There are only a limited number of studies on the impact of influenza in the Spanish child population. The present work intends to increase this knowledge by studying some key aspects, such as the incidence of hospital admissions, clinic variables, comorbidities, and the vaccination status in the hospitalised children.
MethodsA retrospective, observational study was conducted by reviewing the medical records of children under 15 years and hospitalised due to community acquired influenza confirmed microbiologically, during 2́flu seasons (2014–2015 and 2015–2016). The study was carried out in 10 hospitals of 6 cities, which represent approximately 12% of the Spanish child population.
ResultsA total of 907 children were admitted to hospital with main diagnosis of influenza infection (447 <2 years), estimating an average annual rate of hospitalization incidence of 0.51 cases/1000 children (95% CI, 0.48–0.55). Just under half (45%) of the cases had an underlying disease considered a risk factor for severe influenza, and most (74%) had not been vaccinated. The percentage of children with underlying diseases increased with age, from 26% in children <6 months to 74% in children >10 years. Admission to the PICU was required in 10% (92) of the cases, mainly due to acute respiratory failure.
ConclusionInfluenza continues to be an important cause of hospitalization in the Spanish child population. Children <6 months of age and children with underlying diseases make up the majority (>50%) of the cases. Many of the severe forms of childhood influenza that occur today could be avoided if current vaccination guidelines were met.
La información existente sobre el impacto de la gripe en la población infantil española es escasa. El presente trabajo pretende aumentar este conocimiento estudiando aspectos clave como la incidencia de hospitalización, clínica, comorbilidades y el estado vacunal en los niños hospitalizados.
MétodosEstudio retrospectivo, observacional, por revisión de historias clínicas, en menores de 15 años hospitalizados por gripe adquirida en la comunidad, confirmada microbiológicamente, durante 2temporadas gripales (2014-2015 y 2015-2016). El estudio se realizó en 10 hospitales de 6 ciudades, que atienden aproximadamente al 12% de la población infantil española.
ResultadosFueron hospitalizados 907 niños con diagnóstico principal de gripe (447<2 años), con una tasa media anual de incidencia de hospitalización de 0,51 casos/1.000 niños (IC del 95% 0,48-0,55). El 45% presentó enfermedades subyacentes consideradas factores de riesgo para gripe grave, y la mayor parte de ellos (74%) no habían sido vacunados. El porcentaje con enfermedades subyacentes aumentó con la edad, desde el 26% en menores de 6 meses al 74% en mayores de 10 años. El 10% de los casos (n=92) precisaron cuidados intensivos pediátricos por fallo respiratorio agudo.
ConclusiónLa gripe es causa importante de hospitalización en la población infantil española. Los menores de 6 meses de edad y los niños con enfermedades subyacentes constituyen una parte mayoritaria (> 50%) de los casos. Una gran parte de las formas graves de gripe en población infantil podrían ser evitada si se cumplieran las indicaciones actuales de vacunación.
Viral respiratory infections are the most frequent infectious diseases in infants and children.1 They encompass a broad clinical spectrum, from mild conditions like the common cold to severe diseases that often require inpatient evaluation and treatment, such as infections by respiratory syncytial virus and influenza viruses. The latter constitute a significant health care burden in the paediatric population and entail a substantial use of resources at both the outpatient and the inpatient care level.2–4 At the international level, there is wide variability in the rates of hospitalization reported in the literature, which depend on the country where the study is conducted, the ages of the individuals under study and the methodology used. Most hospital admissions occur in healthy children,5 but there are also well-known risk factors for admission, such as young age (age <6–12 months), membership in specific ethnic groups and underlying chronic disease.6
Few population-based studies have spanned more than 1 flu season. Furthermore, nationwide data for the impact of influenza on hospital admissions in the Spanish paediatric population are not available, although there is partial evidence from regional or small sample-size case series.1,5,7–10 The primary objective of our study was to establish the rate of hospitalization due to influenza in children aged less than 15 years in Spain based on data from 10 tertiary care hospitals. The secondary objectives included assessing the need for paediatric intensive care, the frequency of comorbidities and the history of vaccination against influenza in hospitalised children.
