The prevalence and the variability of clinical practice in acute bronchiolitis make it a perfect candidate to monitor the proper use of resources. The aim of this study is to analyse the differences in the use of non-recommended resources in the management of bronchiolitis in the Emergency Department, before and after the establishment of a new protocol.
MethodsA retrospective study was conducted on a sample of patients diagnosed with acute bronchiolitis in the Emergency Department of a tertiary hospital, before (December 2014) and after (December 2016) the implementation of a new protocol. A comparison was made on the use of diagnostic tests and treatments in both groups.
ResultsThe analysis included a total of 113 patients with acute bronchiolitis examined in December 2014, and 128 patients in December 2016. The clinical characteristics in both groups were similar. In the post-protocol period, there was a significant decrease in the use of salbutamol, both in the Emergency Department (33.6% vs 19.5%, P<.01) and at discharge (46.7% vs 15.2%, P<.001); adrenaline (12.4% vs 2.4%, P=.002); and nebulised hypertonic saline solution (5.3% vs 0.8%, P=.04). Rapid respiratory syncytial virus (RSV) testing was also decreased (40.7% vs 26.6%, P=.01). This decrease was not associated with an increase in the number of admissions or re-assessments in the Emergency Department.
ConclusionsThe establishment of a new protocol for acute bronchiolitis decreased the use of non-recommended resources, mainly the use of bronchodilators and rapid RSV testing.
La prevalencia y la variabilidad de la práctica clínica en la bronquiolitis aguda la convierten en una candidata perfecta para evaluar la adecuación en el uso de recursos asistenciales. El objetivo de este estudio es comparar la utilización de recursos no recomendados para la atención de pacientes con bronquiolitis en el Servicio de Urgencias, antes y después de la instauración de un nuevo protocolo basado en las recomendaciones actuales.
MétodosEstudio retrospectivo de una muestra de pacientes diagnosticados de bronquiolitis aguda en el Servicio de Urgencias de un hospital terciario y seleccionados mediante aleatorización simple antes (diciembre de 2014) y después (diciembre de 2016) de la instauración de un nuevo protocolo. Se comparó el uso de pruebas diagnósticas y el tratamiento en ambos grupos.
ResultadosSe han comparado 113 pacientes con bronquiolitis aguda atendidos en diciembre de 2014 y 128 en diciembre de 2016. Las características clínicas en ambos grupos eran similares. En el período posprotocolo se observó una disminución significativa en la utilización de salbutamol, tanto en el servicio de urgencias (33,6% vs 19,5%, p<0,01) como al alta (46,7% vs 15,2%, p<0,001); de adrenalina (12,4% vs 2,4%, p=0,002) y de suero salino hipertónico nebulizado (5,3% vs 0,8%, p=0,04). También disminuyó la solicitud de la prueba de detección rápida de VRS (40,7% vs 26,6%, p=0,01). No se produjo un aumento en el número de ingresos o readmisiones en urgencias en las siguientes 72horas.
ConclusionesLa instauración de un nuevo protocolo de bronquiolitis aguda disminuyó la utilización de recursos no recomendados, principalmente el uso de broncodilatadores y de la prueba de detección rápida del VRS.
Acute bronchiolitis (AB) is defined as the first acute episode of respiratory distress with wheezing and crackles, preceded by a clinical picture of viral infection of the upper respiratory airway. It affects children aged less than 24 months and generally exhibits a seasonal pattern. In Spain, the epidemic season ranges from November to March.1 In up to 83% of cases, the causative agent is respiratory syncytial virus (RSV), although coinfection by other viruses is common.2
Most cases of AB are mild and can be treated at the outpatient level. However, between 2% and 3% of children require hospital admission,3 and AB is the leading cause of hospital admission in infants aged less than 12 months.4
The diagnostic tests and treatment recommended in clinical practice have changed in recent years based on the emerging scientific evidence.
Acute bronchiolitis is a clinical diagnosis, and there is no evidence supporting the routine performance of diagnostic tests (complete blood count, acute phase reactants, chest X-ray).5,6 The detection of respiratory viruses in nasopharyngeal samples does not guide the management or predict the outcome of patients with AB.7 Viral detection tests may be indicated during the bronchiolitis season in patients with risk factors presenting with cold-like symptoms to assess the need of inpatient monitoring and in patients with a diagnosis of AB that require hospital admission for the purpose of implementing the necessary isolation measures.
Treatment options beyond guaranteeing adequate hydration and oxygen saturation are quite limited.
