The consumption of ultra-processed products (UP) is associated with many diseases in the adult, such as arterial hypertension, diabetes, or asthma.
ObjectiveTo determine whether the consumption of UP in children is associated with wheezing respiratory diseases (asthma or bronchitis/recurrent wheezing).
Material and methodsA cross-sectional study was conducted within the Follow-up of the Child for Optimal Development (SENDO) project (an open, multidisciplinary and multiple outcome study of Spanish children). The consumption of UP was calculated using semi-quantitative questionnaires on the frequency of food consumption. The foods were grouped according to the NOVA classification, and the daily consumption was estimated along with the percentage of Kilocalories from the UP. The exposure was grouped into “high” and “low” from the median consumption. Odds Ratios and 95% confidence intervals were calculated for wheezing respiratory diseases associated with the high consumption UP, using low consumption as a reference. Crude and multi-adjusted estimators were calculated, and mixed regression models were used to take into account the correlation between siblings.
ResultsIn the 513 children studied (51.8% males, mean age 5.2 years), the mean consumption of UP was 446.76 g/day, representing 39.9% of the total calories ingested. A high consumption of UP was associated with an increase of 87% in the prevalence of wheezing respiratory diseases (OR: 1.87, 95% CI: 1.01–3.45). It was found that a higher consumption of UP multiplied by 2.12 (95% CI: 1.10–4.05) the prevalence of bronchitis/recurrent wheezing.
ConclusionsThe results of this study show a direct relationship between UP consumption and the prevalence of wheezing diseases in children.
El consumo de productos ultraprocesados (UP) se relaciona con múltiples enfermedades en el adulto, como hipertensión arterial, diabetes o asma.
ObjetivoEstudiar si el consumo de UP en niños se asocia con enfermedades respiratorias sibilantes (asma, o bronquitis/sibilancias de repetición).
Material y métodosEstudio transversal dentro del proyecto SEguimiento del Niño para un Desarrollo Óptimo (SENDO), una cohorte abierta, multidisciplinar y multipropósito de niños españoles. El consumo de UP se calculó mediante cuestionarios semicuantitativos de frecuencia de consumo de alimentos. Los alimentos se agruparon según la clasificación NOVA y se estimó el consumo diario y el porcentaje de kilocalorías procedentes de UP. Dividimos la exposición en «alto» y «bajo» a partir de la mediana de consumo. Se calcularon las odds ratio y los intervalos de confianza al 95% para las enfermedades respiratorias sibilantes asociadas al consumo alto de UP, usando como referencia el bajo consumo. Se calcularon estimadores brutos y multiajustados y se utilizaron modelos de regresión mixtos para tener en cuenta la correlación entre hermanos.
ResultadosEn los 513 niños estudiados (51,8% varones, edad media de 5,2 años), el consumo medio de UP fue de 446,76 g/día, representando un 39,9% de la ingesta calórica total. Un alto consumo de UP se asoció a un incremento del 87% de la prevalencia de enfermedades respiratorias sibilantes (OR 1,87; IC 95% 1,01–3,45). Encontramos que un mayor consumo de UP multiplica por 2,12 (IC 95% 1,10–4,05) la prevalencia de bronquitis/sibilancias de repetición.
ConclusionesNuestros resultados muestran una asociación directa entre el consumo de UP y la prevalencia de enfermedades sibilantes en niños.
