The results are presented on the “current situation of the organisation, resources and activity in paediatric cardiology in Spain”. It was promoted by the Spanish Society of Paediatric Cardiology and Congenital Heart disease.
Material and methodsAn analysis was carried out on the results obtained from a specifically designed questionnaire, prepared by the Spanish Society of Paediatric Cardiology and Congenital Heart disease, that was sent to all hospitals around the country that offer the speciality of paediatric cardiology.
ResultsA total of 86 questionnaires were obtained, including 14 hospitals that perform cardiac surgery on children. A total of 190 paediatric cardiology consultants, 40 cardiac surgeons, and 27 middle grade doctors performing their paediatric residency (MIR programme) were identified. All hospitals had adequate equipment to perform an optimal initial evaluation of any child with a possible cardiac abnormality, but only tertiary centres could perform complex diagnostic procedures, interventional cardiology, and cardiac surgery. In almost all units around the country, paediatric cardiology consultants were responsible for outpatient clinics and hospital admissions, whereas foetal cardiology units were still mainly managed by obstetricians. The number of diagnostic and therapeutic procedures was similar to those reported in the first survey, except for a slight decrease in the total number of closed cardiac surgery procedures, and a proportional increase in the number of therapeutic catheterisations.
ConclusionsPaediatric Cardiology in Spain is performed by paediatric cardiology consultants that were trained initially as general paediatricians, and then completed a paediatric cardiology training period. Almost all units have adequate means for diagnosis and treatment. Efforts should be directed to create a national registry that would not only allow a prospective quantification of diagnostic and therapeutic procedures, but also focus on their clinical outcomes.
Presentamos el trabajo «situación actual de la organización, recursos y actividad en cardiología pediátrica en España», promovido por la Sociedad Española de Cardiología Pediátrica y Cardiopatía Congénitas.
Material y métodosEl estudio se elaboró con los resultados obtenidos de un cuestionario elaborado por la Sociedad Española de Cardiología Pediátrica y Cardiopatía Congénitas, remitido a todos los hospitales del territorio nacional con actividad en cardiología pediátrica.
ResultadosOchenta y seis respondieron el cuestionario, 14 de los cuales disponen de cirugía cardíaca infantil. Los recursos humanos incluyen 190 médicos, 40 cirujanos y 27 MIR. Todos los hospitales disponen de material para el diagnóstico inicial adecuado, y solo los hospitales terciarios disponen de técnicas de diagnóstico específico, cardiología intervencionista y cirugía cardíaca. La atención a los pacientes, en consultas externas y en la hospitalización es realizada o supervisada mayoritariamente por cardiólogos pediátricos. Existe diversidad en los profesionales que realizan las ecocardiografías fetales, ya que en un porcentaje considerable de hospitales sigue siendo realizada en exclusiva por los obstetras. El número de procedimientos diagnósticos y terapéuticos fueron similares al registro previo, con un leve descenso de cirugía cardíaca cerrada y un aumento proporcional de cateterismos terapéuticos.
ConclusionesLa cardiología pediátrica en España es realizada por pediatras con formación en cardiología pediátrica mayoritariamente. La mayoría de los centros disponen de medios adecuados de diagnóstico, y solo los hospitales terciarios cuentan con técnicas de diagnóstico específico, cardiología intervencionista y cirugía cardíaca. En futuros estudios, debemos no únicamente cuantificar las técnicas de diagnóstico y tratamiento sino también, aspirar a la cuantificación de resultados clínicos.
Since the introduction of the medical intern residency programme (MIR) in Spain in the 1970s, paediatrics has experienced an enormous advance that has inevitably led to the emergence of paediatric specialties.1 In our country, paediatric cardiology has developed progressively from the opening of the first units in the La Paz, Ramón y Cajal and Vall d’Hebron hospitals, with the creation of multiple tertiary care cardiology units nationwide in the 1990s.2 In recent years, the major diagnostic methods that have emerged in the field of cardiology (magnetic resonance imaging [MRI], three-dimensional echocardiography [3D echo], high resolution computed tomography [HRCT], positron emission tomography [PET] and single-photon emission computed tomography [SPECT]) have been integrated in patient care and broadened the scope of the specialty, which now runs the whole gamut from foetal diagnosis to the care of adolescent and adult patients with congenital heart defects.3 All of the above, combined with the substantial improvement of surgical and percutaneous techniques, has achieved a survival rate in paediatric cardiac patients of more than 85%, with many living into adulthood, giving rise to new challenges in the care of this new and complex population.