The most recent clinical practice guidelines do not recommend many of the treatments that have been used in everyday clinical practice (such as nebulised salbutamol or adrenaline).5,8,9 A systematic Cochrane review10 demonstrated that neither oxygen saturation, the time elapsed to resolution of symptoms or the length of stay improved with administration of nebulised salbutamol. Nebulised adrenaline does not seem to benefit these patients either.11 There is no consensus regarding the use of nebulised hypertonic saline solution (HSS), although its use is generally reserved for hospitalised patients.12,13
Antibiotherapy is not indicated either, as the incidence of bacterial superinfection in children with AB is very low, with a risk of bacteraemia or meningitis of less than 1%.14 Furthermore, their use can cause adverse events and promote the development of microbial drug resistance.2
The prevalence of BA and the variability in its management15 make this disease a perfect candidate for monitoring adequate use of resources in clinical practice in the paediatric emergency department (ED) setting.
The aim of the study was to determine the impact of the updating and dissemination of a new protocol for the treatment of AB on the use of resources that are not indicated in the ED.
Materials and methodsWe performed a retrospective and comparative study of patients that received a diagnosis of AB in the ED selected by simple randomisation during 2 bronchiolitis seasons: before the implementation of the new protocol (December 2014) and after its implementation (December 2016). We obtained the data for the study by reviewing patient health records. Based on the evidence available in the literature, at the time we designed the study about 60% of patients with bronchiolitis in the ED received bronchodilators,15 and similar interventions have succeeded in reducing the use of bronchodilators by 12%16 and 17%.17 To calculate the sample size, we used this 60% value as the estimated proportion, and set the objective of reducing bronchodilator use by 15%, assuming an alpha error of 5% and a beta error of 10%. The estimated sample size was n=114, and we decided to select 130 patients per season to minimise the impact of potential losses.
The AB protocol was debated by the chiefs of each of the departments involved in its implementation in 2015, and was finally updated after obtaining the approval of the health care quality committee of the hospital on November 1, 2016. It was then distributed to all permanent and resident physicians in the hospital in a clinical meeting held at the beginning of the RSV epidemic season and via electronic mail, accompanied by a document with the supporting evidence. The protocol was also available to all clinicians in the hospital intranet. The updated protocol placed particular emphasis on restricting the use of bronchodilators in the ED to cases of severe bronchiolitis that did not improve with supplemental oxygen and on identifying the patients in whom diagnostic tests were actually indicated (Table 1).
Recommendations of the emergency department protocol for the management of acute bronchiolitis (2016).
| Acute bronchiolitis is a clinical diagnosis. Testing for detection of RSV should only be performed in patients with risk factors or in case of hospital admission. |
| Assess severity in all children with AB. |
| Measure the RR and oxygen saturation in all children with AB. |
| Chest X-rays are only indicated if severe complications are suspected, in patients without favourable outcomes or in case of diagnostic uncertainty. |
| Empiric treatment with nebulised salbutamol is only indicated in children aged more than 6 months with severe AB that does not improve with oxygen therapy. |
| Empiric treatment with nebulised adrenaline is only indicated in children aged less than 6 months with severe AB that does not improve with oxygen therapy. |
| Document the effectiveness of the empiric treatment (severity score or clinical judgement of paediatrician) and discontinue treatment if it has not been effective |
| Corticosteroids are not indicated in these patients. |
| Antibiotherapy is not indicated in the absence of evidence of bacterial infection. |
| Oxygen: indicated to decrease the work of breathing in moderate-to-severe AB or when the oxygen saturation is less than 92% for a sustained period. |
AB, acute bronchiolitis; RR, respiratory rate; RSV, respiratory syncytial virus.
- -
Acute bronchiolitis: first acute episode of respiratory distress with wheezing preceded by a cold-like clinical picture of the upper respiratory airway which affects children younger than 24 months of age.
- -
We categorised the severity of AB using the modified Wood-Downes-Ferré (mWDF) scale.18
- -
Risk factors for poor outcome of AB: age<4 weeks, preterm birth before 34 weeks’ gestation, cystic fibrosis, bronchopulmonary dysplasia, heart disease, immunodeficiency, neurologic disease, severe malnutrition.
- -
Children aged less than 24 months with a ED discharge diagnosis of AB.
- -
Patients in which a meticulous review of the health records revealed previous episodes of bronchiolitis, bronchitis or bronchospasm.
We selected clinical variables taking into consideration the quality indicators featured in the literature and for which there are specific recommendations in the protocol of our hospital.
We collected data for the following variables:
- -
Demographic: date of service, age, sex, risk factors for poor outcome of AB.
- -
Clinical: fever, vomiting, food refusal, apnoea, cyanosis, lung auscultation findings, severity of AB (mWDF).
- -
Diagnostic tests: rapid RSV detection test, chest X-rays, blood tests.
- -
Treatment: nebulised salbutamol, nebulised adrenaline, nebulised HSS, corticosteroids, antibiotherapy and supplemental oxygen in the ED; salbutamol inhaled salbutamol and corticosteroids after discharge.
- -
Outcome: fate (home, inpatient ward, PICU), readmission in the following 72h, length of stay in ED.