Respiratory diseases are increasingly frequent in the paediatric age group, and asthma is the most prevalent chronic disease of childhood in developed countries.1,2 In Spain, the prevalence of childhood asthma exceeds 10% and its incidence continues to increase.3 Although it has a genetic basis, the aetiology of asthma is multifactorial, with exogenous factors such as exposure to tobacco smoke, environmental pollution, diet and breastfeeding playing an important role.1,4,5 Consequently, the analysis of modifiable risk factors, including dietary factors, is essential for the purpose of developing primary prevention strategies and improve symptom control in asthma.6
The Mediterranean diet has proven to have a protective effect on the risk of recurrent wheezing and asthma,5,7 but in recent years there has been a tendency toward its replacement with the Western pattern diet in Spain. This shift is particularly evident in children and youth, with a decrease in the average intake of fruits and vegetables and an increase in the intake of animal products and processed and ultraprocessed (UP) foods.8
Ultraprocessed foods are defined as industrial formulations made from substances extracted from foods (starches, sugars, etc.) or synthesised in laboratories. They are rich in added sugars, salt, saturated fats, additives and preservatives, foods with a low nutritive value but that are very palatable, durable and widely available. Most of these products contain none or a very small quantity of the original natural food substrate and have no nutritive value, have been made to consume directly or after heating, require little cooking and are very affordable.9
There is evidence that consumption of UP foods in the adult population is associated with several diseases, such as high blood pressure, cardiovascular disease, diabetes mellitus, cancer, obesity or depression,10–14 as well as an increase in all-cause mortality.15,16 When it comes to respiratory diseases, consumption of UP foods is associated with an increased prevalence of asthma and other respiratory diseases in adolescence and adulthood, while consumption of UP foods during pregnancy is associated with subsequent development of wheezing in the child.17,18 However, few studies have analysed consumption of UP foods and its association with respiratory diseases in childhood. The aim of our study was to assess the potential association between consumption of UP products and wheezing disorders in school-age children included in the project SEguimiento del Niño para un Desarrollo Óptimo (Follow-up of Children for Optimal Development, SENDO), a cohort in the Mediterranean region.
Material and methodsStudy designSENDO is a multipurpose, prospective and dynamic cohort study. The primary objective of the SENDO project is to assess the effects of dietary and lifestyle habits on child and adolescent health. More information on the project, the participants and the questionnaires used is available at www.proyectosendo.es. Enrolment started in 2015 and is ongoing, that is, new participants can join SENDO at any time. The inclusion criteria are: (1) age 4–5 years, and (2) residing in Spain. At present, approximately 76% of children in the SENDO cohort belong to the Navarre node (the region where SENDO started), 16% to the Balearic Islands node, 2% to the Madrid node, 2% to the Andalusia node and the rest to other nodes. The sole exclusion criterion is lack of access to a device with an internet connection to complete the questionnaires. Most patients are recruited by their paediatricians, but recruitment is also conducted through various promotional campaigns in schools, sports events, the print press or social media. When participants decide to join the cohort, they can enrol directly through the project website or enrol with the help of their paediatrician at the primary care centre. Follow-ups are conducted yearly through online questionnaires, completed mainly by parents and to a lesser extent by participants. Before enrolment, parents or legal guardians sign and submit to the research team a copy of the informed consent form. A few weeks later, they receive a link to the online questionnaires by email. Each year, parents receive a link to a new follow-up questionnaire that changes based on the age of the child.
For the present study, we used data collected for children that enrolled in SENDO between 2015 and 2019 and had completed the baseline questionnaire (Q0). Of the 537 eligible participants, 24 had not provided the necessary information to calculate the consumption of UP products, but all provided data to assess the outcome (respiratory illness), which resulted in a final sample of 513 participants.
Description of the variables under studyThe Q0 collects exhaustive information about the health of the child as well as the personal and family history, sociodemographic characteristics, lifestyle and dietary habits through more than 1000 items.
