Acute viral bronchiolitis (AB) is one of the most common respiratory diseases in infants. However, diagnostic criteria for AB are heterogeneous and not very well known.
ObjectiveTo identify the diagnostic criteria for AB used by experts and clinical paediatricians in Spain.
MethodsDelphi study with Spanish AB experts, looking for the points of agreement about AB diagnosis. A subsequent cross-sectional study was conducted by means of an online questionnaire addressed to all Spanish paediatricians, reached through electronic mail messages sent by nine paediatric scientific societies. Descriptive and factorial analyses were carried out, looking for any association of diagnostic criteria with demographic or geographic variables, or with paediatric subspecialty.
ResultsAgreement was reached by 40 experts in many issues (first episode of respiratory distress and high respiratory frequency, diagnosis in any season of the year, and usefulness of virus identification in making diagnosis), but opposite views were maintained on key characteristics such as the maximum age for diagnosis. The online questionnaire was completed by 1297 paediatricians. Their diagnostic criteria were heterogeneous and strongly associated with their paediatric sub-specialty. Their agreement with the Spanish expert consensus and with international standards was very poor.
ConclusionsDiagnostic criteria for AB in Spain are heterogeneous. These differences could cause variability in clinical practice with AB patients.
La bronquiolitis vírica aguda (BA) es una de las enfermedades respiratorias más frecuentes en los lactantes. Sin embargo, los criterios utilizados para su diagnóstico son heterogéneos e insuficientemente conocidos.
ObjetivoIdentificar los criterios de diagnóstico de BA empleados en España, tanto por expertos como por pediatras clínicos.
MétodosEstudio de metodología Delphi con expertos españoles en BA, buscando los puntos de consenso sobre el diagnóstico de BA. Posteriormente se realizó un estudio transversal mediante encuesta online dirigida a todos los pediatras españoles, contactados a través de mensajes de correo electrónico enviados por nueve sociedades científicas pediátricas. Se hizo análisis descriptivo y análisis factorial de los resultados de la encuesta, buscando si los criterios diagnósticos empleados se relacionaban con variables demográficas, geográficas o con la subespecialidad pediátrica.
ResultadosLos 40 expertos participantes alcanzaron un consenso en muchos aspectos (primer episodio de dificultad respiratoria y aumento de la frecuencia respiratoria, diagnóstico en cualquier estación del año, y utilidad de la identificación de virus para el diagnóstico), pero manteniendo opiniones enfrentadas en cuestiones importantes como la edad máxima aceptable para el diagnóstico. A la encuesta online respondieron 1297 pediatras. Los criterios diagnósticos que aplican son heterogéneos y están fuertemente asociados con la subespecialidad pediátrica. Su acuerdo con el consenso de expertos y con estándares internacionales es muy bajo.
ConclusionesLos criterios usados en España para el diagnóstico de BA son heterogéneos. Esas diferencias pueden causar variabilidad en la práctica clínica en pacientes con BA.
Acute bronchiolitis (BA) is a disease of the lower respiratory tract caused by viral infection, especially by respiratory syncytial virus (VRS), that predominantly affects infants and exhibits a seasonal pattern.1 It is the leading reason for hospital admission in children aged less than 2 years worldwide, with an annual rate of hospitalisation of approximately 25 per 1000 children aged less than 2 years in Spain.2 Although its clinical picture has been known for a long time, it was in 1940 that the term “bronchiolitis” was first introduced to refer to it.3 This term has become the standard name for the disease. In 1967, the National Library of Medicine of the United States included bronchiolitis as a MeSH descriptor (bronchiolitis, viral).