MethodsWe conducted an epidemiological, multicentre, retrospective observational study through the review of health records of children aged less than 15 years admitted with infection by influenza virus in 2 consecutive epidemic seasons (September 15, 2014 to April 15, 2015 and September 15, 2015 to April 15, 2016). We conducted the study in 4 Spanish regions that were geographically distant, including 10 university hospitals): Basque Country (Hospital Universitario [HU] Basurto and HU Donostia), Madrid (HU 12 de Octubre, HU Clínico San Carlos, Hospital General Universitario [HGU] Gregorio Marañón, HU La Paz), Catalonia (HU Germans Trias i Pujol, HU Sant Joan de Déu, HU Vall d’Hebron) and Andalusia (Hospital Regional Universitario [HRU] de Málaga). We collected data on the catchment population of these hospitals and the number of admissions made (excluding surgical and neonatal admissions) in the 2 periods under study.
We included children aged less than 15 years hospitalised for more than 24h with a primary clinical diagnosis of influenza virus infection with microbiological confirmation. We excluded children who had onset 48h or later following admission, as these could be cases of nosocomial infection.
We obtained the lists of patients from the departments of clinical records, preventive medicine and epidemiology or microbiology of participating hospitals. We reviewed all the health records in which the discharge report included as the primary diagnosis (first listed diagnosis) codes 487.0-487-8 of the International Classification of Diseases (ICD) 9th revision, or J09–J18 of the ICD 10th revision, in the databases of participating hospitals, collecting data for several demographic and clinical variables. We entered the previously anonymised data in an online database designed for the purpose that was shared by all participating hospitals, including information on demographic, clinical and treatment variables.
The methods used for detection of influenza A and B viruses in upper respiratory tract secretion samples were commercially available rapid immunochromatographic assays for influenza virus antigens, multiplex real-time PCR (preceded by reverse RNA transcription) or viral culture in MDCK, A549 and LLC-MK2 cell lines using the shell-vial technique.
An external consultant performed the statistical analysis using the R software, without input from any of the researchers.11 We calculated the incidence of hospital admission using the catchment population of the 10 referral hospitals as the denominator, which amounted to 878808 children aged less than 15 years (12.5% of the Spanish population in this age range). Since we were unable to determine the age distribution in every hospital, we calculated the rate of hospitalization for certain age groups (<6 months, 2 years, <5 years) using as denominator a reference population estimated based on the age distribution of the entire Spanish population in 2017.12
The study protocol was approved by the ethics boards of all participating hospitals and submitted to the Agencia Española de Medicamentos y Productos Sanitarios (Spanish Agency of Medicines and Medical Devices, AEMPS). We conducted the study in adherence with the international ethical guidelines for research and clinical studies in humans of the Declaration of Helsinki, the principles of good clinical practice and the guidelines for clinical research of the AEMPS. All collected data were kept confidential and handled in adherence with Decree SAS/3470/2009 and the Law on the Protection of Personal Data.
ResultsWe identified 984 cases of influenza, of which we excluded 77 (8.5%) that we suspected to be nosocomial infections. Thus, the final sample comprised 907 cases, of which 389 (42.9%) occurred in the first flu season and 518 (57.1%) in the second. Of the total cases, 815 (89.9%) corresponded to patients hospitalised in the paediatric ward, and the another 92 (10.1%) to patients that required admission to the paediatric intensive care unit (PICU) at some point. The mean estimated annual rate of hospitalization due to influenza per 1000 children in the reference population for the 2 seasons under study was 0.51 (95% CI, 0.48–0.55), and it varied between regions, going from 0.31 (95% CI, 0.25–0.40) in Andalusia (HRU de Málaga) to 0.36 (95% CI, 0.31–0.43) in Catalonian hospitals, 0.46 (95% CI, 0.35–0.62) in hospitals in the Basque Country and 0.83 (95% CI, 0.73–0.94) in hospitals in Madrid (Table 1). Overall, infection by influenza virus caused 1.60% (95% CI, 1.51–1.71%) of all paediatric admissions during the study period (mean of the 2 seasons), excluding surgical and neonatal admissions.
