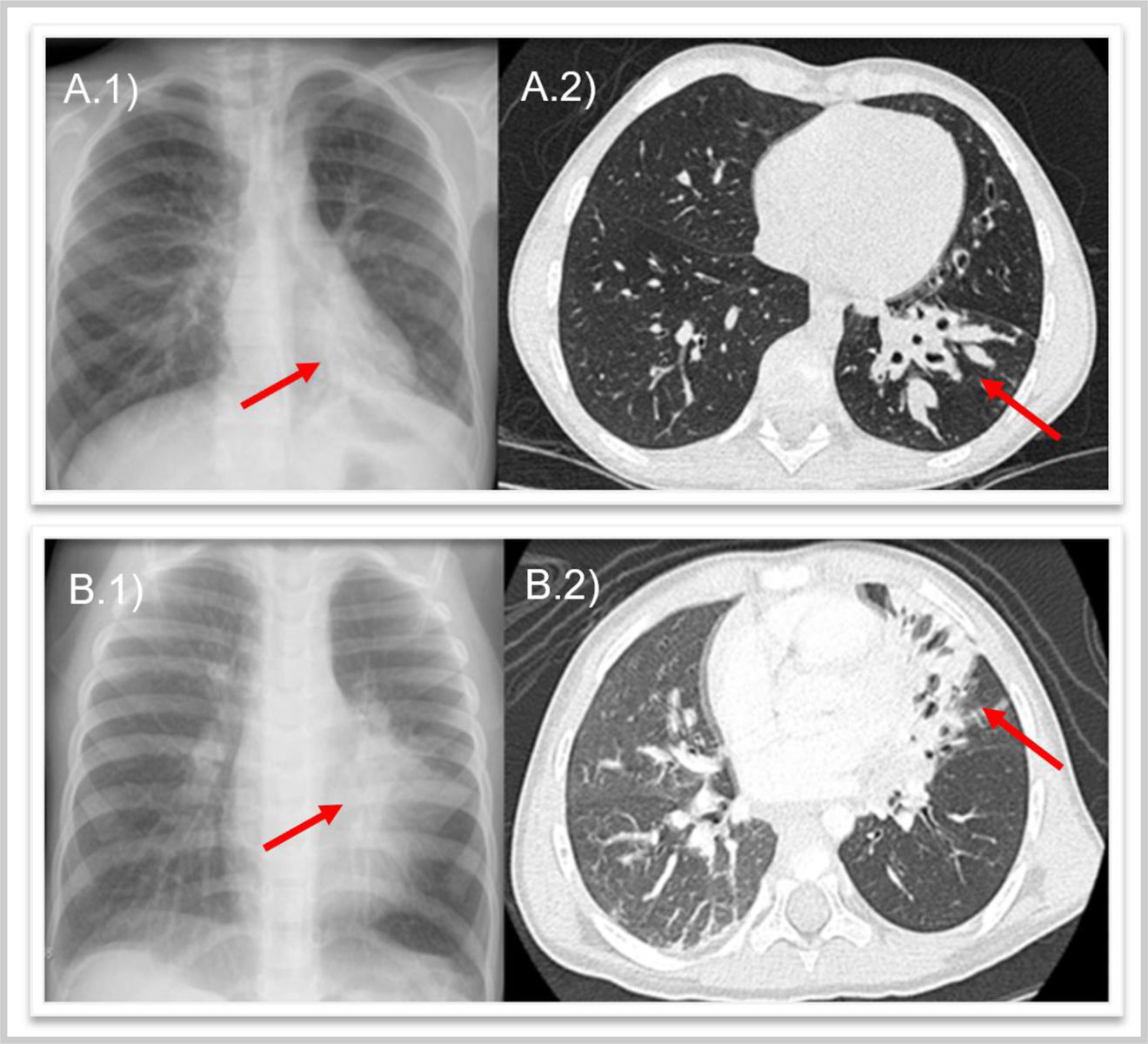
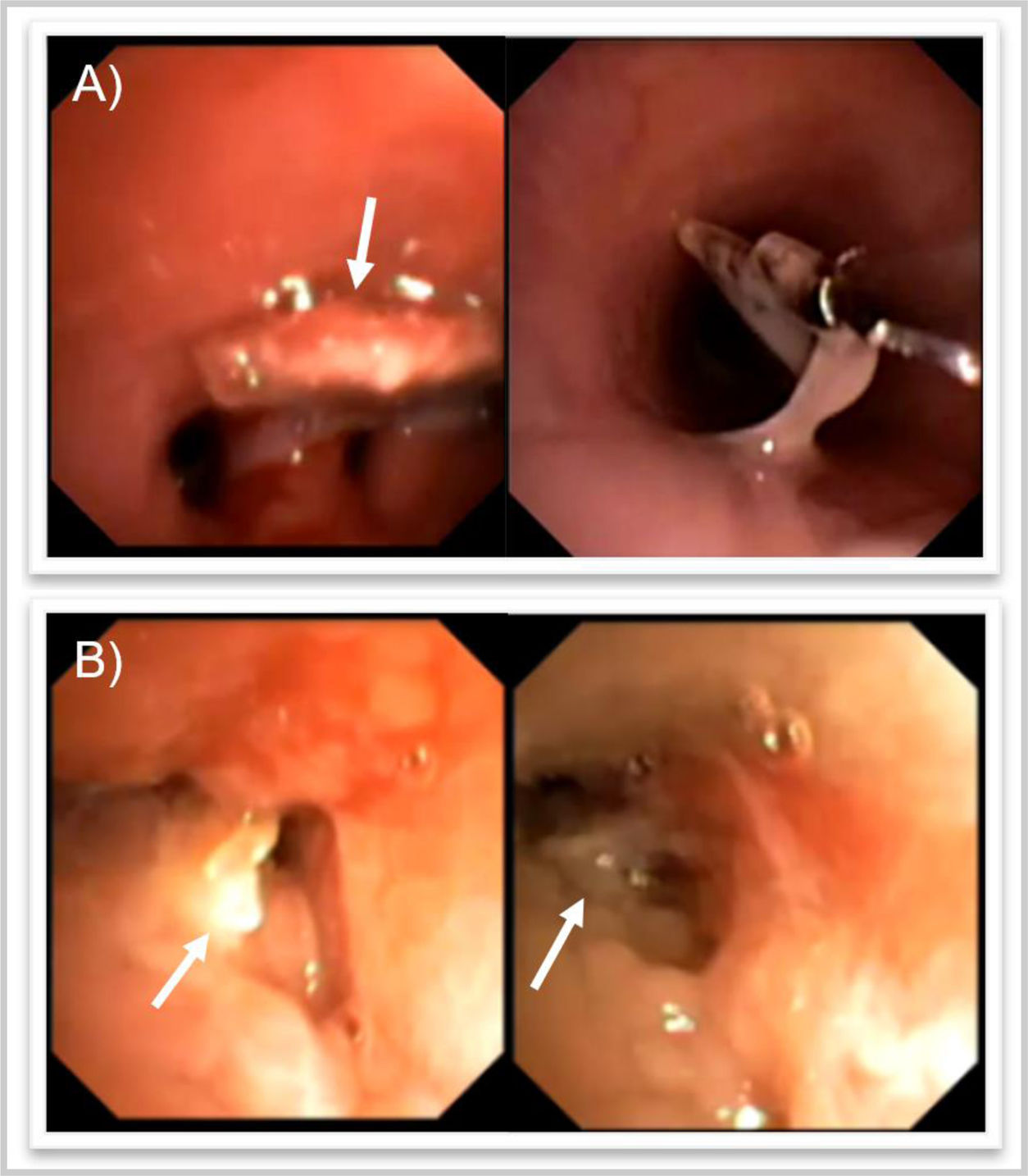
Case 1 Boy aged 8 years with an unremarkable history presenting with productive cough of one year’s duration and chronic left lower lobe (LLL) atelectasis observed in chest X-rays (Rx) and bronchiectasis with bronchial wall thickening and mucous content in the chest CT scan (Fig. 1). The patient underwent flexible bronchoscopy, with visualization of an intrabronchial foreign body (FB) in the LLL that was removed in the same procedure (Fig. 2; Appendix B video) and turned out to be a sunflower hull. (A) Case 1: (1) chest X-ray showing atelectasis of the left lower lobe (red arrow), (2) computed tomography showing bronchiectasis in the left lower lobe (red arrow). (B) Case 2: (1) chest X-ray showing infiltration of left paracardiac region (red arrow), (2) computed tomography showing atelectasis in the lingula and bronchiectasis (red arrow). Boy aged 2 years, previously healthy, who abruptly started coughing blood while jumping on a trampoline. The chest Rx revealed infiltration in the left paracardiac region and the chest CT scan a poorly defined mass in the left main bronchus with atelectasis of the lingula and bronchiectasis (Fig. 1). Flexible bronchoscopy allowed visualization of a FB and substantial edema and inflammation of the adjacent mucosa, which precluded its removal (Fig. 2). After administration of intravenous steroids and antibiotherapy, the FO, which was a piece of branch, was removed by rigid bronchoscopy.