The term bronchiolitis is currently used worldwide in hundreds of thousands of diagnoses each year, and yet there are still problems about its definition.4 There are no universally accepted diagnostic criteria, so that the same clinical picture may be diagnosed as AB or given a different label: infant asthma, bronchopneumonia, episode of wheezing or bronchitis, possibly accompanied by any of several qualifiers (spasmodic, asthmatic, catarrhal, etc.). Some authors have even questioned its being a distinct entity.5 Various scientific societies, quality assessment agencies and individual experts have developed criteria for the clinical diagnosis of AB, which differ on significant aspects.4 The case definitions and inclusion criteria used in clinical trials of AB are also heterogeneous, and many studies have considered eligible any infants with “signs and symptoms consistent with bronchiolitis”, with the authors simply stating that they applied one or other “widely accepted” definition of AB.6,7
There are also inconsistencies in clinical practice. The criteria used to diagnose AB vary, and the diagnostic label assigned to a patient with manifestations of AB determines the approach to treatment.8 Recent guidelines have established that there is no effective pharmacological treatment for AB,9,10 but clinicians do not adhere to the treatment recommendations given in current guidelines.11 This may be due to the discrepancies that exist between different guidelines,12 but also to differences in opinion about what is or is not AB.13–15 Similarly, the heterogeneity in diagnostic criteria generates disagreement in regard to the assessment of the long-term prognosis.16
The evidence on the criteria used to diagnose AB in clinical practice is scarce. A study conducted in Portugal found substantial variability in the applied criteria both in general physicians and in paediatricians.17 In Spain, the AB guideline published in 2007 by the Ministry of Health did not include a case definition,18 and published Spanish studies usually cite one of the most common definitions in the international literature. It is not known whether Spanish paediatricians use consistent criteria to diagnose AB.
The aim of our study was to find out which criteria paediatricians in Spain use to diagnose AB, including both experts on the subject and the collective of paediatricians that manage children with AB, and to analyse possible contributors to variability.
MethodsWe conducted 2 consecutive studies. In the first study, we assessed whether there was agreement between Spanish experts on the diagnostic criteria for AB using the Delphi method.19 The second one was a cross-sectional survey of clinical paediatricians carried out by means of an online questionnaire that explored their opinions regarding the diagnosis of AB. Appendix B (available in the online version of this article) provides detailed information on the methodology used.
Delphi procedure (expert consensus)- 1)
We searched the literature for consensus documents, clinical practice guidelines and systematic reviews that proposed diagnostic criteria, case definitions or standardised descriptions of AB (Appendix B, Table S1). Based on the identified sources, we developed a questionnaire to begin the Delphi procedure.
- 2)
Gathering the panel of experts. We established an explicit definition of expert (Appendix B, Table S2), and strove to obtain a group that was sufficiently representative of both the paediatric subspecialties associated with AB and the different Spanish regions.
- 3)
Delphi process. We submitted the questionnaire to the experts (Appendix B, Table S3), which included items with dichotomous answers (yes/no), multiple-choice answers and answers on a 1–10 scale to rate the importance of specific clinical characteristics in the diagnosis. We held successive rounds in which the initial responses were processed, feedback provided to participants along with a summary of the opinions of all participating experts, and new items proposed by participants added to the questionnaire. To this end, we had established criteria to define consensus and to bring the process to an end, which can be found in Appendix B.
- 4)
Analysis. We made a descriptive analysis of the responses, identifying items in which consensus was reached based on the pre-established criteria.
- 1)
Development of questionnaire. We developed a questionnaire similar to the one used in the Delphi procedure, summarising it to include the key aspects of the latter (Appendix B, Table S4).
- 2)
Administration of the questionnaire. With the help of the Asociación Española de Pediatría (Spanish Association of Pediatrics, AEP) and several other Spanish paediatrics societies (Appendix B, Table S5), we informed all their members of the project by electronic mail, inviting them to participate in an online survey and offering as an enticement entry in a draw for winning a free registration to an AEP congress.
- 3)
Sample size. We calculated the sample size based on the estimation that the population of paediatricians in Spain is of approximately 10000. We assumed the case of maximum uncertainty, and estimated a necessary sample size of 965 for a level of confidence of 95% and a precision of 3% (see Appendix B for details).