Rate of hospitalization due to influenza per 1000 children in the catchment population. Distribution by geographical area.
| Geographical area | Population (N)a | Hospital admissions due to influenza (n)b | Rate per 1000 children (95% CI)c | Relative frequency (%)d |
|---|---|---|---|---|
| Madrid | 281380 | 464 | 0.83 (0.73–0.94) | 51.2 |
| Basque Country | 97685 | 90 | 0.46 (0.35–0.62) | 9.9 |
| Barcelona | 400311 | 290 | 0.36 (0.31–0.43) | 32.0 |
| Malaga | 99432 | 63 | 0.31 (0.25–0.40) | 6.9 |
| Total | 878808 | 907 | 0.51 (0.48–0.55) | 100 |
CI, confidence interval (lower bound-upper bound).
Catchment populations of university hospitals used as reference (age<15 years): Madrid (Gregorio Marañón, San Carlos, La Paz and 12 de Octubre); Basque Country (Donostia [San Sebastian] and Basurto [Bilbao]); Barcelona (San Joan de Déu, German Trías i Pujol and Vall d́Hebron); Malaga (Carlos Haya).
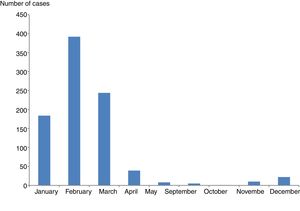
The sex distribution was 508 male (56%) and 399 female (44%), and the mean age was 3.2 years (median, 2 years), with 49.3% aged less than 2 years and 77.6% aged less than 5 (Table 2). The annual rate of hospitalization decreased with age, with an estimated rate of 3.48/1000 children aged less than 6 months (95% CI, 2.82–4.26), of 2.14 in children aged less than 24 months (95% CI, 1.88–2.44), 1.31 in children aged less than 60 months (95% CI, 1.18–1.45) and 0.17 in children aged 5–15 years (95% CI, 0.14–0.20). Hospital admissions were most frequent between January and March (90%) (Fig. 1).
Patients admitted with community-acquired influenza. Estimated age distribution and incidence by age group.
| Age | Absolute frequency | Percentage (95% CI) | Reference populationa | Mean annual incidence (95% CI) |
|---|---|---|---|---|
| <6 months | 178 | 19.6 (17.2–22.3) | 3.48 (2.82–4.26) | |
| 6–24 months | 269 | 29.7 (26.8–32.7) | 78840 | 1.71 (1.45–2.03) |
| >24 months to <60 months | 257 | 28.3 (25.5–31.4) | 165249 | 0.78 (0.65–0.92) |
| 5 years to <10 years | 135 | 14.9 (12.7–17.4) | 308437 | 0.22 (0.17–0.28) |
| 10 to <15 years | 68 | 7.5 (6.0–9.4) | 300570 | 0.11 (0.08–0.16) |
| <24 months | 447 | 49.3 (46.0–52.5) | 104551 | 2.14 (1.88–2.44) |
| <60 months | 704 | 77.6 (74.8–80.2) | 269800 | 1.31 (1.18–1.45) |
| Total | 907 | 100 | 878808 | 0.51 (0.48–0.55) |
CI, confidence interval (lower bound-upper bound).