We collected dietary data regarding consumption of UP products through a semiquantitative food frequency questionnaire (FFQ) validated in the paediatric population19 that included 149 foods organised into 10 categories (dairy; eggs, meat and fish; vegetables; fruit; cereal and legumes; oils and fats; confectionery and savoury snacks; baked goods; beverages and miscellanea). The amount that constituted 1 serving was provided for each food. Parents were asked to report how frequently the participant had consumed each of the foods in the past year by choosing 1 out of 9 answer choices (from “never or almost never” to “6 or more times daily”). A team of nutritionists calculated the macronutrient and micronutrient composition of each food using data from food composition tables published in Spain.20
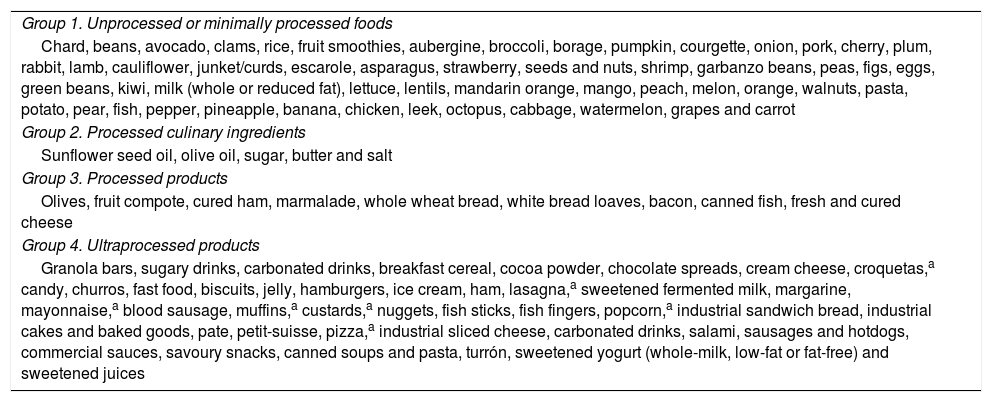
We categorised the 149 foods included in the FFQ based on the degree of processing using the NOVA classification, which differentiates 4 food groups.21 Group 1 in the NOVA classification includes unprocessed or minimally processed foods. Group 2 includes processed culinary ingredients. Group 3 includes processed foods, usually through the addition of sugar, oil or salt to foods in group 1. Group 4 is formed by UP foods, including industrial processing and use of synthetic antioxidants, stabilizers and preservatives. Table 1 presents the classification of the foods included in the FFQ of the SENDO project based on the NOVA classification. Some examples of UP foods in the FFQ are sugary drinks, fast food, salty snacks and industrial baked goods. We calculated the food intake corresponding to each of the 4 groups in g/day and kcal/day as well as the percentage of the total energy intake corresponding to each of the groups. For the analysis, we divided participants into 2 groups (high and low consumption) based on the median consumption of UP products (NOVA group 4), using the low-consumption group as reference.
Classification of the foods included in the food frequency questionnaire of the SENDO project by the degree of processing, established based on the NOVA food classification system.
| Group 1. Unprocessed or minimally processed foods |
| Chard, beans, avocado, clams, rice, fruit smoothies, aubergine, broccoli, borage, pumpkin, courgette, onion, pork, cherry, plum, rabbit, lamb, cauliflower, junket/curds, escarole, asparagus, strawberry, seeds and nuts, shrimp, garbanzo beans, peas, figs, eggs, green beans, kiwi, milk (whole or reduced fat), lettuce, lentils, mandarin orange, mango, peach, melon, orange, walnuts, pasta, potato, pear, fish, pepper, pineapple, banana, chicken, leek, octopus, cabbage, watermelon, grapes and carrot |
| Group 2. Processed culinary ingredients |
| Sunflower seed oil, olive oil, sugar, butter and salt |
| Group 3. Processed products |
| Olives, fruit compote, cured ham, marmalade, whole wheat bread, white bread loaves, bacon, canned fish, fresh and cured cheese |
| Group 4. Ultraprocessed products |
| Granola bars, sugary drinks, carbonated drinks, breakfast cereal, cocoa powder, chocolate spreads, cream cheese, croquetas,a candy, churros, fast food, biscuits, jelly, hamburgers, ice cream, ham, lasagna,a sweetened fermented milk, margarine, mayonnaise,a blood sausage, muffins,a custards,a nuggets, fish sticks, fish fingers, popcorn,a industrial sandwich bread, industrial cakes and baked goods, pate, petit-suisse, pizza,a industrial sliced cheese, carbonated drinks, salami, sausages and hotdogs, commercial sauces, savoury snacks, canned soups and pasta, turrón, sweetened yogurt (whole-milk, low-fat or fat-free) and sweetened juices |
The endpoint was the prevalence of wheezing illness reported by the parents. We defined positive case of asthma as a “yes” answer to the item in the Q0 “Has your child been given a diagnosis of asthma by a physician?” or a history of hospital admission due to asthma or under pharmacological treatment for asthma control in the past year. We defined positive case of recurrent wheezing/bronchitis as a “yes” answer in any of the following items: “Has your child been given a diagnosis of recurrent wheezing by a physician?”, “Has your child been given a diagnosis of asthma by a physician of recurrent bronchial obstruction syndrome or RBOS?” or “Has your child been given a diagnosis of recurrent bronchitis by a physician?”. Lastly, we defined positive case of wheezing illness as an existing diagnosis of asthma or recurrent wheezing/bronchitis. We excluded children whose parents reported a medical diagnosis of bronchopulmonary dysplasia, cystic fibrosis or other chronic pulmonary diseases.