- 4)
Analysis. We performed a descriptive analysis of the questionnaire items and assessed the association between the answers and demographic variables such as age, sex, place of residence and main professional activity (subspecialty) by means of the χ2 test, Mann–Whitney U test and Spearman correlation coefficient. Applying predefined criteria (Appendix B, Table S6), we identified the answers that were consistent with 2 of the most widely used definitions of AB (McConnochie,20 NICE10) and with the expert consensus reached in the preceding Delphi process. We analysed whether the variables under study could be reduced to a smaller number of criteria by means of factor analysis (Appendix B). Subsequently, for each identified factor, we analysed whether there were differences in the factor scores based on the aforementioned demographic variables using the Kruskal-Wallis test and the Spearman correlation coefficient. We defined statistical significance as a P-value of less than .05.
The study was approved by the Research Ethics Committee of the health district of the principal investigator.
ResultsDelphi procedure – expert consensusWe identified 66 experts. We were unable to get in touch with 8 of them, and 40 responded to the invitation to participate. The panel represented a wide variety paediatric subspecialties and geographical areas (Appendix B, Table S7).
The Delphi process was completed in 2 rounds. Between the first and second rounds, there were changes in only 3 items: one in which there was consensus from the first round (adenovirus as a causative agent), one in which consensus was reached in the second round (diagnosis in any season), and another item (age limit for diagnosis) in which the change was an increased polarisation of opinion (12 months or 24 months). Table 1 presents the variables for which a consensus was reached, and Appendix B offers the full results (Appendix B, Table S8). The expert consensus can be thus summarised: AB is defined as a first episode of respiratory distress with increased respiratory rate, in any season of the year, and identification of the causative virus is helpful for diagnosis. The viruses considered potential aetiological agents of AB are RSV, rhinovirus, influenza, metapneumovirus, bocavirus, parainfluenza, coronavirus and adenovirus; the panel did not consider Mycoplasma a causative agent of AB.
Summary of the results of the Delphi procedure to achieve an expert consensus.
| Variable | Value | Round 1 | Round 2 | Change (P)a |
|---|---|---|---|---|
| Age limit for diagnosis | 6 months (%) | 7.5 | 2.7 | .046 |
| 12 months (%) | 45.0 | 51.4 | ||
| 18 months (%) | 7.5 | 0.0 | ||
| 24 months (%) | 40.0 | 45.9 | ||
| Maximum number of acceptable episodes | Only one (%) | 84.6 | 83.8 | .999 |
| Two (%) | 7.7 | 2.7 | ||
| No limit (%) | 7.7 | 13.5 | ||
| Season in which diagnosis is appropriate | Winter only (%) | 5.0 | 2.7 | .004 |
| Winter and spring (%) | 2.5 | 0.0 | ||
| Autumn and winter (%) | 15.0 | 5.4 | ||
| Autumn, winter and spring (%) | 17.5 | 10.8 | ||
| Any season (%) | 60.0 | 81.1 | ||
| Identification of causative virus is important for diagnosis | Yes (%) | 75.0 | 78.4 | .317 |
| Infectious agents that can cause bronchiolitis | ||||
| RSV | Yes (%) | 100.0 | 100.0 | 1.000 |
| Rhinovirus | Yes (%) | 94.9 | 100.0 | .317 |
| Influenza | Yes (%) | 71.4 | 77.8 | .083 |
| Metapneumovirus | Yes (%) | 97.5 | 100.0 | .317 |
| Bocavirus | Yes (%) | 89.2 | 94.3 | .157 |
| Parainfluenza | Yes (%) | 89.2 | 85.0 | .083 |
| Coronavirus | Yes (%) | 86.5 | 100.0 | .157 |
| Adenovirus | Yes (%) | 87.2 | 100.0 | .046 |
| Mycoplasma | Yes (%) | 30.3 | 25.0 | .564 |
| Relevance of signs/symptoms for diagnosis (scale 0–10) | ||||
| Increased RR | P25 | 8.0 | 8.0 | .773 |
| P75 | 9.0 | 9.0 | ||
| Respiratory distress | P25 | 8.0 | 8.0 | .163 |
| P75 | 9.0 | 9.0 | ||
AB, acute bronchiolitis; P25, 25th percentile; P75, 75th percentile; RR, respiratory rate; RSV, respiratory syncytial virus.
