital is the referral centre in the city for medical diagnosis and is staffed with attending physicians in all paediatric subspecialities. Although the hospital offers surgical care in every speciality, it is not a cardiac surgery or transplant centre, and therefore these patients were referred to other facilities. We included all patients aged more than 28 days and less than 18 years admitted to the paediatric intensive care unit over a 1-year period (July 2017- July 2018). All the immigrant children included in the study were of Syrian descent. The Pediatric Risk of Mortality II (PRISM II) score was the default disease severity score installed in the software of the electronic health record database of the hospital, and it was calculated for each patient using the most critical measurement values and laboratory test results found within 24 h of admission to the intensive care unit. We collected data from the electronic health records on demographic characteristics, underlying diseases, acute diagnoses, length of stay in the intensive care unit and mortality.
We compared patient age in months, sex, presence of underlying disease and community-acquired infectious disease, lengths of stay, PRISM scores and mortality rates in the Turkish patients versus the immigrant patients. We defined community-acquired infection as infectious disease with onset within 48 h of admission. We assessed the discriminatory power of the PRISM score and calculated the SMR for the overall patient population and each group (Turkish vs immigrant).
We performed the statistical analysis with the Statistical Package for Social Sciences (SPSS) version 22.0 for Windows (SPSS Inc; Chicago, IL, USA). We summarised categorical data as percentages (%) and continuous data as mean and standard deviation (SD) in case of a normal distribution or median and interquartile range (IQR) in case of a skewed distribution. We compared continuous data using the Student t test (normality assumption met) or the Mann-Whitney U test (normality assumption not met) and categorical data using the chi square test. We considered p-values of less than 0.05 statistically significant. We generated receiver operating characteristic (ROC) curves and calculated the area under the curve (AUC) to assess the sensitivity and specificity of the PRISM score in predicting mortality. We obtained a cut-off point for predicting mortality (death predicted above the threshold) for each curve using the Youden index. We calculated the SMR as the ratio of observed deaths to the predicted number of deaths.
The study was approved by the ethics committee of Harran University in Sanliurfa.
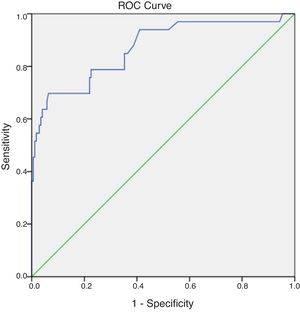
ResultsWe analysed data for 1283 patients. There were 1077 patients in the Turkish group and 206 patients in the immigrant group. The mean age of the overall sample was 39.50 ± 66.05 months. The mean age was similar in the 2 groups (P = .416 ) The male-to-female ratio was greater in the immigrant group (63.1% vs 55.4%) (P = 0.042) Table 1 summarises the main characteristics of the sample, comparing both groups.
Main characteristics of the study groups.
| Immigrant group | Turkish group | P | |
|---|---|---|---|
| Number of patients | 206 | 1077 | |
| Mean age (month) | 34.27 ± 107.08 | 40.50 ± 54.83 | .416 |
| PRISM | 13.94 ± 10.32 | 12.53 ± 10.30 | .074 |
| SMR (standardised mortality ratio) | 0.4 | 0.24 | |
| Frequency of chronic disease | 77 (37.4%) | 452 (42.0%) | .048 |
| Frequency of infectious disease | 109 (52.9%) | 510 (47.4%) | .144 |
| Length of stay in ICU (days) | 6.14 ± 8.17 | 5.35 ± 7.69 | .203 |
| Mortality | 33 (16%) | 120 (11.1%) | .048 |
In the total sample, 529 patients had underlying disease (41.2%). Table 2 lists the chronic diseases found in the sample and the corresponding proportions. The proportion of patients with underlying disease was significantly greater in the Turkish group (42% vs 37.4%) (P = 0.048).
Prevalence of chronic underlying diseases.
| Congenital heart diseases and cardiomyopathies | 12% |
| Cerebral palsy and neuromuscular diseases | 14% |
| Epilepsy | 12% |
| Hydrocephalus or ventriculoperitoneal shunt | 8% |
| Malignancies | 4% |
| Chronic renal failure | 6% |
| Diabetes mellitus and other endocrine diseases | 10% |
| Metabolic diseases | 5% |
| Genetic syndromes and other miscellaneous diseases | 29% |
The mean PRISM score was 12.76 ± 10.31 in the total sample, and we found no differences in the mean between the 2 groups (P = 0.074). The mean length of stay in the unit was similar in both groups (6.14 ± 8.17 vs 5.35 ± 7.69 days; P = 0.203). The mortality was higher in the immigrant group (16% vs 11%; P = 0.048). Since it is known that children with comorbidities have an increased rate of mortality and higher PRISM scores point to increased risk of mortality, we performed a logistic regression analysis with chronic disease and the PRISM score as potential confounders, obtaining an adjusted odds ratio of 1.715 (95% confidence interval [CI], 0.999–2.942; P = 0.05) while the crude odds ratio was 1.521(95% CI, 1.002–2.310; P = 0.049).