Paediatric specialties are now an established reality in the United States and most of the European Union, but they have not been recognised officially in Spain.4,5 In 2001, the Sociedad Española de Cardiología Pediátrica y Cardiopatías Congénitas (Spanish Society of Paediatric Cardiology and Congenital Heart Disease, SECPCC) branched out from the Asociación Española de Pediatría (Spanish Association of Padiatrics) and the Sociedad Española de Cardiología (Spanish Society of Cardiology) with the aim of bringing together health professionals involved in the diagnosis and treatment of paediatric heart disease in general and congenital heart defects in particular. One of the first tasks tackled by the SECPCC was to collect data on the organisational structure and resources in this specialty, as the data available at the time the society was created dated from 1979.6 The SECPCC conducted the first survey of the organisation and resources in this specialty in 2003 and published its results in 2005.7 Given the continuous development and changes in the specialty, it seemed necessary to collect updated data to obtain an overall perspective of the care provided to patients with heart disease from intrauterine life to adulthood.8
Materials and methodsFor the purpose of data collection, we sent out a questionnaire in the first semester of 2014 to all hospitals offering paediatric care in each autonomous community in Spain, both public and private. The data were collected by one or more representatives in each autonomous community and subsequently processed in the second semester of 2014 by the Working Group on Clinical Cardiology and Registers of the SECPCC.
The questionnaire collected data for 2013 and was divided into several sections: the first one devoted to the type of facility, method of data collection and organisational structure in relation to paediatric cardiology, the second to the available human and material resources, the third one to the specific training and allocation of the health professionals involved in care delivery, and the fourth one to quantitative data regarding the care delivered (admissions, appointments in outpatient clinics, diagnostic tests and interventions, cardiac catheterization).
To compare data, we considered the following hospital categories: (a) hospitals offering medical–surgical care (MSC), (b) regional hospitals that did not offer MSC (at the autonomous community level or involving more than 1 province), (c) hospitals not offering MSC of less than regional scope (at the province or county level).
ResultsWe received correctly completed questionnaires from 86 hospitals, including 14 of the 17 offering MSC in Spain. Ninety-six percent of participating hospitals were public. The total number of children's hospitals that offer some type of paediatric cardiology care is unknown, but our survey collected data for those with a significant activity in the field. Table 1 presents the distribution of responses by hospital category. The information to fill out the questionnaire was retrieved from hospital administrative records in 43% cases. When such records were not available, the individuals responsible for care delivery provided estimated data.
Distribution of responses in the hospital survey by established categories of hospital.
| Hospitals with medical–surgical activity | Regional hospitals (not offering surgery) | Rest of hospitals | Total hospitals | |
|---|---|---|---|---|
| Total number of hospitals invited to participate | 17 | 15 | 77 | 109 |
| Total responses received | 14 | 12 | 60 | 86 |
| Percentage of participating hospitals that responded correctly | 82.3% | 80% | 77.9% | 78.9% |
All hospitals had departments of paediatrics. We counted a total of 47 paediatric cardiology units. All hospitals that offered MSC had paediatric cardiology units, while the percentage with these units dropped to 83.3% in regional hospitals without MSC and to 57.6% in all other hospitals (local referral hospitals without MSC). Our survey identified 14 adult congenital heart disease units: 10 were in hospitals offering MSC and 4 in regional hospitals without MSC. Thus, 5 hospitals offering MSC did not have a specific unit for the care of adult survivors of congenital heart disease (Table 2).
Human resources (Table 3)Based on questionnaire data, we counted a total of 190 medical doctors, 40 surgeons and 27 MIR residents devoted to paediatric cardiology. The mean number of full-time paediatric cardiologists in hospitals with MSC was 5.2. However, the number of paediatric cardiologists fully dedicated to this area of care declined progressively in regional hospitals and then province- or county-level hospitals. Overall, in the group of hospitals without MSC, the mean number of physicians devoted exclusively to paediatric cardiology was of only 0.54 physicians per hospital, as these physicians combined their activity in paediatric cardiology with work in other areas, such as neonatology or general paediatrics (Table 3).
Human resources.
| Hospitals offering surgery (%) | Regional hospitals (%) | Other hospitals (%) | |
|---|---|---|---|
| Paediatric cardiologists | 78 (5) | 18 (3) | 21 (67) |
| Paediatric cardiology resident physicians | 25 | 1 | 1 |
| Surgeons | 40 | 0 | 0 |
In parentheses, number of physicians dedicated part-time to paediatric cardiology, and outside parentheses, number of physicians dedicated full-time to paediatric cardiology.