The AEP sent the invitation to participate to 8869 valid electronic mail addresses. We received 1297 responses (Table 2). There were participants from every autonomous community and city in Spain and all paediatric subspecialties related to AB. Table 3 summarises the answers given in the questionnaire. There was little agreement with the McConnochie criteria, the NICE criteria or the expert consensus obtained through the Delphi process. Agreement with these standards was not associated with subspecialty, age, sex or place of residence.
Online questionnaire. Demographic characteristics of the sample (n=1297).
| Type of professional activity (%) | |
| Primary care paediatrics or general paediatrics practice | 53.5 |
| Residence physician training in paediatrics | 11.7 |
| General paediatric inpatient care | 9.4 |
| Paediatric emergency care | 9.1 |
| Neonatology | 6.5 |
| Paediatric pulmonology or allergy | 5.2 |
| Paediatric intensive care | 1.3 |
| Paediatric infectious diseases | 0.5 |
| Other | 2.8 |
| Autonomous community/city (%) | |
| Madrid | 21.5 |
| Andalusia | 12.4 |
| Catalonia | 11.3 |
| Valencian Community | 8.9 |
| Basque Country | 7.1 |
| Castilla y Leon | 6.6 |
| Murcia | 4.9 |
| Aragon | 4.3 |
| Canary Islands | 4.1 |
| Castilla-La Mancha | 4.1 |
| Asturias | 3.5 |
| Navarre | 3.1 |
| Galicia | 2.7 |
| Balearic Islands | 1.7 |
| Extremadura | 1.6 |
| La Rioja | 1.0 |
| Cantabria | 0.8 |
| Ceuta and Melilla | 0.3 |
| Male sex (%) | 24.2 |
| Age in years (median and range) | 41 (25–78) |
| Frequently manages children with bronchiolitis (%) | 93.6 |
Online questionnaire. Answers.
| Age limit for diagnosis (%) | |
| 6 months | 3.2 |
| 12 months | 19.7 |
| 18 months | 4.8 |
| 24 months | 66.1 |
| 36 months | 2.2 |
| No age limit for diagnosis | 4.0 |
| Maximum acceptable number of episodes (%) | |
| 1 | 70.8 |
| 2 | 10.2 |
| 3 | 1.7 |
| 4 | 0.1 |
| No limit to acceptable number of episodes | 17.3 |
| AB can be diagnosed in any season of the year (%) | 82.9 |
| Identification of the virus is important for diagnosis (%) | 25.7 |
| It is a distinct disease (%) | 84.2 |
| Very important for diagnosisa(%) | |
| Prodromal rhinitis | 29.8 |
| Cough | 61.1 |
| Wheezing on auscultation | 65.2 |
| Crackles on auscultation | 58.1 |
| Signs of respiratory distress (intercostal retractions, nasal flaring, etc.) | 70.3 |
| Increased respiratory rate | 74.5 |
| Agreed with McConnochie criteria (%)b | 10.0 |
| Agreed with criteria of the NICE (%)b | 11.2 |
| Agreed with Spanish experts’ criteria (%)b | 7.9 |
We found significant differences based on subspecialty (Table 4), but the following three opinions dominated in all subspecialties: single episode, diagnosis possible any season of the year, and maximum age limit of 24 months for diagnosis. Intensive medicine specialists were the physicians that most frequently considered 12 months the age limit for diagnosis, followed by neonatologists and general paediatricians employed in hospitals. When it came to the importance of specific signs or symptoms for diagnosis (Table 4), those rated most relevant were respiratory distress, increased respiratory rate (especially by resident physicians, neonatologists and intensivists) and crackles. The physicians that considered cough and wheezing important most frequently were primary care paediatricians.