Statistical analysisWe classified participants into 2 groups based on their median consumption of UP products. To describe the sample under study, we compared quantitative and qualitative variables in the 2 groups by means of the Student t test and the chi square test, respectively. We calculated crude and adjusted odds ratios (ORs) with the corresponding 95% confidence intervals (CIs) to analyse the association between UP product consumption (independent variable) and the presence of wheezing illness (dependent variable).
The analysis was adjusted for age, sex, race, perinatal variables (preterm birth and birth weight), history of asthma or allergy in first-degree relative and exposure to tobacco smoke. We also took into account the total energy intake (estimated in total kcal/day), the degree of adherence to the Mediterranean diet (estimated by means of the KIDMED index22), the level of physical activity (estimated in metabolic equivalent of task [MET]/hour/week) and the body mass index (BMI) z-score, as it a better marker of obesity/overweight than the weight in kilograms. We calculated the BMI as weight (kg) divided by height square (m2) and the BMI z-score based on the 2012 International Obesity Task Force standards.23
We fitted mixed models to take into account correlations between siblings. Lastly, we calculated predictive values and generated scatterplots and logistic regression curves to describe the association between consumption of UP products and the frequency of wheezing illness overall and asthma and recurrent wheezing/bronchitis in particular. Previous studies in this cohort in the context of the SENDO project found a high validity for the self-reported data.24 All the statistical analyses were performed with the software Stata version 14.1, and we defined statistical significance as a p-value of less than 0.05.
Ethical considerationsThe SENDO study was conducted in adherence to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of the Government of Navarre (Project 2016/122). We obtained signed informed consent from the parents or legal guardians of all participants prior to participation in the study, including a specific clause authorising the SENDO medical team to access the health records to verify self-reported information and diagnoses.
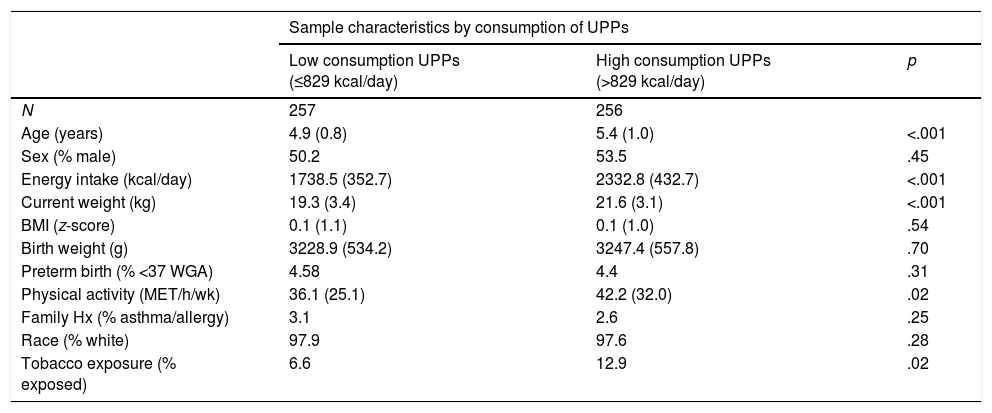
ResultsWe analysed data for 513 school-age children in Spain (51.8% male, mean age 5.2 years). The mean weight of participants was 19.9 kg, with a mean BMI z-score of 0.07. The mean daily energy intake was 2035.08 kcal/day (standard deviation, 494.9) and the median energy intake was 1986 kcal/day. When it came to consumption of UP products, we found a mean daily consumption of 446.76 g corresponding to an energy intake of 829.22 kcal/day, or 39.9% of the mean total energy intake. More specifically, 88.3% of participants consumed more than 30% of the total energy intake in the form of UP products and 16.2% consumed more than 50% of the total energy intake in the form of UP products. As for respiratory diseases, out of 513 children, 104 (20%) reported having received a diagnosis of wheezing illness from a physician, including 40 cases of asthma (7.8%) and 64 (12.5%) of recurrent wheezing/bronchitis. Fifty participants (9.7%) reported exposure to tobacco smoke, 12 (3.2%) a family history of asthma or allergy and 23 (4.5%) a personal history of preterm birth (<37 weeks’ gestation). Table 2 summarises the main characteristics of the participants based on the consumption of UP products. The group of children with high consumption of UP products was significantly older, had a higher reported total energy intake and a greater proportion of exposure to tobacco smoke.