In the total sample, the primary diagnosis at admission was a community-acquired infectious disease in 619 patients (48.25%). The proportion of patients with a community-acquired infectious disease (such as pneumonia, sepsis, gastroenteritis or meningitis/encephalitis) as the presenting complaint was similar in the 2 groups (52.9% vs 47.4%; P = 0.144). Table 3 compares the proportions of patients with infectious diseases in each group. We did not find a significant difference in the prevalence of any of the infectious diseases between the 2 groups (P = 0.406). The mortality in patients with infectious disease was higher in the immigrant group (19.3% vs 9.8%; P = 0.008). We carried out a logistic regression analysis with chronic disease and PRISM as potential confounders and found an adjusted odds ratio of 2.97 (95% CI, 1.47–6.002; P = 0.002) and a crude odds ratio of 2.19 (95% CI, 1.2256–3.837; P = 0.006).
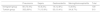
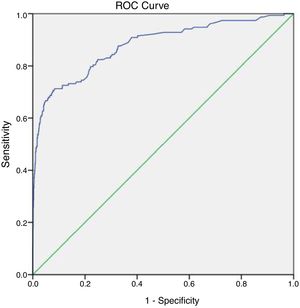
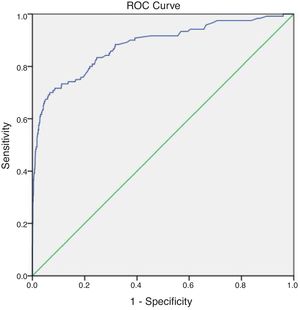
To analyse the SMR calculated using the predicted mortality derived from PRISM scores and the actual mortality in each group, we generated ROC curves for the 2 groups. We found an area under the curve (AUC) of 0.878 for the total sample (P < 0.001), with a sensitivity of 80.4% and a specificity of 76.9%. The AUC for the immigrant group was 0.869 (P < 0.001), with a sensitivity of 78.8% and a specificity of 77.5%, and a cut-off value for the prediction of mortality of 12.65. The AUC for the native Turkish group was 0.880 (P < 0.001), with a sensitivity of 83.3% and a specificity of 75.3%, and the cut-off value for the prediction of mortality was 10.45. The SMR was 0.32 for the total sample, 0.4 for the immigrant group and 0.24 for the Turkish group. Figs. 1 to 3 show the ROC curves for the total sample and each of the 2 groups.
In the subset of Turkish patients with a diagnosis of community-acquired infectious disease, the sensitivity of the PRISM score for predicting mortality was 78.0% and the specificity 40.9% (AUC = 0.569), while in the subset of immigrant patients with community-acquired infection, the sensitivity was 78.0% and the specificity 42.3% (AUC = 0.585).
DiscussionIn this descriptive study of critically ill paediatric patients, we compared immigrant children with native Turkish children. The mean age, PRISM scores, proportion of patients with community-acquired infectious disease as the presenting complaint and the length of stay in the PICU were similar in both groups, while the proportion of patients with chronic diseases was greater in the native Turkish group. We found a higher mortality in the immigrant group. The mortality of patients with infectious disease was also higher in the immigrant group.
A study by Lopez et al. did not detect significant variation in paediatric intensive care therapies and outcomes by race.8 On the other hand, other authors have reported differences in the rate of admission and risk-adjusted mortality in paediatric intensive care patients between patients of different ethnicities.9 While a study by Büyüktiryaki et al. found an overall higher mortality in newborns of Syrian refugees compared to newborns of Turkish descent, a more recent study did not find a statistically significant difference.10,11 To our knowledge, there is no published data on differences in mortality in the paediatric intensive care setting in Turkey after the start of the Syrian civil war. When we compared the crude death rate in immigrant children versus children of Turkish descent in our 49-bed paediatric intensive care unit, we found a higher mortality in the immigrant group, despite there being no significant differences in the disease severity scores at admission.