Online questionnaire. Answers by type of medical practice.
| PC | R | H | U | N | PA | IC | ID | Other | Pa | |
|---|---|---|---|---|---|---|---|---|---|---|
| Number of episodes acceptable for diagnosis | <.001 | |||||||||
| Only one episode | 66.6 | 88.8 | 68.9 | 76.9 | 67.5 | 69.1 | 82.4 | 83.3 | 62.9 | |
| Two episodes | 10.6 | 4.6 | 14.8 | 12.0 | 12.0 | 8.8 | 0.0 | 16.7 | 5.7 | |
| Three episodes | 2.8 | 0.0 | 0.8 | 0.0 | 2.4 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Four episodes | 0.0 | 0.0 | 0.0 | 0.0 | 1.2 | 0.0 | 0.0 | 0.0 | 0.0 | |
| No limit | 20.0 | 6.6 | 15.6 | 11.1 | 16.9 | 22.1 | 17.6 | 0.0 | 31.4 | |
| More than one episode is acceptable | 33.4 | 11.2 | 31.1 | 23.2 | 32.5 | 30.9 | 17.6 | 16.7 | 37.1 | <.001 |
| Diagnosis can be made any season of year | 78.3 | 86.2 | 89.2 | 92.3 | 82.1 | 89.7 | 88.2 | 100.0 | 88.9 | .001 |
| Maximum age limit for diagnosis | .044 | |||||||||
| 6 months | 3.3 | 2.6 | 2.5 | 0.8 | 6.0 | 1.5 | 17.6 | 0.0 | 2.8 | |
| 12 months | 20.5 | 9.2 | 23.8 | 20.3 | 22.6 | 20.6 | 17.6 | 16.7 | 25.0 | |
| 18 months | 6.1 | 2.6 | 4.1 | 3.4 | 4.8 | 2.9 | 5.9 | 0.0 | 0.0 | |
| 24 months | 63.0 | 80.3 | 67.2 | 69.5 | 58.3 | 69.1 | 58.8 | 83.3 | 63.9 | |
| 36 months | 3.2 | 0.7 | 0.0 | 2.5 | 3.6 | 0.0 | 0.0 | 0.0 | 0.0 | |
| No limit | 3.9 | 4.6 | 2.5 | 3.4 | 4.8 | 5.9 | 0.0 | 0.0 | 8.3 | |
| Diagnosis can be made after 12 months | 76.2 | 88.2 | 73.8 | 78.8 | 71.4 | 77.9 | 64.7 | 83.3 | 72.2 | .050 |
| Bronchiolitis is a distinct entity | 84.6 | 74.3 | 88.1 | 92.2 | 87.8 | 82.1 | 82.4 | 100.0 | 70.6 | .002 |
| Signs and symptoms relevant to diagnosisb | ||||||||||
| Prodromal rhinitis | 31.6 | 26.3 | 36.1 | 25.4 | 29.8 | 27.9 | 17.6 | 33.3 | 11.1 | .125 |
| Cough | 67.7 | 44.1 | 63.9 | 52.5 | 58.3 | 57.4 | 64.7 | 33.3 | 38.9 | <.001 |
| Wheezing | 73.3 | 59.9 | 57.4 | 53.4 | 59.5 | 47.1 | 52.9 | 16.7 | 58.3 | <.001 |
| Crackles | 51.0 | 71.1 | 62.3 | 66.1 | 67.9 | 60.3 | 76.5 | 83.3 | 61.1 | <.001 |
| Respiratory distress | 65.1 | 82.9 | 78.7 | 67.8 | 82.1 | 67.6 | 82.4 | 66.7 | 69.4 | <.001 |
| Increased RR | 70.9 | 86.2 | 77.0 | 75.4 | 81.0 | 73.5 | 88.2 | 66.7 | 63.9 | .005 |
| Identification of the virus is important for diagnosis | 28.5 | 19.2 | 27.3 | 16.1 | 26.2 | 25.0 | 17.6 | 33.3 | 28.6 | .112 |
Values given as percentage of physicians in each type of professional practice.
H, hospital-based general paediatrics; IC, intensive care; ID, paediatric infectious diseases; N: neonatology; PA, paediatric pulmonology or allergy; PC, primary care paediatrics or general paediatrics practice; PE, paediatrics emergency care; R, resident physician in paediatrics; RR, respiratory rate.
