Drug resistance is an additional difficulty in the diagnosis and treatment of tuberculosis (TB). A rate of isoniazid (H) resistance of up to 9.6% has been reported in children in Spain.1 We present data on an outbreak of isoniazid-resistant TB, with emphasis on contact tracing and the diagnostic and treatment characteristics of paediatric cases.
The index case was a man aged 39 years with active laryngeal TB and pulmonary cavitation that cared for children in an apartment block. He was isolated in the hospital from the moment of diagnosis and treated with H, rifampicin (R), pyrazinamide (Z) and ethambutol (E). Seven weeks later, resistance to H was confirmed (S315T mutation in the katG gene), so H was discontinued and streptomycin (S) and moxifloxacin added to the regimen. The patient suffered a tendon rupture that led to discontinuation of moxifloxacin, and eventually completed 12 months of treatment.
The contact tracing involved performance of a tuberculin skin test (TST) that was repeated 2 months later in individuals with indurations of less than 5mm. Children aged up to 14 years underwent a QuantiFERON® test (Cellestis, Victoria, Australia) and chest radiograph (CXR). Contacts with a TST induration of 5mm or greater and normal CXR underwent ultrasound examination of the mediastinum to assess for potential lymphadenopathies not visible in CXR. Lymph nodes greater than 1cm considered abnormal.
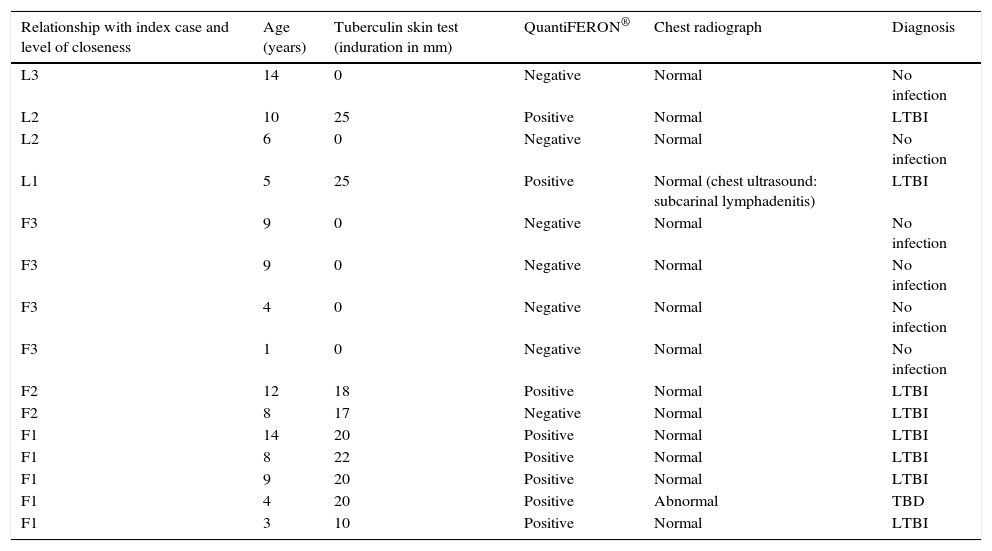
The investigation comprehended 16 adults and 15 children. None of the contacts were immigrants or had been vaccinated with BCG. Six children had indurations of 0mm (Table 1) and were treated with H for primary chemoprophylaxis until the second TST, and this was negative in all of them.
Epidemiologic, clinical and radiologic data for the children under study.