All participating hospitals had basic resources for diagnosis (laboratory, radiology, electrocardiography and echocardiography). All medical–surgical hospitals and regional hospitals could perform conventional exercise echocardiograms. When it came to imaging tests, all hospitals had the resources to perform computed tomography (CT) scans, and MRI was available at 100% of hospitals offering MSC and most regional and local hospitals without MSC. All medical–surgical hospitals had a coronary care unit, which was exclusively paediatric in 47% of cases; of all regional hospitals, only 25% had such a unit, and it was always shared with adult cardiology services (Table 4).
Material resources.
| Hospitals offering surgery (%) | Regional hospitals (%) | Other hospitals (%) | |
|---|---|---|---|
| General radiology suite | 100% | 100% | 100% |
| Laboratory | 100% | 100% | 100% |
| ECG | 100% | 100% | 100% |
| 2D-Doppler echocardiogram | 100% | 100% | 100% |
| Conventional exercise echocardiogram | 100.00% | 100% | 33% |
| Ergospirometry | 53.30% | 50% | 10% |
| 24-h Holter | 100% | 100% | 91.50% |
| Event monitoring | 53.30% | 50% | 17% |
| Tilt table test | 100.00% | 83.30% | 31.20% |
| CT | 100% | 100% | 84.70% |
| MRI | 100.00% | 91.60% | 79.60% |
| Paediatric coronary care unit | 47% | 0% | 5% |
| Shared coronary care unit | 100% | 25% | 5% |
| Paediatric electrophysiology unit | 6.7 | 0 | 0 |
| Shared electrophysiology unit | 93.30% | 91.60% | 26.60% |
| ECMO | 66.60% | 0% | 0% |
| Ventricular assist device placement | 33.00% | 0% | 0% |
Overall, 66% of hospitals offering MSC had the resources for extracorporeal membrane oxygenation (ECMO) and 1/3 could perform implantation of ventricular assist devices.
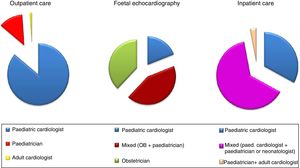
Activity (Table 5)The survey revealed a total of 155840 outpatient visits, of which 42.8% were initial visits. A total of 159334 transthoracic echocardiograms were performed (including those performed at the outpatient, emergency and inpatient levels). Hospitalised patients mainly stayed in the paediatric ward, but nearly 40% required intensive care: neonatal intensive care unit (NICU, 22%) or paediatric intensive care unit (PICU, 17.1%). Inpatient care was always provided by paediatric cardiologists in hospitals with MSC, whereas in all other hospital categories, the care was delivered by a combination of professionals or by general paediatrics teams in up to 22% of cases. Depending on the hospital category, foetal echocardiograms were performed by different professionals (Fig. 1, Table 5).
Activity.
| Total patients | Mean per hospital | Range | % of total | |
|---|---|---|---|---|
| Total visits | 155840 | 1833 | 45–10030 | 100 |
| 1st visit | 62615 | 771 | 25–3000 | 42.8 |
| Successive visits | 89216 | 1049 | 20–7308 | 67.2 |
| TTE | 159334 | 1874 | 1–10129 | 93.4 |
| TEE | 1864 | 22.3 | 0–500 | 6.6 |
| Total admissions | 6886 | 80.0 | 0–1651 | 100 |
| Total ward admissions | 4193 | 53.5 | 0–1119 | 60.9 |
| PICU admissions | 1175 | 19.4 | 0–220 | 17.1 |
| NICU admissions | 1518 | 14.8 | 0–312 | 22.0 |
NICU, neonatal intensive care unit; PICU, paediatric intensive care unit; TEE, transesophageal echocardiogram; TTE, transthoracic echocardiogram.
As for more complex diagnostic and treatment techniques, in the year under study participating hospitals performed 2701 cardiac catheterization procedures, of which slightly more than half (50.8%) were therapeutic, as well as 403 invasive electrophysiology procedures (63.8% of them therapeutic) (Table 6). Relative to the last survey, there has been a significant increase in the frequency of Holter monitoring, heart MRI scans and stress tests, while there has been a decrease in nuclear imaging tests. When it came to circulatory support techniques, in 2013 a total of 60 required ECMO and 4 underwent placement of Berlin Heart ventricular assist devices.
Number of electrophysiology (EP) procedures and cardiac catheterizations performed in 2013.
| Total number | Mean (range) | |
|---|---|---|
| Diagnostic EP procedures | 146 | 1.74 (0–138) |
| Therapeutic EP procedures | 257 | 2.99 (0–47) |
| Adrenaline challenge | 30 | 0.35 (0–20) |
| Flecainide challenge | 60 | 0.71 (0–20) |
| Diagnostic catheterization | 1.329 | 15.82 (0–487) |
| Therapeutic catheterization | 1.372 | 15.95 (0–303) |
There were 1740 heart surgeries, and Table 7 shows their distribution by hospital category. We ought to note that only 2 hospitals performed more than 200 procedures in a year. There were a total of 29 heart transplants.