The opinions of respondents were also associated with their age (Appendix B, Table S9). The only significant differences between autonomous communities/cities concerned the proportion of clinicians that considered crackles or wheezing important for diagnosis (P=.035 and P<.001, respectively) and the proportion that considered that AB could be diagnosed in any season (P=.043). Male respondents were more likely to consider diagnosis in patients with more than one episode acceptable (P=.002) and the identification of the virus important for diagnosis (P=.034), with no other significant differences based on sex.
We analysed the correlation between the scores for each sign/symptom (Appendix B, Table S10). We only found a strong correlation between respiratory distress and increased respiratory rate (r=0.768).
An explanation on the method used to develop the factorial model can be found in Appendix B, and Table 5 presents the results of factor analysis. We identified 3 factors: dyspnoea, coryza and auscultation. It was not possible to include maximum age for diagnosis, number of episodes, seasonality and identification of the virus in any of those factors.
Online questionnaire. Factor analysis rotated component matrix.
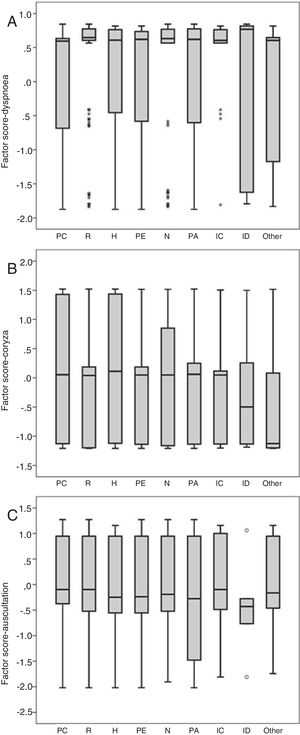
We found significant differences in the factor scores for “dyspnoea” (P<.001) and “coryza” (P=.005) based on subspecialty (Fig. 1). The factor score was higher for “dyspnoea” in medical residents, neonatologists and intensivists, while “coryza” had a higher factor score in primary care paediatricians and general paediatricians at the hospital level. We found no differences between subspecialties in the auscultation factor (P=.231).
Factor scores for dyspnoea (A), coryza (B) and auscultation (C) by subspecialty. H, hospital-based general paediatrics; IC, intensive care; ID, paediatric infectious diseases; N: neonatology; PA, paediatric pulmonology or allergy; PC, primary care paediatrics or general paediatrics practice; PE, paediatrics emergency care; R, resident physician in paediatrics.
We found no significant differences in any of the identified factors between geographical regions, except in dyspnoea, where the P-value was at the threshold of significance (P=.049) and we found no differences based on sex. Age was weakly although significantly correlated with all 3 factor scores: dyspnoea (r=−0.144; P<.001), coryza (r=0.084; P=.002) and auscultation (r=−0.077; P=.005).
DiscussionMain findings. The criteria used to diagnose AB in Spain are heterogeneous. Among experts, there is consensus on a minimum of criteria that does not extend to aspects as relevant as the age limit for diagnosis. Clinical paediatricians do not frequently use standardised criteria, but most consider that the diagnosis should be restricted to first episodes and to the first 24 months of life. The importance given to different signs or symptoms varied depending on the type of professional activity. Hospital specialists, such as intensivists or neonatologists, underscored the relevance of dyspnoea, while coryza in AB was mainly taken into consideration by primary care paediatricians. We also found moderate differences based on the age of respondents. However, our data suggest that geographical factors do not contribute to the heterogeneity of the diagnostic criteria.