Most of the patients were admitted due to respiratory symptoms (wheezing, bronchiolitis, pneumonia/bronchopneumonia), documented in 492 cases (54.2%) and fever without a focus, documented in 256 (28.2%). The working diagnosis was suspected sepsis in 27 cases (3.3%) and encephalitis in 10 (1.1%) (Table 3). Of all patients, 409 (45.1%) had comorbidities or underlying disease, with a single such problem in 288 cases and more than 1 in 121. The most frequent comorbidities were moderate or severe asthma and associated conditions, documented in 140 patients (15.4%), followed by immunosuppression in 88 cases (9.7%), preterm birth in 84 (9.3%) and congenital heart disease in 81 (8.9%). Other frequent comorbidities were chronic encephalopathy (61 cases; 6.7%), neuromuscular disorders (29 cases; 3.2%), chromosome disorders (21 cases, 2.3%), upper gastrointestinal tract malformation (21 cases, 2.3%) and bronchopulmonary dysplasia (20 cases, 2.2%). Of the 716 patients, 36 (5%) were overweight, with a weight below the 95th percentile. The mean weight of admitted children. The mean weight of admitted children was 14.7±11.34kg (range, 2.5–98), corresponding to a mean percentile of 37±30.
Reason for admission in the 907 children hospitalised due to community-acquired influenza.
| Absolute frequency | Percentage (95% CI) | |
|---|---|---|
| Fever and dyspnoea | 295 | 32.5 (29.6–35.6) |
| Fever without a focus | 256 | 28.2 (25.4–31.2) |
| Fever and vomiting/diarrhoea | 93 | 10.3 (8.4–12.4) |
| Pneumonia/bronchopneumonia | 109 | 12.0 (10.1–14.3) |
| Acute respiratory disease | 125 | 13.8 (11.7–16.2) |
| Bronchiolitis with wheezing | 51 | 5.6 (4.3–7.3) |
| Bronchiolitis | 44 | 4.8 (3.6–6.5) |
| Bronchitis | 39 | 4.3 (3.2–5.8) |
| Laryngitis/tracheitis | 28 | 3.1 (2.1–4.4) |
| Suspected sepsis | 27 | 3.0 (2.0–4.3) |
| Seizure | 65 | 7.2 (5.7–9.0) |
| Encephalitis | 10 | 1.1 (0.6–2.0) |
| Miscellaneous | 14 | 1.5 (0.9–2.6) |
CI, confidence interval (lower bound-upper bound).
Main reason for admission. There were cases with more than 1 diagnosis at admission.
We were able to obtain information on the vaccination history of 301 patients aged more than 6 months (41.3%). Of the 143 children in the group that had one or more chronic diseases in whom vaccination was indicated (due to chronic respiratory disease [44.3%], immunosuppression [24.5%], neuromuscular disease [19.8%], preterm birth before 37 weeks’ gestation [18.9%], cardiovascular disease or congenital heart defects [12.6%]), only 37 (25.9%) had been vaccinated (Table 4 details the most frequent comorbidities in the 106 children that had not been vaccinated). On the other hand, 145 children had received antibiotherapy prior to admission, and 18 antiviral medication, of who 8 had a relevant history of disease: immunosuppression (n=5), preterm birth (n=3), bronchopulmonary dysplasia (n=1), bronchiolitis obliterans (n=1) and severe asthma (n=1).
Most frequent comorbidities in children aged more than 6 months that were not vaccinated against influenza (n=106).
| Disease | Absolute frequency | Percentage (95% CI) |
|---|---|---|
| Moderate/severe asthma | 40 | 37.7 (29.1–47.3) |
| Immunosuppression | 26 | 24.5 (17.3–33.5) |
| Preterm birth | 20 | 18.9 (12.6–27.3) |
| Encephalopathy | 16 | 15.1 (9.5–23.1) |
| Cardiovascular | 13 | 12.2 (7.3–19.9) |
Other: bronchopulmonary dysplasia (4), sickle-cell anaemia (3), cystic fibrosis (2), upper gastrointestinal tract malformation (2), diabetes mellitus type 1 (1) and chromosome disorder (1).
In 626 patients (68.0%), the causative agent was influenza A virus, which predominated in both seasons, while influenza B virus was involved in another 278 (30.7%), while the type was unknown in 3 cases (Table 5). In 634 children, sterile samples were collected for bacterial culture (blood, cerebrospinal fluid, etc.), resulting in isolation of pathogens in 15 cases (2.4%): Streptococcus pneumoniae in 9 cases, Streptococcus pyogenes in 4 and Staphylococcus aureus in 2.