We have described quantitative variables using measures of central tendency and dispersion (mean with standard deviation and median with interquartile range) and qualitative variables as absolute frequencies (n) and relative frequencies (%). In the analysis of the differences between the 2 groups under study (pre- and post-introduction of the protocol), we compared quantitative variables by means of the Student's t test if they followed a normal distribution, and otherwise by means of the Mann–Whitney U test. We compared qualitative variables using the chi square test or the Fisher exact test. We defined statistical significance as a P-value of less than 0.05 in any of the tests. The statistical analysis was performed with the software SPSS version 20.
Ethical considerationsThe study adhered to the principles of the Convenio de Oviedo and of the Declaration of Helsinki and was approved by the clinical research ethics committee of the hospital.
ResultsA total of 365 patients received a diagnosis of AB in December of 2014 (pre-protocol group), and a total of 392 received it in December 2016 (post-protocol group). We selected 130 patients from each group by simple randomisation. We excluded 19 patients that did not meet the criteria for AB. The final sample included 113 children in the pre-protocol group and 128 in the post-protocol group.
Demographic and clinical characteristicsThe demographic characteristics were similar in both groups, with the exception of the mean age of the patients, which was slightly greater in 2016 (Table 2). The percentage of children aged less than 6 months was similar in both groups (56.6% vs 48.4%, P=.2). The clinical manifestations were also similar, although the frequency of crackles on auscultation was greater in the post-protocol group (38.1% vs 58.6%, P<.001).
Sample characteristics.
| 2014 Pre-protocol | 2016 Post-protocol | P | |
|---|---|---|---|
| Median age in months (IQR) | 5.8 (3.4–9.2) | 6.7 (3.6–11.1) | .08 |
| Male (%) | 64 (56.6) | 68 (53.1) | .33 |
| Risk factors (%) | 7 (6.2) | 9 (7.0) | .50 |
| Severity | |||
| Mild (%) | 59 (57.8) | 74 (60.2) | .41 |
| Moderate-severe (%) | 43 (42.2) | 49 (39.8) | |
IQR, interquartile range.
We did not find statistically significant differences in the performance of blood tests or chest X-rays. There was a significant decrease in the orders for rapid RSV detection tests in nasopharyngeal aspirate samples (P=.01) (Table 3).
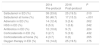
TreatmentOverall, the prescription of medications decreased significantly (Table 4).
Treatment of patients with acute bronchiolitis.
| 2014 Pre-protocol | 2016 Post-protocol | P | |
|---|---|---|---|
| Salbutamol in ED (%) | 38 (33.6) | 25 (19.5) | .010 |
| Salbutamol at home (%) | 50 (46.7) | 17 (15.3) | <.001 |
| Adrenalin in ED (%) | 14 (12.4) | 3 (2.4) | .002 |
| HSS in ED (%) | 6 (5.3) | 1 (0.8) | .042 |
| Antibiotics in ED (%) | 12 (10.6) | 9 (7) | .224 |
| Corticosteroids in ED (%) | 3 (2.7) | 5 (3.9) | .432 |
| Corticosteroids at home (%) | 4 (3.7) | 0 (0) | .055 |
| Oxygen therapy in ED (%) | 16 (14.2) | 25 (19.5) | .175 |
ED, emergency department; HSS, hypertonic saline solution.
There was a decrease in the use of nebulised salbutamol both in the ED (33.6% pre-protocol vs 19.5% post-protocol; P<.01) and in its prescription at discharge for home-based treatment (46.7% pre-protocol vs 15.2% post-protocol; P<.001). There were also significant reductions in the use of nebulised adrenaline (12.4% vs 2.4% P=.002) and nebulised HSS (5.3% vs 0.8%; P=.04) in the ED.
The prescription of antibiotics was similar in both periods (pre-protocol, 10.6%; post-protocol, 7%).
A greater proportion of patients received supplemental oxygen in 2016 (14.2% vs 19.5%), although this difference was not statistically significant (P=.17).
The use of oral corticosteroids was very rare in both groups, both in the ED (2.7% in 2014 and 3.9% in 2016) and in post-discharge treatment (3.7% in 2014 and 0%, in 2016).
OutcomeThe fate of patients after discharge from ED (admission to ward, admission to PICU, home), the number of patients that returned to the ED within 72h from discharge and the median length of stay in the ED were similar in both groups (Table 5).
Fate of patients with acute bronchiolitis.
| 2014 Pre-protocol | 2016 Post-protocol | P | |
|---|---|---|---|
| Admission to ward (%) | 32 (28.3) | 31 (24.2) | .282 |
| Return to ED after <72h (%) | 38 (33.3) | 40 (32.8) | .588 |
| Admission to PICU (%) | 3 (2.7) | 6 (5.0) | .276 |
| Median length of stay in ED in hours (IQR) | 0.8 (0.4–1.7) | 1 (0.5–2.1) | .167 |
ED, emergency department; IQR, interquartile range; PICU, paediatric intensive care unit.