Interpretation. Over 40 years ago, McIntosh stated, in regard to bronchiolitis, that “Clinicians who care for small children all know what this means”.21 This certainty seems to now be faltering, assuming it ever existed. The criteria used for diagnosis differ between countries (for instance, between the United States and northern Europe) and between the physicians in charge of these patients.17 It is known that the treatment approach chosen in children with manifestations of AB is associated with the diagnostic “label” assigned to the case,8 and some authors have even argued that the alleged ineffectiveness of pharmacotherapy in AB is due to an inadequate definition of AB.5
In the Delphi process, the most significant disagreement between the experts concerned the age limit for diagnosis. Rather than increasing agreement, the second round further polarised the positions of the experts (split between 12 and 24 months). The same division has been observed in the United Kingdom.22 This is alarming, as age is the most influential factor in giving a patient with compatible signs and symptoms a diagnosis of AB.8 All widely used definitions limit the diagnosis of AB to infants, and several establish an upper limit of 24 months,9,20,23 which was the age limit that two-thirds of the Spanish paediatricians surveyed in our study agreed with. There are other definitions, however, that propose a limit of 12 months,21,24–27 and some highlight that most cases of AB occur in infants aged less than 6 months.14,28,29 Definitions proposed by Scandinavian authors tend to have a lower age limit.29–31 Among the scarce evidence that may contribute to resolve this issue, we ought to highlight a Spanish community-based study of incident cases that identified a specific wheezing pattern consisting of a single episode typically occurring before age 13 months, with the incidence peak at 7 months.32
On the other hand, both experts and clinical paediatricians agreed that AB is a term that should only be applied to a first episode. McConnochie20 was the first to include this criterion in his definition of AB in 1983. Several clinical guidelines currently include it in their definitions.25–27,29 Others simply warn that recurrent episodes call for the exploration of other diagnoses, such as asthma or “viral-induced wheeze”.10 Many clinical trials include only infants with a first episode to forestall potential questioning of their inclusion criteria.5
It is also worth commenting on the agreement found in Spain that AB may be diagnosed any time of the year, despite the fact that children admitted during the winter epidemic season have distinct characteristics: they are more likely to be infected by RSV, have more severe presentations, are more likely to have a history of tobacco exposure during intrauterine life, are less likely to have a family history of asthma and lower plasma eosinophil counts.33 Some definitions do include the season of presentation among the criteria that are important for diagnosis.6,25,34
In the online survey, we identified 3 factors associated with the clinical manifestations of AB that we labelled dyspnoea, coryza and auscultation. Of all 3, dyspnoea is the one that explains the largest proportion of the variance in diagnosis. These factors had unequal weights in clinicians of different subspecialties. We believe that these differences are partly due to overall differences in the severity of the AB cases managed in each health care setting.
Maybe the most surpraising finding in our study is the agreement on considering AB a distinct disease, which stands in contrast to the scarce agreement on what its characteristic features are. In recent years, the conceptualization of respiratory tract diseases has been changing, as their pathophysiology is broken down into components and researchers seek to identify phenotypes and endotypes that may respond differently to treatment.35 Acute bronchiolitis has also been subject to this process. Several severe AB phenotypes have already been identified, and research in this field continues to grow.36 Thus, some of the current evidence suggests that AB due to rhinovirus has specific clinical and epidemiological characteristics37 as well as a different long-term prognosis in relation to atopic asthma.38,39 A viral aetiology is emphasised in descriptions of AB or specifically included in the definitions of disease proposed by some guidelines,6,9,25–27,34 and many clinical trials only enrol children with infection by RSV.7 Guidelines do not recommend routine testing for identification of the causative agent. It is possible that detection of RSV would make clinicians lean towards a diagnosis of AB and treatment in adherence to current guidelines, but the benefits of this approach are not actually clear.40 In our panel of Spanish experts there was consensus that viral identification was useful in the diagnosis of AB, but clinical paediatricians did not agree with this opinion.
Our results can be compared with those of a recent study conducted in Portugal.17 In the latter, only 32% of paediatricians applied the “first episode only” criterion, and 76% set the age limit at 24 months. Portuguese paediatricians considered those 2 aspects less important for diagnosis compared to general physicians, which were also surveyed in the study.