Detection of influenza viruses for each season under study.
| Virus | Season 1 n (%) | Season 2 n (%) | Total |
|---|---|---|---|
| Influenza A | 282 (72.5)a | 344 (66.4)a | 626 |
| Influenza B | 104 (26.7) | 174 (33.6) | 278 |
| Undetermined type | 3 (0.7) | 0 (0.0) | 3 |
| Total | 389 | 518 | 907 |
Subtype analyses were performed for 90 samples in the first season (31.9%), of which 57 corresponded to subtype H3N2 (63.3%) and 33 to the 2009 pandemic H1N1 subtype (36.7%). Subtype analyses were performed in 100 samples in the second season (29.1%), of which 11 corresponded to subtype H3N2 (11%) and 89 to the 2009 pandemic H1N1 subtype (89%).
Ninety-two children (10.1%) required admission to the PICU, and the most frequent reasons for it were: acute respiratory failure or apnoea in 73 (79.3%); seizures in 9 (9.8%); heart failure in 6 (6.5%), and decreased level of consciousness in 4 (4.3%). Of the patients admitted to the PICU, 59% had some type of chronic disease, and patients with chronic disease were more likely to require intensive supportive care (OR=1.84 [95% CI, 1.19–2.85]; P=.008). In the hospitalised group, the proportion of children with underlying disease increased with age, ranging from 26.4% in infants aged less than 6 months to 73.5% in children aged more than 10 years (χ2=45.7; P<.001) (Table 6). The percentage of children with influenza that needed supportive care in the PICU ranged between 9.7% and 14.7% depending on the age group, except for children aged 5 to less than 10 years, in whom it was 3.7% (χ2=7.26; P=.007).
Association between age of hospitalised children, admission to PICU and presence of chronic disease.
| Age group | Hospitalised, n | Chronic disease, n (%) | Admitted to PICU, n (%) | Chronic disease, n (%) |
|---|---|---|---|---|
| <6 months | 178 | 47 (26.4) | 23 (12.9) | 15 (65.2) |
| 6 to <24 months | 269 | 105 (39.0) | 29 (11.8) | 15 (51.7) |
| 2 to <5 years | 257 | 132 (51.4) | 25 (9.7) | 15 (60.0) |
| 5 to <10 years | 135 | 75 (55.5) | 5 (3.7) | 4 (80.0) |
| ≥10 years | 68 | 50 (73.5) | 10 (14.7) | 5 (50.0) |
| Total | 907 | 409 (45.1) | 92 (10.1) | 54 (58.7) |
The mean length of stay was 6.76 days, with the cumulative stay amounting to a total of 7010 inpatient days, of which 6129 days corresponded to the general paediatrics ward and 881 days to the PICU. During their hospitalization, 524 children were treated with oseltamivir (57.8%) and 488 with antibiotics (53.8%). In addition, 311 received bronchodilators (34.3%), 225 corticosteroids (24.8%) and 412 oxygen therapy (45.4%). There were no deaths among the children included in the study, and none exhibited sequelae associated with the influenza infection at the time of discharge.
DiscussionWe conducted this study in 10 tertiary care hospitals in 6 cities in 4 different geographical areas that were distant from each other, which together served a total population of nearly 900000 children aged less than 15 years, slightly more than 10% of the Spanish population in this age range. For all the above reasons, we expect that our findings may be generalizable to the entire paediatric population of Spain.