Characteristics of the sample based on the median consumption of ultraprocessed products (UPP). SENDO project, 2015–2019.
| Sample characteristics by consumption of UPPs | |||
|---|---|---|---|
| Low consumption UPPs (≤829 kcal/day) | High consumption UPPs (>829 kcal/day) | p | |
| N | 257 | 256 | |
| Age (years) | 4.9 (0.8) | 5.4 (1.0) | <.001 |
| Sex (% male) | 50.2 | 53.5 | .45 |
| Energy intake (kcal/day) | 1738.5 (352.7) | 2332.8 (432.7) | <.001 |
| Current weight (kg) | 19.3 (3.4) | 21.6 (3.1) | <.001 |
| BMI (z-score) | 0.1 (1.1) | 0.1 (1.0) | .54 |
| Birth weight (g) | 3228.9 (534.2) | 3247.4 (557.8) | .70 |
| Preterm birth (% <37 WGA) | 4.58 | 4.4 | .31 |
| Physical activity (MET/h/wk) | 36.1 (25.1) | 42.2 (32.0) | .02 |
| Family Hx (% asthma/allergy) | 3.1 | 2.6 | .25 |
| Race (% white) | 97.9 | 97.6 | .28 |
| Tobacco exposure (% exposed) | 6.6 | 12.9 | .02 |
BMI, body mass index; Hx, history; UPP, ultraprocessed product; WGA, weeks of gestational age.
Quantitative data expressed as mean and standard deviation and qualitative data as percentages.
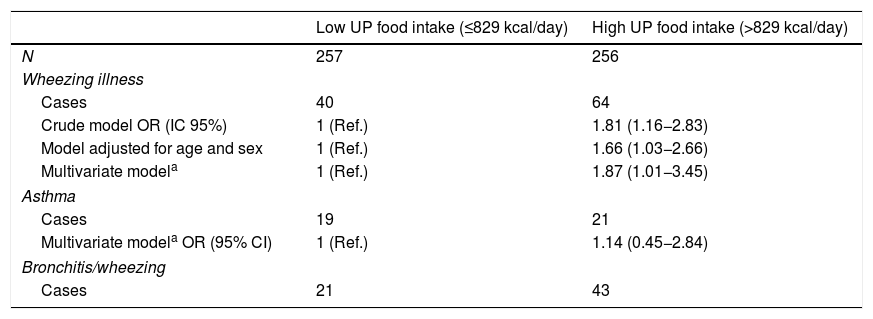
The crude analysis of the association between the consumption of UP products and wheezing illness showed a1.81-fold increase (95% CI, 1.16–2.83) in the risk of wheezing illness during childhood in children with high consumption of UP products. The association was slightly stronger in the adjusted multivariate analysis (OR, 1.87; 95% CI, 1.01–3.45) (Table 3). When we studied specific wheezing illnesses separately, we found that greater consumption of UP products increased the probability of recurrent wheezing/bronchitis by a factor of 2.12 (95% CI, 1.10–4.05), including recurrent bronchitis, recurrent wheezing and RBOS and the probability of asthma by a factor of 1.4 (OR 1.44; 95% CI, 0.46–2.84), although the association with asthma was not statistically significant.