Limitations. The Delphi method can be applied in different ways. We followed international recommendations19 for the selection of experts and in establishing criteria to stop the process and to define the presence of a consensus. As is the case of any form of expert opinion, the results of the consensus process are not based on rigorous evidence, which is a limitation shared by all the diagnostic criteria for AB proposed to date. The online survey methodology entails an inherent participation bias, which is reflected by the fact that nearly 94% of respondents reported frequently managing children with AB. This bias, however, is of little relevance, as the target population of the study was precisely paediatricians that manage children with AB in Spain. We expected participation to be lower among paediatricians who were less interested in this disease, which is why we offered the incentive of the draw for a congress registration, although there is no way of knowing what effect this measure had, if any. The method used for recruitment was flawed, given the gaps that may exist in the databases of the collaborating scientific societies and that some paediatricians may not check their electronic mail often. Although it would be difficult to assess how representative the sample was, we think it is important to consider that there were participants from all autonomous communities and from all subspecialties involved in the management of children with AB. On the other hand, the answers given in the survey may not provide an accurate reflection of real-world clinical practice, and investigation of actual practices was not within the scope of our study.
ConclusionThe criteria applied by Spanish paediatricians to diagnose AB are heterogeneous, differ between experts and clinicians, and vary according to factors such as paediatric subspecialty. There is no question that this can surely hinder adherence to the recommendations of clinical practice guidelines. Initiatives have been launched, such as the one by the European Respiratory Society (https://taskforces.ersnet.org/item/standardizing-definitions-and-outcome-measures-in-acute-bronchiolitis), to attempt to standardise the diagnosis of AB, but we ought to wonder whether the resulting standard would not be just as arbitrary and flawed as previous definitions. In our opinion, it would be more fruitful to direct our efforts to deepen our understanding of the heterogeneity of AB and other respiratory diseases and to apply diagnostic labels fitting clearly differentiated and easily identifiable endotypes.
FundingThis study was funded by the Fundación Ernesto Sánchez Villares (Project 02/2017).
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the scientific societies that collaborated with the study: Asociación Española de Pediatría, Asociación Española de Pediatría de Atención Primaria, Sociedad Española de Cuidados Intensivos Pediátricos, Sociedad Española de Infectología Pediátrica, Sociedad Española de Neonatología, Sociedad Española de Neumología Pediátrica, Sociedad Española de Pediatría Extrahospitalaria y de Atención Primaria, Sociedad Española de Pediatría Hospitalaria, Sociedad Española de Urgencias Pediátricas.
Cristina Calvo, Ángeles Cansino-Campuzano, José Carlos Flores-González, Mirella Gaboli, María Luz García-García, Luis García-Marcos, Francisco Giménez-Sánchez, Javier González de Dios, Eduardo González Pérez-Yarza, Javier Korta-Murua, Yolanda M. López-Fernández, Carles Luaces-Cubells, Jorge Martínez Sáenz de Jubera, Federico Martinón-Torres, Gloria M. Moreno-Solís, Cristina Naharro-Fernández, Carlos Ochoa-Sangrador, Pablo Oliver-Goicolea, Gonzalo Oñoro, Gloria Orejón de Luna, Francisco Javier Pellegrini-Belinchón, Jimena Pérez-Moreno, Javier Pilar-Orive, Josefa Plaza-Almeida, Martí Pons-Ódena, José Miguel Ramos-Fernández, Corsino Rey-Galán, Silvia Ricart-Campos, Cristina Rivas-Juesas, Santiago Rueda-Esteban, Jesús Sánchez-Etxaniz, Manuel Sánchez-Luna, Manuel Sánchez-Solís de Querol, Marta Simó-Nebot
Appendix A lists the collaborators that assisted in this study.
Please cite this article as: Cano-Garcinuño A, Praena-Crespo M, Mora-Gandarillas I, Carvajal-Urueña I, Callén-Blecua MT, García-Merino Á, et al. Heterogeneidad de criterios en el diagnóstico de bronquiolitis aguda en España. An Pediatr (Barc). 2019;90:109–117.
Previous presentation: this study was presented in part at the XL Meeting of the Sociedad Española de Neumología Pediátrica; May 2018; Pamplona, Spain.