The negative impact of overweight and obesity is potentially greater in children affected by a congenital heart disease (CHD). The aim of this study is to calculate the proportion of overweight and obesity in children who underwent an intervention for CHD, and to investigate systolic arterial hypertension as a possible early cardiovascular complication.
Patients and methodsA retrospective study was conducted on patients aged 6–17 years treated for CHD, and healthy control subjects, followed-up in a Paediatric Cardiology Clinic. Body mass index percentiles were calculated according to the criteria of WHO. A review was performed on the anthropometric and clinical data, as well as the systolic blood pressure (SBP).
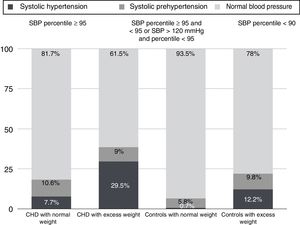
ResultsA total of 440 patients were included, of which 220 had CHD. The proportion of combined obesity and overweight (body mass index percentile ≥85) was 36.4% (37.3% in healthy subjects and 35.4% in patients with CHD, P=.738). A higher prevalence of obesity (body mass index percentile ≥97) was found in CHD patients (22.7%) compared to 15.5% in healthy subjects (P=.015). SBP percentiles were higher in overweight compared to normal-weight patients (P<.001). The prevalence of SBP readings≥the 95th percentile was greater in overweight than in normal weight CHD patients (29.5% versus 7.7%, P<.001) and also in the overweight healthy controls compared to those of normal weight (12.2% versus 0.7%, P<.001).
ConclusionsThe proportion of obesity is high in children treated for CHD and it is associated with high SBP levels. The risk of long-term complications needs to be reduced by means of prevention and treatment of obesity in this vulnerable population.
El impacto negativo del sobrepeso y la obesidad es potencialmente mayor en niños con cardiopatía congénita (CC). El objetivo del estudio es determinar la proporción de sobrepeso y obesidad en niños intervenidos de CC y valorar la existencia de hipertensión arterial sistólica como posible complicación precoz.
Pacientes y métodosEstudio descriptivo retrospectivo, incluyendo pacientes intervenidos de CC y controles sanos entre 6 y 17 años en seguimiento en una consulta de Cardiología Pediátrica. Se calcularon los percentiles del índice de masa corporal según las tablas de la OMS y se analizaron variables antropométricas, clínicas y valores de tensión arterial sistólica (TAS).
ResultadosSe incluyeron 440 pacientes, 220 intervenidos de CC. La prevalencia de exceso de peso (percentil del índice de masa corporal≥85) fue del 36,4% (el 37,3% en controles y el 35,4% en cardiópatas, p=0,738). Hubo una proporción más alta de obesidad (percentil del índice de masa corporal≥97) en afectos de CC (22,7%) que en controles (15,5%) (p=0,015). Los niños con exceso de peso tuvieron percentiles de TAS más altos (p<0,001). La prevalencia de percentiles de TAS≥95 fue mayor en los pacientes con CC con exceso de peso que en los normopeso (29,5 vs. 7,7%, p<0,001) y en los controles sanos con exceso de peso que en los normopeso (12,2 vs. 0,7%, p<0,001).
ConclusionesLa proporción de obesidad es alta en niños intervenidos de CC y se asocia a valores de TAS elevados. Es crucial reducir el riesgo de complicaciones a largo plazo mediante la prevención y el tratamiento de la obesidad en esta población tan vulnerable.
Obesity is a chronic, complex and multifactorial disease1 with severe short- and long-term adverse consequences. The prevalence of childhood obesity has increased at an alarming pace in recent decades, and it is one of the most serious public health problems of the XXI century.2 Excess weight in early childhood tends to persist through the years, and Guo et al.3 found that the probability of being obese at age 35 was up to 80% in individuals who were obese as children.
The cardiovascular complications associated with excess weight include arterial hypertension (HTN), dyslipidaemia,4,5 insulin resistance, glucose intolerance, type 2 diabetes,6 left ventricular hypertrophy and pulmonary hypertension secondary to sleep apnoea.7 In the past, it was believed that these complications occurred exclusively in adulthood, but evidence has emerged that they may develop in childhood, with some authors demonstrating an association between childhood obesity and early development of myocardial changes and coronary and thyroid disease in the paediatric age group.8,9
The negative impact of obesity can be greater in children with congenital heart disease (CHD), as these patients have underlying myocardial abnormalities on which the cardiovascular risk factors associated to obesity can be superimposed.10 At present, there are few data on the prevalence of overweigh and obesity in children with CHD, and it has only been recently that a growing concern about obesity in this group has become widespread, as recent studies have demonstrated that the prevalence in this population is high and similar to the prevalence in the general population.11–14
The aim of this study was to assess the magnitude of the problem of overweight and obesity in patients with CHD that have been treated, as well as the association between systolic HTN as a potential early complication of excess weight. To date, no such study has been conducted in Spain.