Odds ratio and 95% confidence intervals for the presence of wheezing illness based on the consumption of ultraprocessed (UP) products. SENDO project, 2015–2019.
| Low UP food intake (≤829 kcal/day) | High UP food intake (>829 kcal/day) | |
|---|---|---|
| N | 257 | 256 |
| Wheezing illness | ||
| Cases | 40 | 64 |
| Crude model OR (IC 95%) | 1 (Ref.) | 1.81 (1.16−2.83) |
| Model adjusted for age and sex | 1 (Ref.) | 1.66 (1.03−2.66) |
| Multivariate modela | 1 (Ref.) | 1.87 (1.01−3.45) |
| Asthma | ||
| Cases | 19 | 21 |
| Multivariate modela OR (95% CI) | 1 (Ref.) | 1.14 (0.45−2.84) |
| Bronchitis/wheezing | ||
| Cases | 21 | 43 |
CI, confidence interval; OR, odds ratio; Ref, reference group; UP, ultraprocessed.
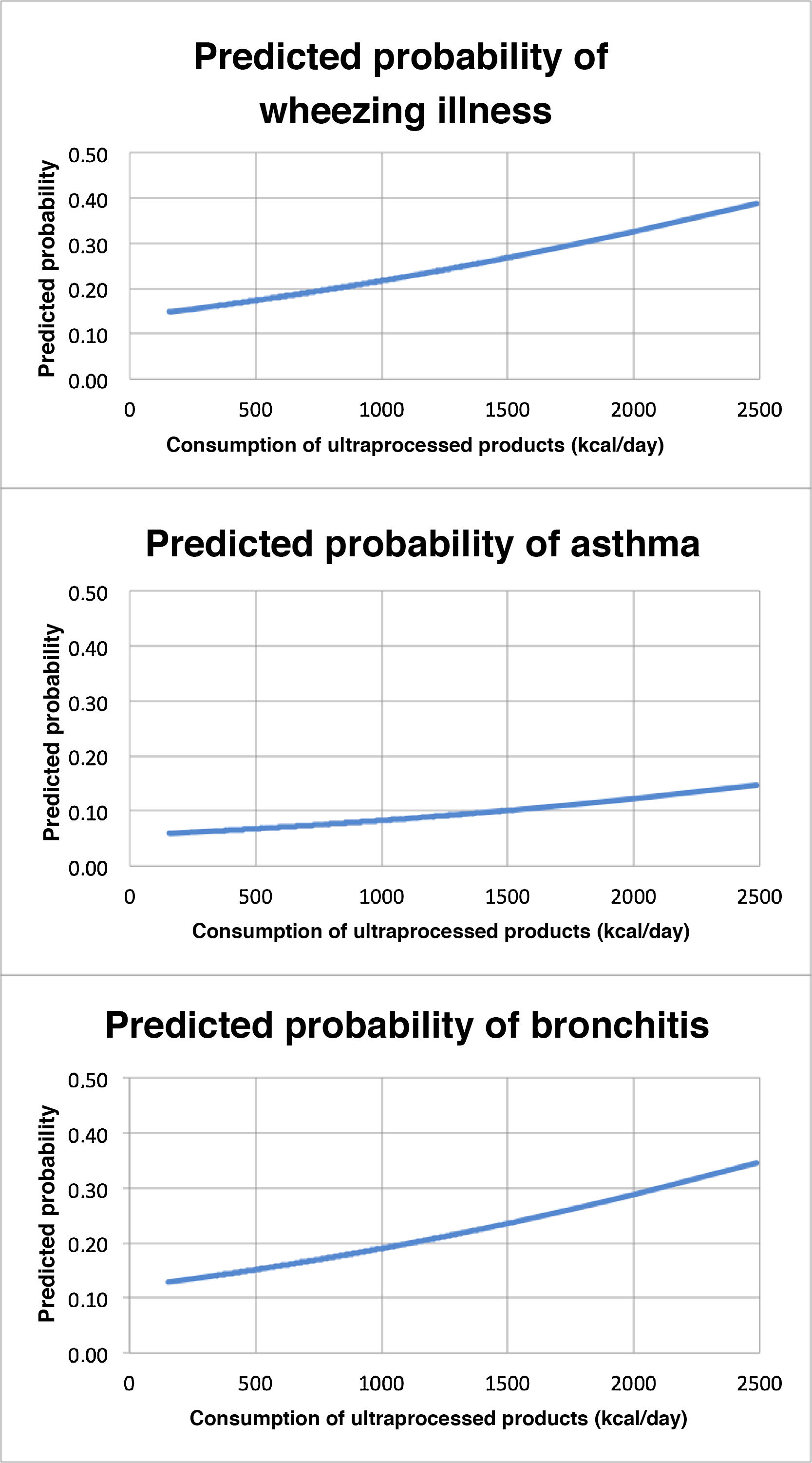
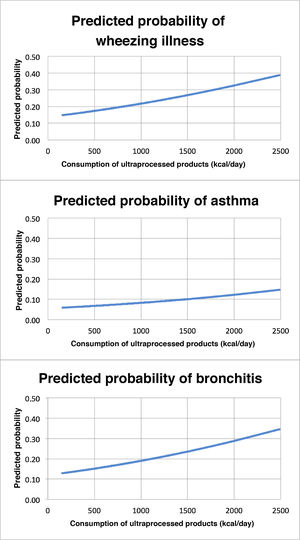
Lastly, we calculated the predictive value of the consumption of UP products for respiratory disease by charting the regression curve, assessing the association between consumption of UP products (in kcal/day) and wheezing illnesses, and analysing the scatter plot for asthma and bronchitis/wheezing separately. Fig. 1 presents the 3 charts, where we can see that the probability of the respiratory diseases under consideration (y-axis) increased with increasing daily consumption of UP products (x-axis).
Predicted probability of disease based on the consumption of UP products. Logistic regression curve for the analysis of the association between consumption of UP products (x-axis) and respiratory diseases (y-axis), with the first chart representing the association with wheezing illness overall, the second with asthma and the third with wheezing/bronchitis. Study in children that participate in the SENDO project in Spain.
The findings in the sample of 513 school-age children in Spain evince a direct linear association between the consumption of UP products and the development of wheezing illnesses, with a crude OR for wheezing illness in the high UP products consumption category of 1.81 (95% CI, 1.16–2.83) with the low consumption category as reference. This association remained in the multivariate analysis, in which consumption of UP products was associated with an 87% increase in the frequency of wheezing illness (OR 1.87; 95% CI, 1.01–3.45).