The war in Syria started 8 years ago, and the mean age of the patients in our study group was 39.50 ± 66.05 months, meaning the vast majority of these patients had been born in Turkey and resided in Turkey their entire lives, and that none of them had been admitted due to traumatic injury incurred in a war zone or combat injuries. Nevertheless, while most of these immigrant children were not born in their country of origin and are not widely affected as a group by trauma or chemical exposure, they should still be considered a specific population because they share a common background from a genetics standpoint. On one hand, the Turkish population in Southeast Turkey and Syrian immigrants are comparable populations that have several factors in common that may have an impact on health status and disease risk in children, such as young maternal age, multiparity and crowded living conditions. However, these populations may differ in their compliance with preventive health care measures. It is not uncommon for refugees to initially have difficulty understanding or complying with local health care processes.2
In a study conducted simultaneously in 100 patients in our unit, we found that the proportion of children that were missing at least 1 dose of vaccine was greater in immigrant children admitted to the intensive care unit compared to children of Turkish descent (81% vs 48%) (unpublished data). Although this difference was not statistically significant, we wanted to evaluate the proportion of children with infectious diseases in these 2 groups in this study, as severe infectious disease could be the underlying reason for the higher mortality. It is known that secondary infections and complications of infection are common in nonvaccinated patients.12,13
A large proportion of patients in the sample (48.25%) had an infectious disease as the presenting complaint. It would be reasonable to assume that despite having similar disease severity scores at admission, nonvaccinated children would have a more severe and complicated course of disease, which could explain the higher mortality in the immigrant group. The proportion of patients with a community-acquired infectious disease as the presenting complaint was similar in both groups (P = 0.144). These data are consistent with the findings of the study by Turktan et al. an adult patients in the intensive care unit.14 Another finding consistent with their study was that the mortality in the subset of patients with infectious disease was higher in the immigrant group (19.3% vs 9.8%; P = 0.008) in our sample. Of the variables under study, the presence of chronic disease and high PRISM scores could be associated with an increase in mortality. To correct for their potential effect as confounders, we performed regression analysis. The higher mortality in immigrant children with infectious diseases persisted after correcting for the presence of underlying chronic disease and a high PRISM score. This increase in mortality in patients with infectious diseases could account for the higher mortality observed in the immigrant group. The PRISM score in the first 24 h may not reflect the severity of infection, which may explain why the score had a low discriminatory power in patients with community-acquired infections.
Since the crude death rate offers limited information, we calculated the SMR, which is the ratio of the observed mortality to the expected mortality in a given population. The SMR was 0.32 for the total sample, 0.4 for the immigrant group and 0.24 for the native Turkish group. All 3 values were less than 1, indicating that actual mortality was lower than predicted based on the score.
Going back to the effect of serious infections on the discriminatory power of the score, we analysed ROC curves for the subsets of patients whose presenting complaint was acute infection. We found a very low specificity in both immigrant and native Turkish patients with acute infections, with AUCs of less than 0.75. This indicates that the discriminatory power of the score is poor in nearly half of each of the 2 groups. While this could indirectly explain differences in mortality despite similar scores, it is an important finding that should be analysed in other patient populations in Turkey and in the assessment of the performance of any score, as infectious diseases are common in critically ill paediatric patients.15 Nearly all severity scores have limitations, and using more than one score could be useful for the purpose of minimising such drawbacks. The possibility of adding infection-related variables to scores for application in the specific population under study should also be evaluated. Regression analysis should also be used to study whether incomplete vaccination is an independent risk factor for infection severity and mortality in these patients and whether it should be included as a variable in future scores.
In a study that analysed the SMR calculated using the PIM2 score, Tritschler et al. found no differences in illness severity, PICU outcomes and the primary diagnosis between immigrant children and the general population admitted to the paediatric intensive care unit.7 However, neither this study nor the Lopez study compared subgroups based on the primary diagnosis.5,7
Our finding of a higher prevalence of underlying chronic diseases in Turkish children should be assessed further and nationwide. The current evidence shows that mortality is higher in children with comorbidities.16 Yet despite a lower prevalence of chronic diseases in the immigrant group in our study, the mortality was higher in this group. This could indicate that many underlying diseases may be underdiagnosed and undertreated in immigrants, but we were not able to explore this hypothesis in this study because autopsies were not performed. Before drawing conclusions, this finding and the significantly greater proportion of male patients in the immigrant population should be further investigated at the national level to characterise the care-seeking behaviour in these two seperate populations.
In summary, immigrant children in paediatric intensive care units are a unique population not only because they have a different genetic background, but also because they are exposed to different environmental factors compared to children residing in their country of origin. It is important to take this into account, as disease severity scores that can be used reliably in the native population may not be informative in immigrant children. In addition to the usual demographic and clinical data, whether the child has a community-acquired infection has an impact in the prognosis and outcome of these patients. More studies are needed to establish the impact of infectious diseases and other relevant factors on the severity scores used in receiving countries.
Please cite this article as: Yetimakman AF, Kiral E. Una población única en la Unidad de Cuidados Intensivos Pediátricos de la actualidad: niños inmigrantes que presentan enfermedades infecciosas. An Pediatr (Barc). 2021;94:4–10.