Frequency distribution of hospitals based on the number of cardiac catheterizations or surgical procedures performed in a year. Comparison of years 2002 and 2013.
| Cardiac catheterizations (n) | 2002 | 2013 |
|---|---|---|
| >150 | 6 | 6 |
| >100 | 4 | 3 |
| >80 | 4 | 1 |
| <65 | 3 | 5 |
| Surgical procedures (n) | 2002 | 2013 |
|---|---|---|
| >200 | 3 | 2 |
| >100 | 7 | 7 |
| >75 | 4 | 1 |
| <65 | 3 | 5 |
Of all patients, 1020 required transfer to a different hospital for evaluation or treatment. Twenty-three percent of hospitals transferred patients to hospitals in other autonomous communities. As expected, hospitals offering MSC transferred very few patients (mean, 1.5 transfers/year) compared to all other hospitals (mean, 15.9 patients/year).
DiscussionOur study contributes data from a large number of hospitals (n = 86), with participation of 48 more hospitals compared to the first survey published in 2002,5 and participation of the majority of hospitals offering medical–surgical care in Spain (14 out of 17). The overall response rate of hospitals offering paediatric cardiology services was 78.9%. According to a recent article, there are 210 hospitals in Spain offering general paediatrics care,9 with a much smaller number offering paediatric specialty care, and while it is possible that some of them offer sporadic paediatric cardiology services, we believe that our data provide a faithful representation of the current status quo of paediatric cardiology in Spain, and that they are more comprehensive compared with the sample obtained in the previous survey.
All hospitals offering MSC and regional hospitals had paediatric cardiology departments or units, while these services were less consistent in all other hospitals, where paediatric cardiology care was provided in combination with or as part of other services, so that most professionals involved in paediatric cardiology care delivered this type of care on a part-time basis, as opposed to medical–surgical or regional hospitals, who had several physicians (a mean of 5.2) fully dedicated to this field. In all of Spain, there were a total of 190 doctors in the field of paediatric cardiology (85 in hospitals with MSC and 105 in other hospitals), as well as 40 surgeons and 27 MIR residents in training, which reflects growth in the field compared to the previous survey.
Resources for the evaluation of congenital heart defects were widely available, and all hospitals in the survey had the essential resources for diagnosis and initial management. More selective resources, such as ECMO, ventricular assist devices or event monitoring were only available in referral hospitals that managed complex cases. In addition, not only large hospitals but nearly all hospitals were adequately equipped to perform specific diagnostic tests such as heart MRI, Holter monitoring or CT.
The most important test in all hospitals was transthoracic echocardiography (available in 100%), and transesophageal echocardiography amounted to only 6% of the total number of echocardiographic exams performed, which was consistent with international guidelines.10
In Spain, care at both the outpatient and inpatient levels was mainly delivered by paediatricians with specific training in paediatric cardiology. At present, there are practically no adult cardiology units left that manage outpatient and inpatient care in children, although we found that 11% of outpatient paediatric cardiology visits were managed by general paediatricians. In almost all instances, inpatient care in the PICU, NICU or paediatric ward involved paediatric cardiologists.
The complexity of the care delivered to cardiac patients is on a different level compared to other diseases, which is reflected by the fact that 40% of the cardiac patients admitted to hospital are admitted to intensive care units, and therefore it is essential that they be managed by qualified professionals.11
We currently face a turning point in foetal echocardiography, as most congenital heart defects can be diagnosed in utero. Thus, the foetal period is becoming increasingly important in paediatric cardiology. However, there is wide variability in the use of this technique between hospital categories, as in hospitals that do not offer MSC nearly 43% of these examinations are performed by obstetricians alone. A greater availability of the equipment and more training on this method could lower this percentage and narrow the gap with medical–surgical hospitals, where only 13% of foetal echocardiograms are performed exclusively by obstetricians. Prenatal diagnosis continues to be an area that needs to be promoted within this subspecialty.
The care provided by specialists in paediatric cardiology to all patients from intrauterine life through adulthood, as currently done in Spain, has achieved a decrease in morbidity and mortality that is reflected in the literature.12
The substantial advances that have taken place in different areas of paediatric cardiology require a specific organisation of these services as well as specialised training of health professionals (physicians and nurses).13 Thus, studies like our own, the survey conducted by the SECPCC in 20037 or the Baby Heart Project of the Italian Society of Paediatric Cardiology14 have contributed to the optimisation of resources and to improved planning in health care systems.