Overall, the mean annual rate of hospitalization due to community-acquired influenza in the 2014–2015 and 2015–2016 seasons was high (0.51/1000 children <15 years; 95% CI, 0.48–0.55), and consistent with the findings of longitudinal studies conducted in developed countries in children aged 0–15 or 17 years: 0.70/1000 in the United States (Philadelphia, 2000–2004)13; 0.67/1000 in Germany (Kiel, 1996–2001)14; 0.36/1000 in a study with a 16-year follow-up in Finland (Turku, 1988–2004)15; 0.22–0.24/1000 in another long-term study in Sweden (Stockholm, 1998–2014)16 and the rate estimated in a nationwide study conducted in Canada (2003–2014), of 0.15/1000.17 Nearly half of the hospitalised patients in our study were aged less than 2 years. In fact, the rate of hospitalization decreased drastically with age, with the rate in infants aged less than 6 months being twice that in children aged 6–24 months, 4-fold that in children aged 2–5 years, 20-fold that in children aged 5–10 years and 32-fold that in children aged 10–15 years, which was consistent with the previous literature.5,13,17–19 It is well known that in infants and young children, fever without a focus and sepsis-like presentations are frequent manifestations of influenza that prompt hospitalization for the main purpose of ruling out bacterial infection.5,20–22 The rate in infants aged less than 6 months (3.48/1000 [95% CI, 2.82–4.26]) was similar to the rates found in Finland (2.76/1000 [95% CI, 2.20–3.36]) (1988–2004),15 Sweden (1.44/1000 [95% CI, 0.69–3.31]) (1998–2014)16 or the United States in the pre-pandemic period (2000–2009), with annual rates between 1.6 and 9.1/1000 (studies conducted in 3 cities).19,23,24
In children aged less than 5 years, the rate found in our study (1.31/1000 [95% CI, 1.18–1.45]) was somewhat higher compared to those reported by other authors of studies conducted in European countries such as Spain, Germany or Finland (0.9–1.23/1000),7,14,15 or in the United States (0.9/1000 in 2000–2004 and 0.58/1000 in 2004–2009).19,23 Regardless of the variability found in the literature, the studies we reviewed evince a substantial burden of influenza in paediatric services at different levels of care.
A constant feature in all case series was the identification among children hospitalised due to influenza of a subset with underlying chronic diseases that are considered risk factors for severe or complicated influenza and who accounted for an important proportion of the total cases (between 25% and 49%),8,13,21,25,26 which was 45% in our study. The comorbidities detected in our study were those expected based on past evidence,8,13,27 chiefly asthma and chronic respiratory diseases, followed by immunosuppression, neurologic or neuromuscular diseases, congenital heart defects and preterm birth.
We also ought to mention that we excluded 77 cases where we believed the infection had been contracted in the hospital, a finding that reinforces the need for yearly vaccination of all health care staff to reduce the incidence of these events.
An aspect that has not been studied frequently is the need for paediatric intensive care in children hospitalised with influenza. In our study, 10% of admitted children required this type of care, most frequently due to respiratory failure, and this proportion fell approximately in the middle of the range of the proportions reported in studies conducted in other countries (5–19%),8,13,15,16,21,23 which shows that the course of disease can be severe. In Spain, during the 2009 pandemic and in the first season that followed, Hernández-Bou et al.28 and Launes et al.26 found proportions of PICU admission of 17.5% (n=54) in patients aged less than 14 years and 14% (n=20) in patients aged 6 months to 18 years, respectively. As was the case in our study, the previous literature has also described a greater need for intensive care in children with underlying chronic diseases, which are considered risk factors for severe or complicated influenza.8,13,21 In fact, 59% of the children admitted to the PICU in our study had underlying chronic diseases, and this percentage was even higher, of 77%, in a recent study conducted in 24 German PICUs (2010–2013).27
Despite the significant impact of influenza in the paediatric population in terms of hospitalization, we ought to note that of the 301 patients aged more than 6 months for whom we could obtain data regarding vaccination (the flu vaccine can be administered starting at age 6 months) a significant percentage (35.2%, n=106) corresponded to children with risk factors for severe disease that had not been vaccinated and in whom vaccination was indicated. This finding, which corroborates previous results in Spain,8,10,26 suggests that the impact of influenza on the Spanish paediatric population could be reduced significantly by adhering to current vaccination recommendations. Infants aged less than 6 months also amounted to a substantial proportion of the total admissions (20%), which highlights the need to recommend universal vaccination during pregnancy, a measure that would prevent at least a portion of these infections29 and has been specifically recommended by the World Health Organization in 2012, in addition to advising parents to adopt additional precautions to prevent infection in infants, such as vaccination of household members or avoiding exposure of the infant to individuals with respiratory infections or fever.21
There are some limitations to this study, so its results should be interpreted with caution. First of all, it has a retrospective design, so we could not explore differences in clinical practice (such as situations where children were not hospitalised) or in the approach to diagnosis (such as the use of virologic testing) between different hospitals. Secondly, the catchment populations of participating hospitals may not be representative of the entire Spanish population, as most of the sample was drawn from predominantly urban areas and from 6 cities in particular. In addition, influenza outbreaks can vary in intensity based on the year, geographical area and age group, among other factors.8,19 In this regard, this study spanned 2 flu seasons (2014–2015 and 2015–2016) with a low-to-moderate incidence of influenza,30 and only covered the usual months of the season, so we may have missed cases occurring outside these intervals. Thus, the incidence results should be considered minimum values.