Globalization has fostered a homogenisation of dietary patterns and industrialization has facilitated the displacement of traditional dietary patterns, including the Mediterranean diet, by the Western pattern diet, while the consumption of sweetened, processed and UP products has increased substantially in recent years worldwide.25 It is known that traditional dietary patterns, such as the Mediterranean diet,26 are associated with a decreased risk of obesity, asthma and wheezing illness, probably due to their high vitamin and antioxidant content. However, the analysis adjusted for adherence to the Mediterranean diet (KIDMED), total energy intake (kcal/day) and obesity (BMI z-score) did not affect the results, which leads us to believe that there is a direct association between the consumption of UP products and wheezing diseases that is not mediated by the degree of adherence to the Mediterranean diet.
Our findings are similar to those of other studies conducted in the adult and adolescent populations. The mean energy intake of participants in our study was above the upper threshold established for their age group, although participants were not obese and the consumption of UP products was similar to the consumption reported in paediatric populations in developing countries. A study conducted in adolescents in Brazil that also used self-reported data had similar results, finding an association between consumption of UP products and the presence of asthma and wheezing that was dose-dependent, with an OR in the quintile with the highest consumption of UP products of 1.27 (95% CI, 1.15–1.41) for asthma and 1.42 (95% CI, 1.35–1.50) for wheezing.27 The data in our study showed the same association with a similar strength in the case of wheezing/bronchitis, while the lack of statistical significance of the association with asthma may have been due to the small sample size. Due to the difficulty of performing lung function tests in early childhood, asthma may be underdiagnosed in preschool-age children or labelled with less specific terms, such as “recurrent wheezing” or “recurrent bronchial obstruction syndrome”.