Patients and methodsPatientsWe conducted a retrospective and descriptive study that included all patients with ages 6–17 years who underwent surgery or therapeutic cardiac catheterization for treatment of CHD and were followed up in the Paediatric Cardiology Unit of the Hospital Virgen de las Nieves in Granada (Spain). We also included an equal number of healthy controls, children selected by consecutive sampling who had been referred to the unit and in whom cardiovascular disease was ultimately ruled out. We excluded patients outside the specified age range and those with genetic disorders, psychomotor retardation and/or chronic comorbidity. We selected patients by reviewing the electronic health records stored in the CardioPed database. We classified children with treated CHD into 3 groups: (1) Patients with CHD repaired surgically or through cardiac catheterization without significant residual defects15,16; (2) patients with operated or treated CHD with haemodynamically significant residual defects15,16; (3) patients with univentricular heart and Fontan circulation. We defined haemodynamically significant residual defect as a defect with clinical or echocardiographic evidence of impact on heart function or leading to remodelling due to pressure or volume overload secondary to the defect.
The study was approved by the Ethics Committee of the Hospital Universitario Virgen de las Nieves of Granada. It was performed in adherence to good clinical practice guidelines and the Declaration of Helsinki, and we followed the protocols established by the hospital for accessing data from health records.
Definitions and measuresBody weight (in kg) and height (in cm) were measured with a combined scale and stadiometer (PesPerson model), and the measurements were taken with the child standing barefoot in underwear by qualified staff. We classified nutritional status based on the body mass index (BMI) percentile, which we obtained using the 2007 World Health Organization (WHO) growth charts as reference.17 We calculated the BMI (kg/m2) using the weight and height of the patient at the time of the visit (weight [kg]/height2 [m2]). We defined overweight as a BMI at or above the 85th percentile and below the 97th percentile, and obesity as a BMI percentile of 97 or greater.
Blood pressure (BP) was measured by qualified staff with an automated sphygmomanometer, with up to 3 measurements taken in case of high blood pressure, in which case the recorded value was the mean. Blood pressure was measured after having the child sit quietly for a period of 5min, in the right arm, with the child's back supported and with the cubital fossa at heart level.18
We calculated systolic blood pressure (SBP) percentiles for age, sex and height for each patient using the tables of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents as reference.18 We defined prehypertension as a SBP between the 90th and 95th percentiles (or a SBP>120/80mmHg even if below the 90th percentile) and systolic HTN as a SBP at or above the 95th percentile.18
In patients with CHD that met the criteria for excess weight, we checked whether a diagnosis of overweight or obesity had been documented in the health records and whether written dietary and physical activity recommendations had been provided to the child.
Statistical analysisWe performed a bivariate analysis to evaluate the differences between the groups under study. We compared qualitative variables by means of the χ2 test and quantitative variables by means of the independent t test or the Mann–Whitney U test in case the assumption of normality was not met. We assessed the normality of distributions by means of the Kolmogorov–Smirnov test. We set the threshold of statistical significance at a P-value of 0.05. All the analyses were performed with the software SPSS version 19 (IBM).
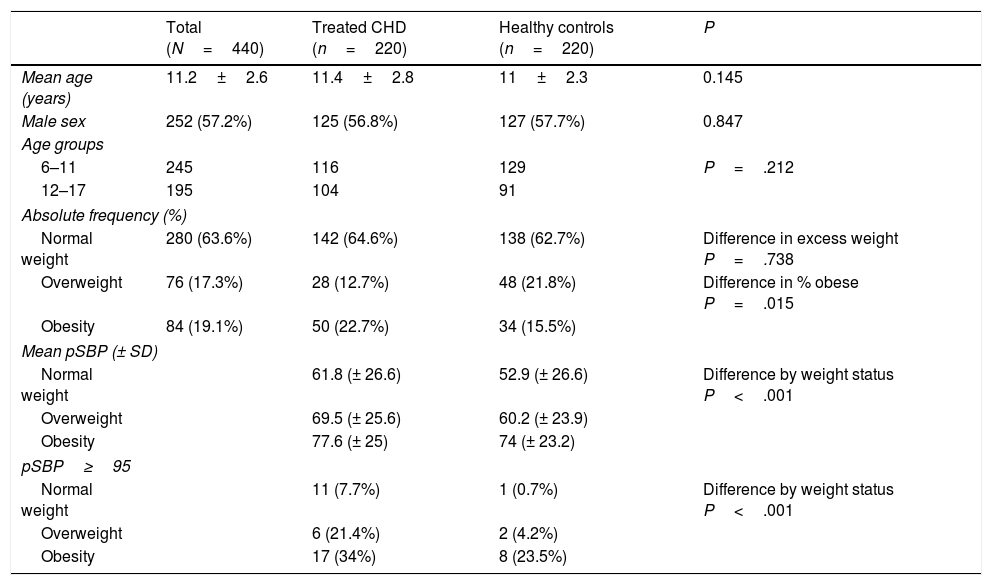
ResultsWe selected 225 patients treated for CHD. We excluded 5 due to the lack of BP measurements in their records. The final sample included a total of 440 patients—220 with treated CHD and 220 healthy controls. The mean age was 11.2 years, and 57% of the patients were male. Table 1 summarises the clinical characteristics and anthropometric and SBP measurements of cases and controls. We found no significant differences in mean age or sex between cases and controls. Based on the WHO growth charts,17 the prevalence of excess weight (overweight+obesity) in the overall sample was 36.4%, with no significant differences between cases and controls (P=.738). The prevalence of obesity in the CHD group was significantly higher compared to controls (P=.015) (Table 1). We did not find differences in the prevalence of excess weight between male and female patients in either the case group (P=.293) or the control group (P=.639). In the control group, we found a greater proportion of patients with excess weight in the subgroup aged 6–11 years (45%) compared to the subgroup aged 12–17 years (26.4%) (P=.019), while in the CHD group the proportion of excess weight was similar (35.3% in the 6–11 subgroup vs 35.6% in the 12–17 subgroup), although in the CHD group there was a higher proportion of obese children in the age 6–11 subgroup (28.6% obese) compared to the age 12–17 subgroup (16.3% obese) (P=.006).