| Relationship with index case and level of closeness | Age (years) | Tuberculin skin test (induration in mm) | QuantiFERON® | Chest radiograph | Diagnosis |
|---|---|---|---|---|---|
| L3 | 14 | 0 | Negative | Normal | No infection |
| L2 | 10 | 25 | Positive | Normal | LTBI |
| L2 | 6 | 0 | Negative | Normal | No infection |
| L1 | 5 | 25 | Positive | Normal (chest ultrasound: subcarinal lymphadenitis) | LTBI |
| F3 | 9 | 0 | Negative | Normal | No infection |
| F3 | 9 | 0 | Negative | Normal | No infection |
| F3 | 4 | 0 | Negative | Normal | No infection |
| F3 | 1 | 0 | Negative | Normal | No infection |
| F2 | 12 | 18 | Positive | Normal | LTBI |
| F2 | 8 | 17 | Negative | Normal | LTBI |
| F1 | 14 | 20 | Positive | Normal | LTBI |
| F1 | 8 | 22 | Positive | Normal | LTBI |
| F1 | 9 | 20 | Positive | Normal | LTBI |
| F1 | 4 | 20 | Positive | Abnormal | TBD |
| F1 | 3 | 10 | Positive | Normal | LTBI |
F, family; L, leisure; 1, close contact (more than 6h a day); 2, daily contact (fewer than 6h a day); 3, occasional contact (not daily).
Eight children with an induration of 5mm or greater and a normal chest CXR received a diagnosis of latent tuberculosis infection (LTBI) and started HR treatment until resistance to H became known, eventually completing 6 months of R (6 R). One of them presented with subcarinal adenopathies of 2.3cm in diameter on mediastinal ultrasound examination, but received a diagnosis of and treatment for LTBI per this study protocol. This patient remained asymptomatic and the lymphadenopathy was no longer visible on ultrasound after 4 months of treatment. One girl developed asymptomatic hypertransaminasaemia, which resolved with the discontinuation of treatment followed by its gradual reintroduction. One adolescent did not adhere to treatment repeatedly, and eventually completed 5 R.
The QuantiFERON® test was negative in children without infection and positive in children with LTBI, except for 1 girl aged 8 years with an induration of 17mm in the TST and close contact with the index case.
One boy aged 4 years with an induration of 20mm and adenopathies on CXR received a diagnosis of tuberculosis disease (TBD) and started treatment with HRZE. His samples were negative, and after H resistance in the source case became known, completed 6 RZE. He was followed up at the clinic one year after he finished the treatment.
Of the adults that were investigated, 10 had a positive result in the initial TST and 1 more had a positive result in the second test. All had normal CXR, received a diagnosis of LTBI and were treated with a 4 R regimen.
The rate of isoniazid resistance in Spain is greater than 4%, so induction treatment of TBD should include 4 drugs unless it is known that the strain is sensitive to H.2 The recommended regimes for isoniazid resistant TB are 6–9 RZE, 2 RZES/7 RE or 2 RZE/7–10 RE, with the possible addition of a quinolone the first 2 months.3,4 The boy with TBD in our study started treatment with 4 drugs and only completed 6 months of RZE, since Z was used throughout the treatment and due to the low bacillary population in the patient.
In our unit, we use the 3 HR regimen for LTBI, which shortens the duration of treatment, improves adherence and covers the possibility of H resistance from the beginning of treatment. Cases with documented resistance to H require a 4–6 R regimen.3,5
Six children were treated ineffectively with H for primary prophylaxis, as the resistance to H was unknown at the time, but fortunately the results of the second TST were negative in all.
The delay in the diagnosis of drug resistance was 7 weeks. The GenoType MTBDRplus® (Hains Life Science, Nehren, Germany) is a rapid assay that can be used to identify most of the mutations that confer resistance to R (rpoB) or H (inhA and katG), facilitating the early detection of resistance.
The agreement of the QuantiFERON® test with the TST for the diagnosis of LTBI was good, although there was 1 false negative result with QuantiFERON®. This technique can help diagnose LTBI, especially in patients that have received BCG vaccination or with immunosuppression, although it should not be used as a substitute for the TST.
The asymptomatic patient with an induration of 23mm in the TST and a normal CXR with evidence of adenopathies on mediastinal ultrasound was classified and treated as a case of LTBI as opposed to TBD in our study, with a favourable outcome in sonographic followup. Lymphadenopathies that can only be detected by computed tomography or ultrasound in asymptomatic children do not seem to be specific of tuberculosis disease.6
Please cite this article as: Ruíz de Zárate B, Gomez-Pastrana D, Pérez-Escolano E, Aragón Fernández C, López Prieto MD. Descripción de un brote de tuberculosis resistente a isoniacida en una comunidad de vecinos. An Pediatr (Barc). 2017;87:292–293.