The SENDO project is characterised by the collection of exhaustive information, but we ought to mention its main limitations. First of all, its cross-sectional design did not allow establishment of causal relationships or calculation of relative risks, so we could only make inferences about associations but not causality. Also, since the data were self-reported, there is a risk of information bias, although previous studies have demonstrated the validity of self-reported data in similar cohorts with highly educated participants, such as the SUN study.7 Another limitation is the estimation of the consumption of UP products based on the responses to a FFQ. The high mean energy intake reported by our participants may be biased due to overestimation by parents of the food consumed by their children.28 At any rate, it is unlikely that inaccuracies in the reported consumption of UP products would be associated with the previous diagnosis of wheezing illness or asthma, so information bias on this aspect would not result in differential misclassification and would bias the measure of the association towards the null. Furthermore, both the FFQ used in the study and several self-reported measures in the SENDO project have been previously validated and published. The results of the validation study of the FFQ showed an acceptable reproducibility and acceptable validity for the evaluation of nutrient and food consumption in Spanish preschoolers.19,24
The SENDO cohort is mainly comprised of households with a middle to high socioeconomic and educational level (82% of parents had an undergraduate university degree or higher). This cohort is not representative of the general population of Spain. However, the inference of the association between variables, beyond being a purely statistical process, is based on underlying biological processes and therefore is not conditioned by how representative the sample is. In cohort studies, the validity of self-reported data and losses to follow-up must be given more importance compared to how representative the sample is.29 Of the 573 participants that provided informed consent, 537 corrected the Q0 completely (92%). In 2015, in a cohort of 170 children in the SENDO pilot study, the reported cases of asthma and respiratory diseases were confirmed by a paediatric pulmonologist through the review of health care records including primary care, paediatric pulmonology and allergology records, and all reported cases of respiratory disease were confirmed as accurate. Also, the use of self-reported data for variables such as gestational age, height or weight has also been validated with a high correlation and excellent agreement, such as an intraclass correlation coefficient for the weight of 0.95 (95% CI, 0.94–0.96) and a rate of agreement for gestational age of 97% with a weighted kappa index of 0.90 (95% CI, 0.89–0.90).24
We consider that given the high prevalence of respiratory diseases in the paediatric age group and their increasing incidence in recent years, it is important to thoroughly study potential aetiological factors to establish effective prevention strategies. More prospective studies are required to assess the observed association between consumption of UP products and the development and outcomes of respiratory diseases in the long term.
In conclusion, our study, conducted in a sample of 513 children in Spain, found a direct association between consumption of UP products and wheezing illness during childhood.
Funding- •
Ignacio H. de Larramendi Research Grants, Fundación MAPFRE, 2015.
- •
SENP Grant for Young Researchers of the Sociedad Española de Neumología Pediátrica, 2016.
- •
Research gant, Fundación AEP, Invest-AEP, Asociación Española de Pediatría, 2018.
The authors have no conflicts of interest to declare.
We thank the Fundación MAPFRE for funding the pilot study through the Ignacio H. de Larramendi research grant, the Sociedad Española de Neumología Infantil for the award of the 2016 SENP Young Researchers Grant and the Asociación Española de Pediatría and Fundación-AEP for awarding a research grant (Invest-AEP 2018). The SENDO project has become a reality thanks to the collaboration of the Universidad de Navarra and the public health system of Navarre. Therefore, we also want to express our gratitude for the collaboration of all the primary care paediatricians of the public health system of Navarre and the Complejo Hospitalario de Navarra and the researchers at the Universidad de Navarra. We also thank the paediatricians cooperating through the SENDO nodes in Madrid, the Basque Country, Canary Islands and Balearic Islands. Lastly, and most importantly, we thank all the participants, children and families, for their time, patience and willingness to collaborate with us in the development of the SENDO project.
Please cite this article as: Moreno-Galarraga L, Martín-Álvarez I, Fernández-Montero A, Santos Rocha B, Ciriza Barea E, Martín-Calvo N. Consumo de productos ultraprocesados y enfermedades respiratorias sibilantes en niños. Proyecto SENDO. An Pediatr (Barc). 2021;95:18–25.