Clinical characteristics, anthropometric measurements and systolic blood pressure percentiles (pSBP) of cases and controls.
| Total (N=440) | Treated CHD (n=220) | Healthy controls (n=220) | P | |
|---|---|---|---|---|
| Mean age (years) | 11.2±2.6 | 11.4±2.8 | 11±2.3 | 0.145 |
| Male sex | 252 (57.2%) | 125 (56.8%) | 127 (57.7%) | 0.847 |
| Age groups | ||||
| 6–11 | 245 | 116 | 129 | P=.212 |
| 12–17 | 195 | 104 | 91 | |
| Absolute frequency (%) | ||||
| Normal weight | 280 (63.6%) | 142 (64.6%) | 138 (62.7%) | Difference in excess weight P=.738 |
| Overweight | 76 (17.3%) | 28 (12.7%) | 48 (21.8%) | Difference in % obese P=.015 |
| Obesity | 84 (19.1%) | 50 (22.7%) | 34 (15.5%) | |
| Mean pSBP (± SD) | ||||
| Normal weight | 61.8 (± 26.6) | 52.9 (± 26.6) | Difference by weight status P<.001 | |
| Overweight | 69.5 (± 25.6) | 60.2 (± 23.9) | ||
| Obesity | 77.6 (± 25) | 74 (± 23.2) | ||
| pSBP≥95 | ||||
| Normal weight | 11 (7.7%) | 1 (0.7%) | Difference by weight status P<.001 | |
| Overweight | 6 (21.4%) | 2 (4.2%) | ||
| Obesity | 17 (34%) | 8 (23.5%) | ||
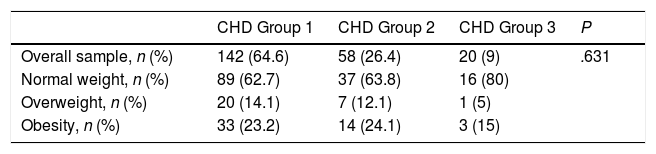
The largest group of patients with treated CHD corresponded to the group without haemodynamically significant residual defects, as can be seen in Table 2. This group included patients that underwent treatment of atrial septal defects, ventricular septal defects, patent ductus arteriosus, aortic valve stenosis (either surgery or cardiac catheterization), partial or complete atrioventricular septal defect, transposition of the great vessels or tetralogy of Fallot without haemodynamically significant residual defects. The second largest group, which included patients with haemodynamically significant residual defects, included cases of valve stenosis, tetralogy of Fallot, complex coarctation of the aorta and transposition of the great vessels. The least frequent group comprised patients with a univentricular heart that had hypoplastic left or right ventricle syndrome. Forty-seven patients (21.3% of patients with CHD) had coarctation of the aorta as a single lesion or as part of a more complex CHD. We did not find statistically significant differences in the proportion of excess weight among the 3 categories of CHD (P=.631) (Table 2).