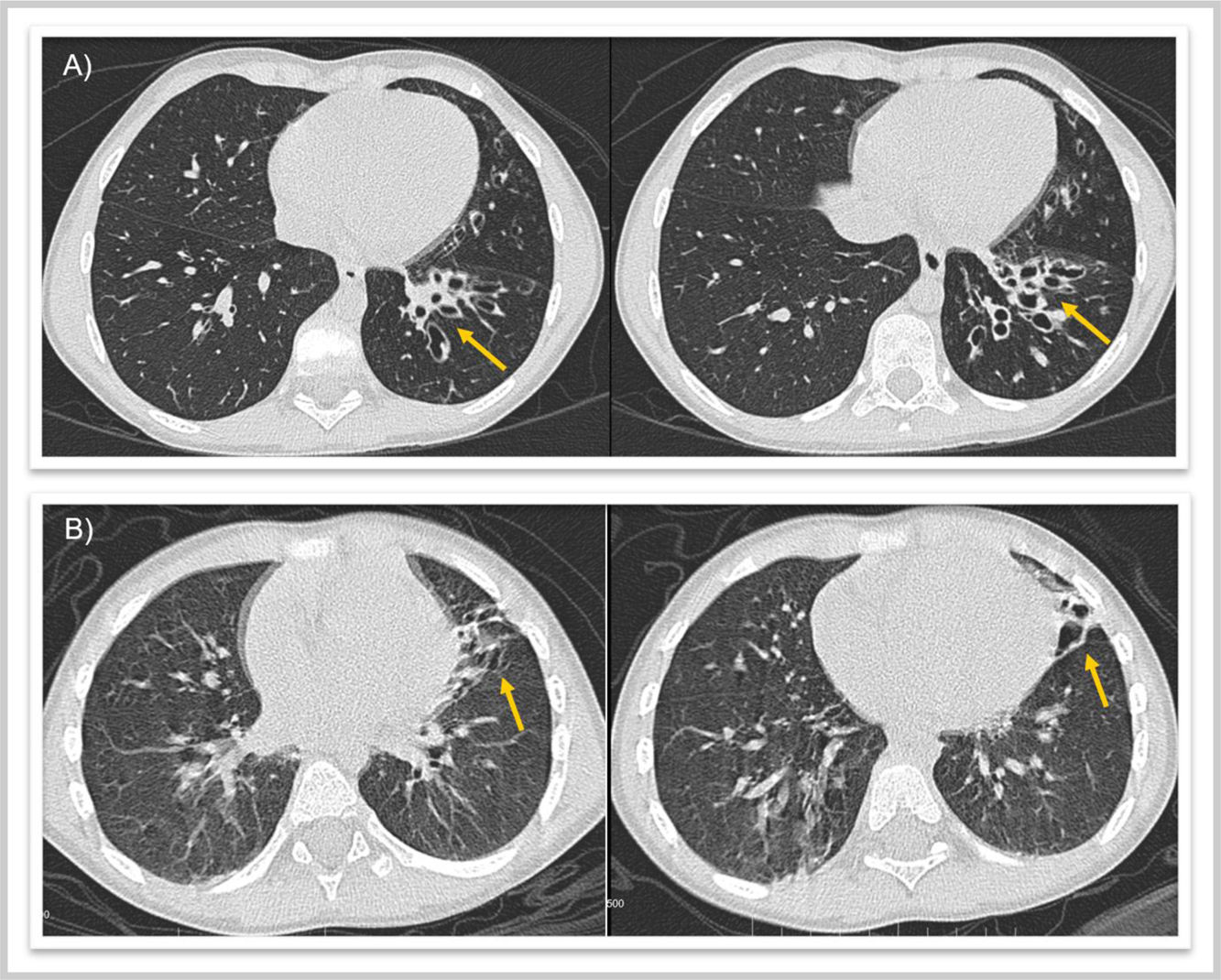
Foreign body aspiration was not suspected in either patient due to the lack of a choking episode, which resulted in delayed diagnosis and the development of bronchiectasis that persisted even five years after removal of the object (Fig. 3).
Organic FBs that linger in the airway for a long time are associated with a stronger inflammatory response, bronchial obstruction and late complications such as pneumonia or bronchiectasis.1–3