The only diagnostic tests whose frequency declined compared to the previous survey were nuclear medicine tests, which were probably replaced by advances in MRI techniques in recent years.15
When it came to interventional cardiology, we found 7 coronary care units that were exclusively paediatric and 12 shared by both adult and paediatric patients. The number of procedures performed was slightly higher, with the increase mainly corresponding to therapeutic cardiac catheterization, a technique in which there has been considerable progress, and which in some instances has been demonstrated to improve outcomes compared to surgery16 or with the use of hybrid procedures.17 In most hospitals, these procedures were performed by paediatric cardiologists specialised in interventional cardiology.
Electrophysiology procedures were performed in as many as 38 hospitals, in nearly all by adult electrophysiologists, except in 3 hospitals that offered MSC, where the procedures were performed jointly. The total number of electrophysiology procedures performed was 403, of which 257 were therapeutic procedures (Table 6).
These findings reveal that as of 2013, the number of paediatric cardiologists trained in paediatric electrophysiology is significantly smaller compared to the paediatric cardiologists trained in percutaneous techniques. As for surgery, we found a decrease of nearly 50% in the number of closed-heart surgeries and a similar number of surgeries with extracorporeal circulation, while the total number of procedures (including surgery, catheterization and cardiac ablation) was very similar to the total found in the previous survey.
The Spanish territory is broad, encompassing 17 autonomous communities over the Iberian Peninsula, Balearic Islands and Canary Islands, and the autonomous cities of Ceuta and Melilla. In 2013, participating hospitals made 1020 transfers, and 23% needed to transfer patients to other autonomous communities.
When it comes to the number of surgical interventions, previous studies have analysed approaches for the optimisation of resources and their outcomes, demonstrating that costs, morbidity and mortality are all lower in higher-volume hospitals,18–20 although the recommendations regarding the minimum necessary volume varied widely between the studies we reviewed. In the United States, hospitals are considered high-volume if they perform more than 400 heart surgeries a year, medium-volume if they perform between 200 and 400 surgeries and low-volume if they perform fewer than 200 heart surgeries a year,21 which means that nearly all units in Spain would be considered low-volume and only 2 medium-volume. In Europe, the standards are somewhat different, and the recommendation is performance of more than 100 procedures a year (75 with extracorporeal circulation).22 In our survey, we found a slight increase in the number of very-low-volume hospitals that performed fewer than 65 procedures, which could have an impact on patient care (Table 7).
An indicator of the high quality of the procedures performed in Spain is the frequency of surgeries with ECMO, placement of ventricular assist devices and above all paediatric heart transplantation, with a total of 29 transplantations performed in 2013, the highest in the time series of paediatric transplantation,23 positioning us among the leading countries in paediatric heart transplantation.24,25 We still need to establish nationwide surgical registers, as has been done for adult patients,26 as we only found valuable studies at the health district level27,28 or by hospital surgical groups, but none of national scope. The overall mortality in individuals with congenital heart defects over a 10-year period in a Spanish register was 4.58%, although there was significant variability between specific diseases.27
ConclusionsIn Spain, human and health care resources in the field of paediatric cardiology have been consolidated in the past decade. However, while there is a well-established organisational structure in terms of human and material resources, there is a void at the administrative level, as paediatric cardiology is not officially recognised as a medical subspecialty. Due to this lack of recognition, which the SECPCC has been pursuing for years, it is not possible to formally regulate the core competencies that must be included in medical training or required for teaching. Our study indicates that overall, the care delivered to paediatric patients is structured correctly, although there is a dearth of paediatric cardiologists with specific training in foetal echocardiography, paediatric electrophysiology and the care of adult patients with congenital heart disease, areas in which, in some cases, care may be delivered by professionals without specific training on congenital heart defects.
Although our survey found evidence that hospitals had material and human resources that were adequate for the level of care they offered, it did not contribute any data on the clinical outcomes of the care delivered to patients with congenital heart disease from intrauterine life to adulthood throughout Spain.
Our study consisted of a survey of hospitals for collection of data that in some instances were estimated. There were 3 hospitals that officially deliver MSC that were not included due to nonresponse (2 fewer compared to the last survey), so we may have underestimated some of the overall results pertaining to surgical activity.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank our colleagues in all participating hospitals for their efforts in data collection.
Please cite this article as: Sánchez Ferrer F, Castro García FJ, Pérez-Lescure Picarzo J, Roses Noguer F, Centeno Malfaz F, Grima Murcia MD, et al. Situación actual de la organización, recursos y actividad en cardiología pediátrica en España. An Pediatr (Barc). 2019;90:94–101.