Proportion of overweight and obesity in each treated congenital heart disease group (1: no residual defects, 2: significant residual defects; 3: univentricular heart).
| CHD Group 1 | CHD Group 2 | CHD Group 3 | P | |
|---|---|---|---|---|
| Overall sample, n (%) | 142 (64.6) | 58 (26.4) | 20 (9) | .631 |
| Normal weight, n (%) | 89 (62.7) | 37 (63.8) | 16 (80) | |
| Overweight, n (%) | 20 (14.1) | 7 (12.1) | 1 (5) | |
| Obesity, n (%) | 33 (23.2) | 14 (24.1) | 3 (15) |
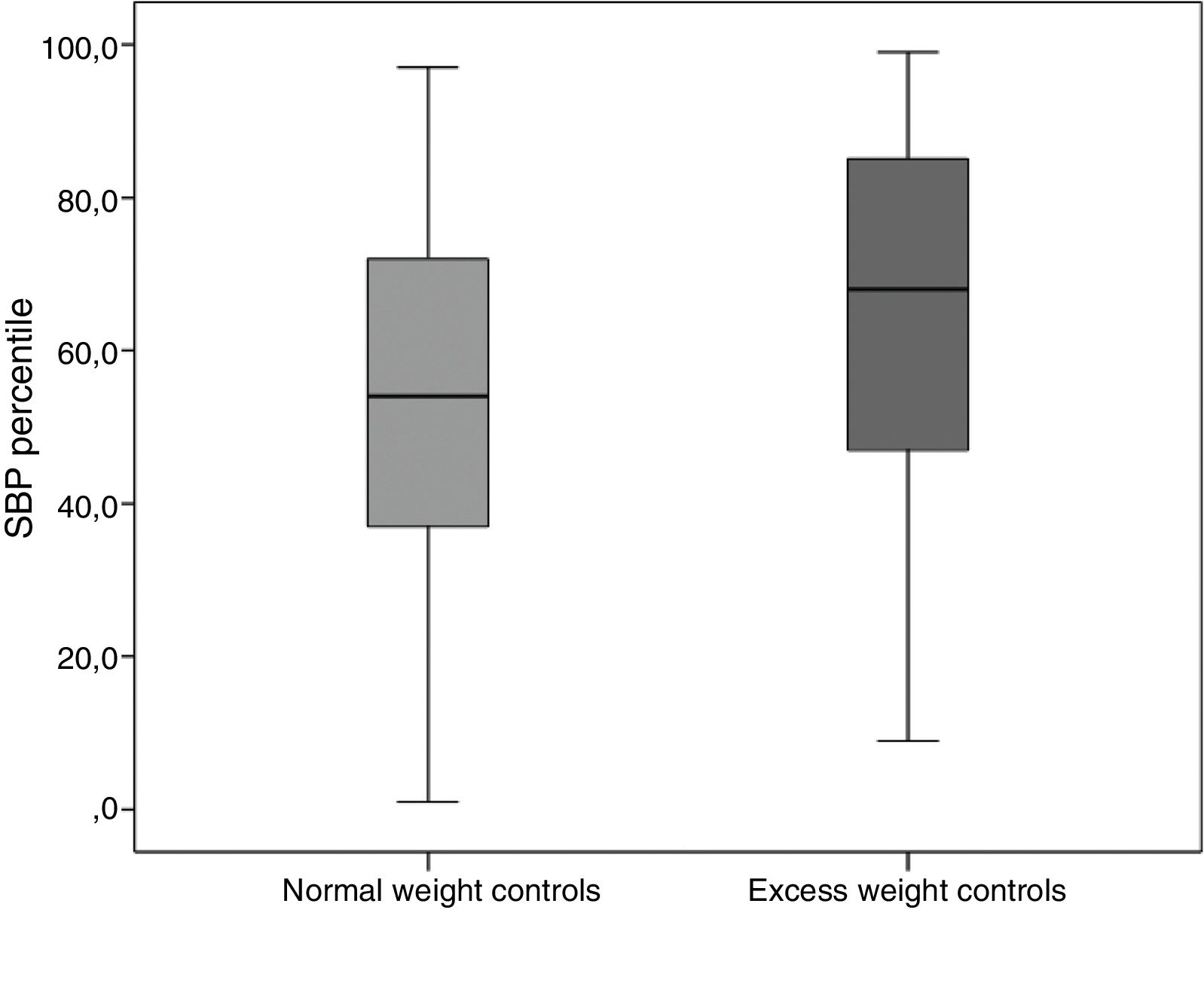