The intervention at the ED level of introducing and disseminating an updated protocol for AB proved effective, as it achieved decreases in the use of bronchodilators (salbutamol and adrenaline) and nebulised HSS for treatment of AB, without associated increases in length of stay in the ED, admissions to the ward or PICU or readmission within 72h from discharge. We found the greatest decrease in the percentage of patients that received a prescription for post-discharge treatment with salbutamol, which was of 30%. The demographic and clinical characteristics of the patients and the severity of AB determined by means of the mWDF scale were very similar in the 2 patient cohorts, with the exception of age. Although the median patient age was higher in 2016 (5.8 months in 2014 vs 6.7 in 2016), this did not seem to have an effect on decision-making regarding treatment or on patient fate (admission or discharge home). The positive impact of the protocol was consistent with the findings of other studies, although these interventions are not always as effective.19,20 It is possible that reinforcing the introduction of the protocol by holding informational meetings contributed to this outcome.
The impact on the ordering of diagnostic tests was not significant except for the rapid RSV detection test, which was probably due to the fact that the proportion of patients evaluated by means of blood tests (2.7% pre-protocol vs 3.3% post-protocol) and X-rays was already very low before the introduction of the new protocol.
The percentage of patients that underwent a chest X-ray examination (2014, 8.8%; 2016, 5.5%) was very low compared to similar studies performed in hospital settings, which have reported proportions of 51% to 95% in patients admitted with AB.19 Johnson demonstrated that the use of X-rays was less frequent in children's hospitals, such as ours, compared to general hospitals, and that chest X-rays were ordered more frequently in patients admitted to hospital compared to patients discharged home from the ED.20
The group that developed the new protocol decided to continue testing for RSV in children in whom admission was indicated to facilitate the prompt implementation of measures to prevent transmission, separating RSV-positive patients from RSV-negative patients. However, given that the mechanisms of transmission of the different viruses that cause AB are similar (aerosol transmission through close contact with infected individuals, direct contact with fomites), some studies have suggested that infection control and prevention of nosocomial infection do not require identification of the causative virus, but rather the strict implementation of hygiene measures.21 The proportion of patients that underwent rapid testing for detection of RSV was very similar to the proportion of patients admitted to hospital, which reflected adherence to the protocol.
Although inflammation plays an essential role in the pathophysiology of AB, no study to date has found evidence of the effectiveness of corticosteroids for treatment of a first episode of AB in previously healthy infants. For this reason, none of the current guidelines recommends their use.5,8,9 As occurred in other studies,16,20 the protocol did not achieve a reduction in the prescription of corticosteroids due to the already low baseline proportion.
In our series, antibiotic prescription (in 10.6% of patients pre-protocol and 7% post-protocol) was less frequent compared to similar past studies,22 where the proportion has ranged between 27% and 45%, although it is important to take into account that those studies were conducted in hospitalised patients.
Oxygen therapy is one of the few interventions recommended in the management of AB.5,8,9 The debate regarding oxygen therapy revolves around the saturation threshold after which it should be given. Consistent with similar studies in the literature,20 our study did not find any differences in the proportion of children that received supplemental oxygen in each season.
In our study, the proportion of patients discharged home (approximately 70%) was similar in both groups, but a little higher compared to the proportion reported in the literature (57%).23 A possible explanation for this is that in some cases, especially those of bronchiolitis of moderate severity, our ED discharges the patient and recommends scheduling an appointment for clinical followup in the next 24h, which decreases the rate of admissions at the expense of the rate of readmission. In addition, in Spain December is the month with the most holidays, which at times impedes proper outpatient followup of patients with mild disease at the primary care level.
In health care, quality is not only a parameter necessary for adequate management of resources, but it is also an ethical imperative. Evaluating care delivery is important to implement improvement plans, prioritising critical diseases such as AB-RSV infection, which year after year give rise to an outbreak that overwhelms paediatric EDs and primary care paediatrics clinics.
Our results demonstrate that the introduction and dissemination of an evidence-based protocol can improve health care quality, as it achieved a reduction in the number of diagnostic and therapeutic interventions that are not recommended in patients with AB without a negative impact on patient outcomes. Thus, to consolidate these results, we have decided to go on with the intervention by providing all the staff that may be on call in the ED feedback regarding these outcomes, and holding an informational session every year right before the beginning of the AB-RSV epidemic season to remind the staff of the most relevant points of the protocol for the management of AB-RSV infection.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Jiménez García R, Andina Martínez D, Palomo Guerra B, Escalada Pellitero S, de la Torre Espí M. Impacto en la práctica clínica de un nuevo protocolo de bronquiolitis aguda. An Pediatr (Barc). 2019;90:79–85.