In conclusion, influenza continues to cause a significant number of paediatric hospitalizations in Spain every year; a substantial proportion of cases (more than 50%) occur in infants aged less than 6 months and in children with underlying disease, in whom the administration of the vaccine against influenza is clearly indicated (in case of infants aged less than 6 months, by vaccination of the mother during pregnancy),31,32 and who clearly must be targeted more intensely by interventions aiming at improving vaccine coverage.
FundingThe study was funded by the Instituto de Investigación Sanitaria Biodonostia (San Sebastian, Spain) as sponsor of the project. Protocol code: HOSPIGRIP16.
Conflicts of interestEGPY, GCE, JAF, EGLL, THSP, MJMP, JTRA, JRC, MMH, JJGG, CRGL, DMP have no conflicts of interest to declare.
The authors of the article want to thank all of the following:
J. Arrizabalaga, director of the Instituto de Investigación Sanitaria Biodonostia (sponsor of the HOSPIGRIP study), and L. Codesido, for the management of the HOSPIGRIP research project.
J. Arístegui, the scientific director, and E.G. Pérez-Yarza, the national coordinator of the HOSPIGRIP study.
All the researchers in the HOSPIGRIP research group.
L.M. Molinero (Alce Ingeniería, Madrid, Spain) for IT support and for conducting the statistical analysis.
J. Aristegui, E. Garrote, A. Larrauri, Hospitals and researchers: Hospital Universitario (HU) Basurto, Bilbao, E.G. Pérez-Yarza, G. Cilla, M. Unsain, HU Donostia, San Sebastian, J. Ruiz Contreras, E. García-Ochoa, J.C. Gordillo, HU 12 de Octubre, Madrid, T. Hernández Sampelayo, R. Rodríguez, F. González, Hospital General Universitario Gregorio Marañón, Madrid, M.J. Mellado, C. Calvo, A. Méndez, J. Bustamante, D. Salas, C. Lacasta, HU La Paz, Madrid, J.T. Ramos, M. Illán, HU San Carlos, Madrid, M. Mendez, M. Barjuan, HU Germans Trias i Pujol, Badalona, J.J. García, S. Urraca, M. Caballero, C. Launes, HU Sant Joan de Déu, Barcelona, C. Rodrigo, A. Fàbregas, R. Esmel, A. Antón, HU Vall d’Hebron, Barcelona, D. Moreno, A.I. Valdivielso, P. Piñero, B. Carazo, Hospital Regional Universitario de Málaga, Malaga
Appendix A lists all the authors of the article.
Please cite this article as: Arístegui Fernández J, González Pérez-Yarza E, Mellado Peña MJ, Rodrigo Gonzalo de Liria C, Hernández Sampelayo T, García García JJ, et al. Hospitalizaciones infantiles asociadas a infección por virus de la gripe en 6 ciudades de España (2014–2016). An Pediatr (Barc). 2019;90:86–93.