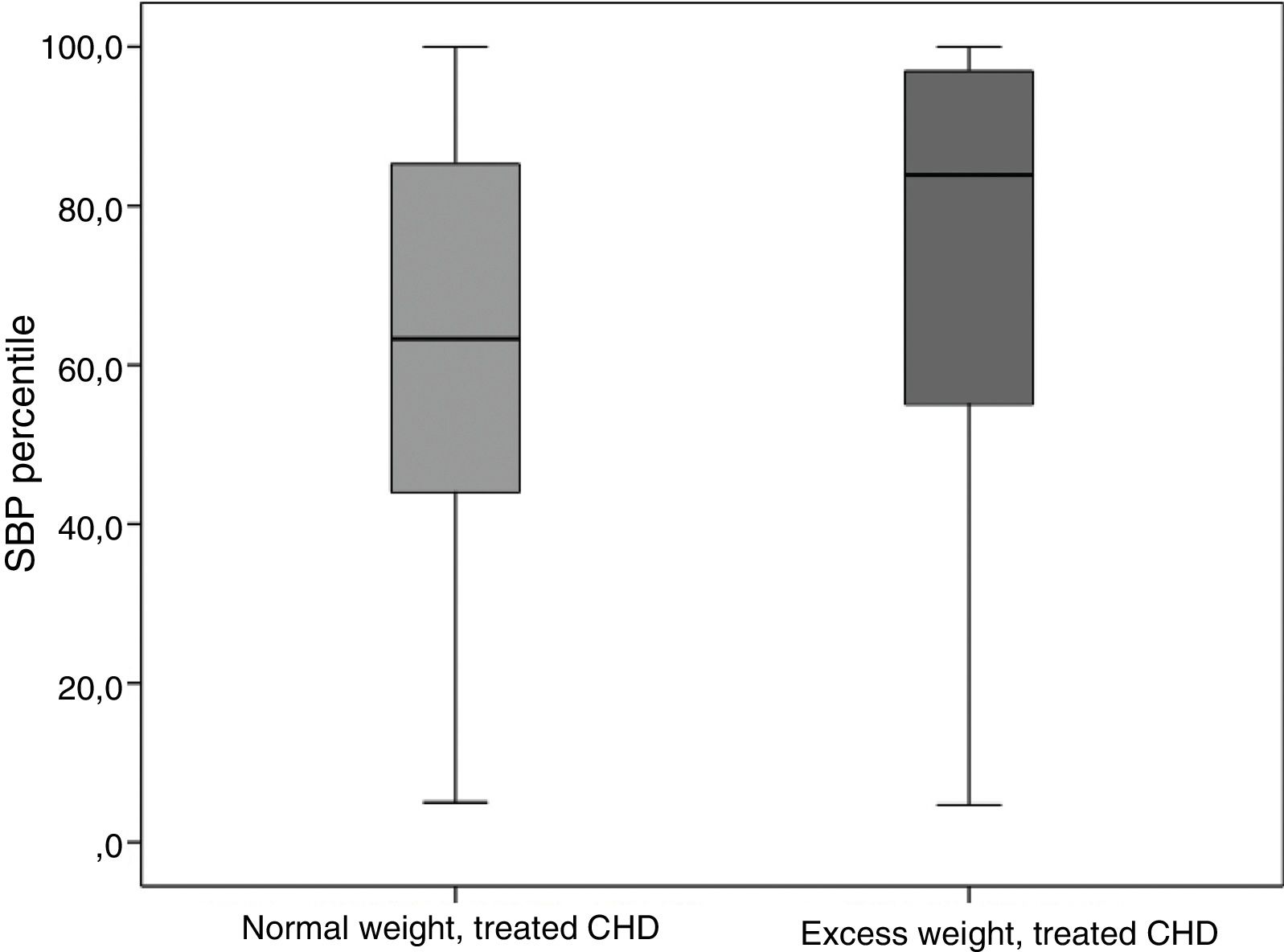
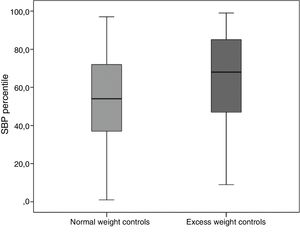
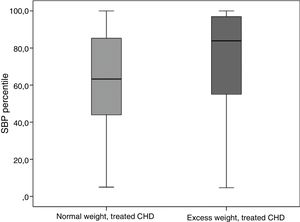
The mean SBP percentile, without taking pharmacotherapy into account, was significantly higher in the group of patients with excess weight compared to patients whose BMI was below the 85th percentile (P<.001) both in the healthy controls (Fig. 1) and in the patients with CHD of any type (Fig. 2). The mean percentile was higher in obese patients compared to overweight patients (Table 1).
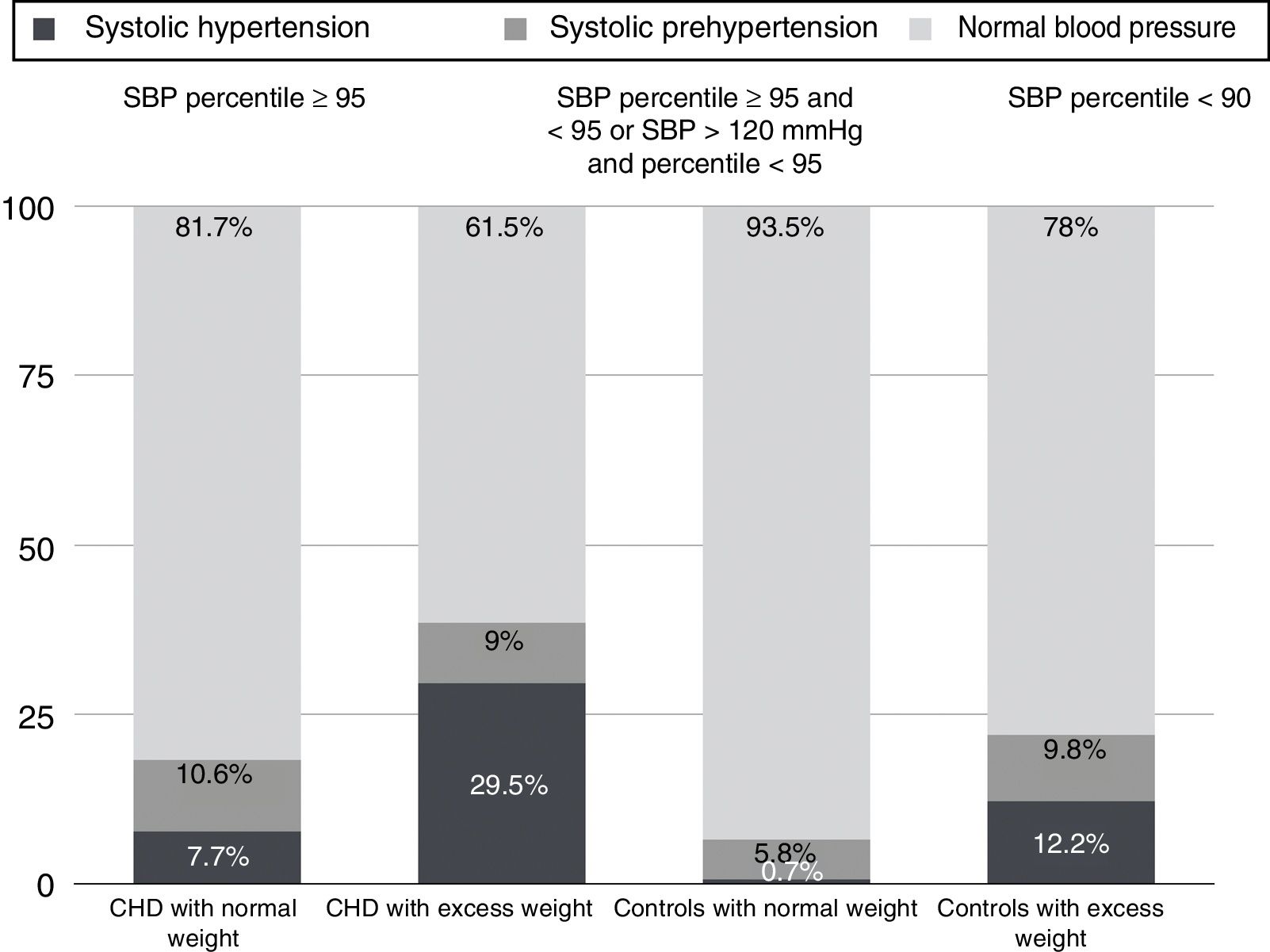
When it came to the number of patients that met the criteria for HTN, we also found significant differences in the proportion of patients with HTN between the subsets with normal weight, overweight and obesity in both the case and the control groups (P<.001) (Table 1, Fig. 3).
In the group of patients with treated CHD, we compared the SBP percentiles based on the presence or absence of coarctation of the aorta as an isolated malformation or as part of a complex CHD, and found a significantly higher mean SBP percentile in the group of patients with treated coarctation of the aorta compared to the group of patients with treated CHD that did not have this defect (P=.011).
When it came to the documented diagnosis of overweight/obesity and advice provided in regard to cardiovascular risk factors, we found records of it in 60% of patients with treated CHD and excess weight. 40% of patients with treated CHD that required this type of guidance did not receive it.
DiscussionOur study demonstrates that the prevalence of excess weight is high in Spanish children treated for CHD. At present, there is international agreement on the use of BMI threshold for diagnosis of overweight and obesity. However, in the paediatric population the BMI varies with age and sex, so it must be assessed using percentile charts. The BMI percentile charts vary widely based on the reference population and the prevalence of obesity in that particular group, so estimates of the prevalence of excess weight change substantially depending on the charts used as reference.
We decided to use the WHO charts, as recommended by the Childhood Obesity Surveillance Initiative (COSI)19 promoted by the WHO Regional Office for Europe. These are the charts used by the Spanish Ministry of Health in their surveillance study of growth, diet, physical activity, child development and obesity (ALADINO study)20 and by the Integral Plan on Childhood Obesity of Andalusia (PIOBIN).21
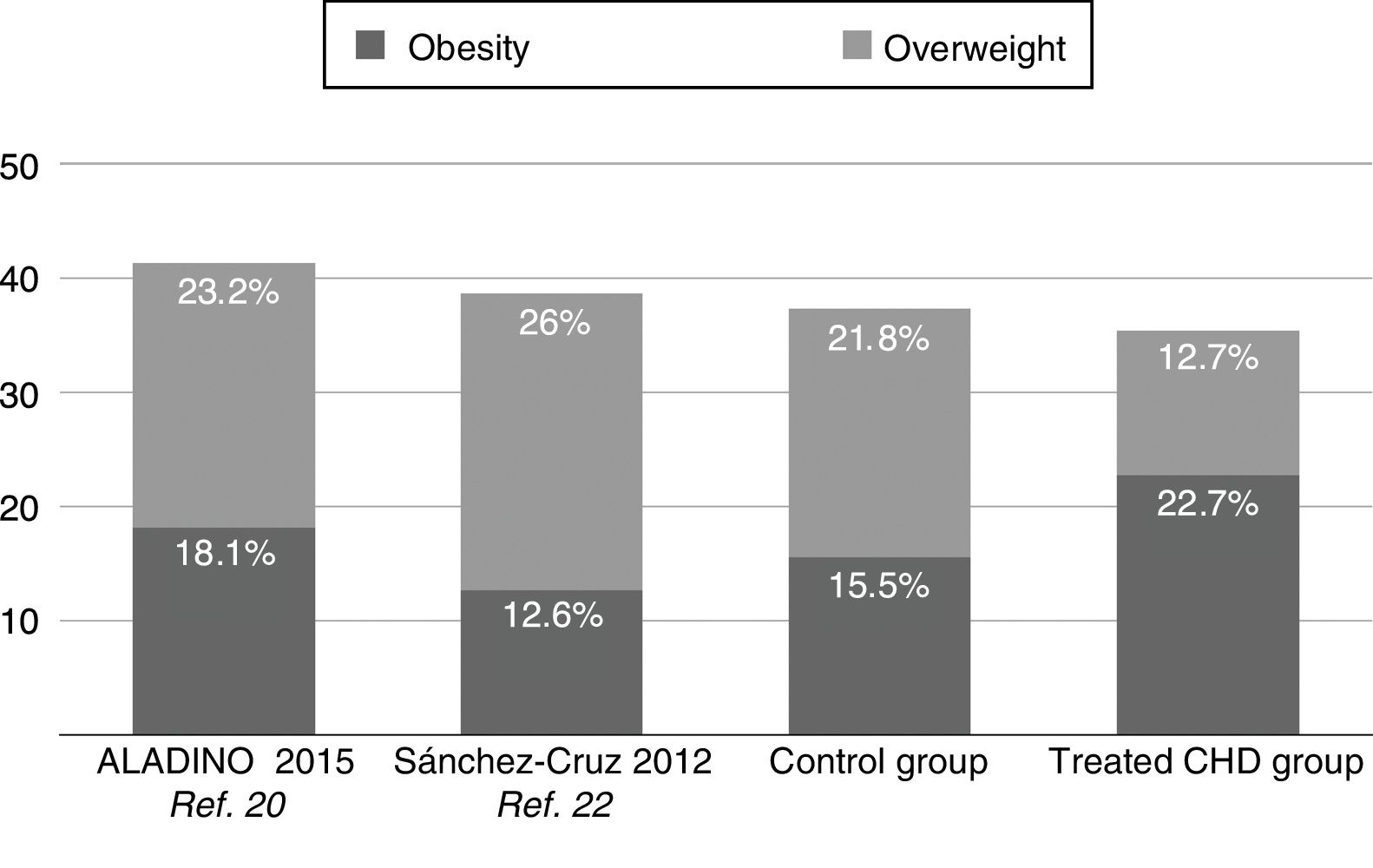
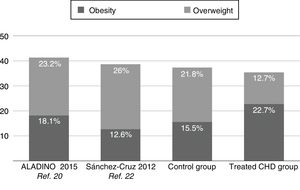
Applying the WHO standards, the results of our study show that more than one third of patients treated for CHD met the criteria for excess weight. The proportion of excess weight (35.4%) was similar to the proportion found in healthy controls and slightly lower than the proportions found in the Spanish paediatric population by Sánchez-Cruz in 2012 (38.6%)22 and the ALADINO study in 2015 (41.3%)20 (Fig. 4), both of which also used the WHO standards.17 We ought to highlight that while the study by Sánchez-Cruz et al.22 included patients aged 8–17 years, the ALADINO study only included children aged 6 to 9 years, which may explain the higher proportion of excess weight found in the latter study compared to our study and the one by Sanchez-Cruz et al, as obesity is more prevalent in children aged 6 to 11 years compared to older children, which was also corroborated by our data. Pinto et al.12 studied children followed at 2 outpatient cardiology clinics in the United States and found that 26% had overweight or obesity based on the tables of the International Obesity Task Force (IOFT). Pasquali et al.13 found a proportion of 31% of overweight or obesity in patients with CHD treated with the arterial switch operation or the Ross procedure.
A salient finding in our study was that in patients treated for CHD, the proportion of obesity was higher than the proportion of overweight and significantly higher compared to the control group. The prevalence of obesity is usually lower compared to the prevalence of overweight, as observed in the control group and in other studies in which the prevalence of overweight was up to twice that of obesity.20,22 The administration of a high-energy diet in early childhood and unnecessary restrictions to physical activity in patients treated for CHD may contribute to the increased risk of obesity in this group.11,23,24 Stefan et al.23 showed that children with CHD in whom physical activity had been restricted were at higher risk of obesity. In many cases, children with CHD have unnecessary restrictions in physical activity or sports that are either self-imposed or imposed by their parents.25,26
We did not find significant differences in the proportion of excess weight between the different CHD severity groups, although it is worth noting that the proportion of patients with excess weight was smaller (20%) in the univentricular palliation group (Fontan), which was consistent with previous studies12 that found a prevalence of 16%, lower compared to patients with other types of CHD. This phenomenon could be explained by the higher morbidity associated with the univentricular heart. It is possible that we did not find statistically significant difference due to the small number of cases.
One of the potential complications of excess weight is the development of HTN. Several studies have demonstrated that children with obesity have higher BP values compared to children with normal weight,27–29 and at present overweight is the leading cause of HTN in children. This was corroborated by our study, as the mean SBP percentile was higher in children with excess weight compared to children with normal weight in both the treated CHD and the control groups, and also higher in obese children compared to overweight children (Table 1). We found SBP levels at or above the 95th percentile in 5% of the controls, but almost exclusively in children with excess weight. An alarming proportion of patients treated for CHD (29.5% of those with excess weight and 34% of those with obesity) met the criteria for systolic HTN (Table 1, Fig. 3).
Given the findings in our population, we hope for an increased awareness among paediatricians, paediatric cardiologists and health care workers involved in the management of children with CHD. Our study found that written guidance regarding cardiovascular risk factors associated with obesity was only provided to 60% of patients with CHD and excess weight. This percentage is substantially higher to the percentages reported in other studies,12 where more than 85% of patients received no guidance, but it is still not optimal. Parents of children with obesity or overweight often believe their child's weight is adequate, and this perception may in part result from this aspect being neglected in medical appointments. Parents are more likely to consider their children's excess weight a problem if they recall a physician expressing concern about this issue.28
Primary care paediatricians and paediatric cardiology specialists both play an important role in the assessment of cardiovascular risk factors in patients with CHD.10
At present, thanks to advances in diagnostic, surgical and catheterization techniques and intensive care, the mortality of patients with CHD has decreased substantially. The challenge we currently face is to help as many patients as possible achieve a good quality of life, and therefore it is crucial to prevent exposure, starting in childhood, to modifiable cardiovascular risk factors that may have a negative impact on health in the short and the long term.
Limitations of the studyThere are limitations to our study. It had a retrospective design, with all the associated biases. The number of cases included in the study was small, specially in the group of patients with univentricular physiology. Other limitations involve the measurement of BP. The SBP was measured through the oscillometric method as opposed to the auscultatory method, and the latter is the gold standard for BP measurement.18 We only analysed systolic BP and not diastolic BP, and we did not take into account whether patients were taking any medication that could alter blood pressure values. Another of the limitations in this regard is that we only analysed the SBP values taken in a single visit, whereas clinical practice guidelines recommend repeating the measurements on 3 different occasions,18 as it has been demonstrated that BP levels tend to fall in subsequent measurements due to the phenomena of patient accommodation and regression to the mean. Despite this limitation, there is evidence that children with a high blood pressure values, even if it is recorded on a single occasion, tend to continue having BP values at high percentiles.30 Lack of measurement during other visits does not necessarily entail a low risk, and while patients might not have met the criterion of having a SBP at or above the 95th percentile in subsequent visits, many would still have values within the upper limit of normality, and there is evidence that the risks associated with high blood pressure exhibit a continuous linear trend rather than a categorical pattern.31
ConclusionOverweight and obesity are frequent in children treated for CHD. Systolic blood percentiles are higher in patients with excess weight compared to patients with normal weight. Prospective multicentre studies are necessary to define the magnitude of this problem more accurately. The prevention of obesity should be an essential component of health promotion in the entire paediatric population and an even greater priority in children with CHD, who are more vulnerable to cardiovascular complications.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank Manuela Expósito Ruiz of the Fundación para la Investigación Biosanitaria de Andalucía Oriental (FIBAO) for her help in the statistical analysis.
Please cite this article as: Perin F, Carreras Blesa C, Rodríguez Vázquez del Rey MdM, Cobo I, Maldonado J. Sobrepeso y obesidad en niños intervenidos de cardiopatía congénita. An Pediatr (Barc). 2019;90:102–108.