A boy aged 5 years presented with left upper extremity (LUE) dysfunction of three weeks’ duration. No history of trauma preceding the onset. The week before, he had experienced an episode of acute bronchitis.
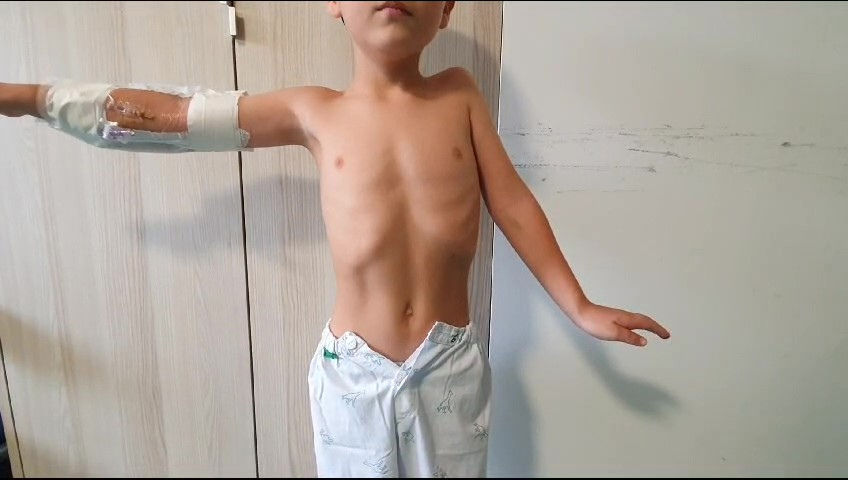
The salient findings in the examination were the inability to raise the LUE and pain on palpation of the left shoulder; unexpectedly, the patient experienced no pain at rest (Fig. 1). Weakness in the left forearm and hand. The rest of the physical examination was normal.
The evaluation included a blood panel, serologic tests for infectious agents, nasopharyngeal aspiration, radiography, an ultrasound scan of the LUE and lumbar puncture, with no relevant findings.
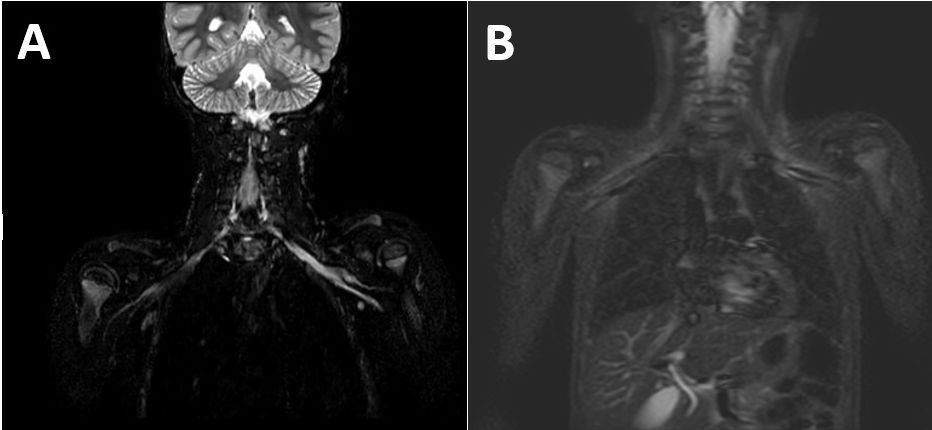
An MRI scan of the head and spine was performed and, due to the unremarkable findings, followed by an MRI scan of the affected area, which revealed edema at the level of the muscles of the rotator cuff and brachial plexus hyperintensity (Fig. 2).
MRI with STIR hyperintensity at the level of the left brachial plexus trunks (A and B), with no discontinuity or associated masses, and signs of acute denervation with mild edema at the supraspinatus and infraspinatus muscles. Normal thickness and signal intensity in cervical spinal cord, with no evidence of space-occupying lesions in the spinal canal. Normal morphology, alignment and signal intensity in vertebral bodies, posterior elements and intervertebral discs.
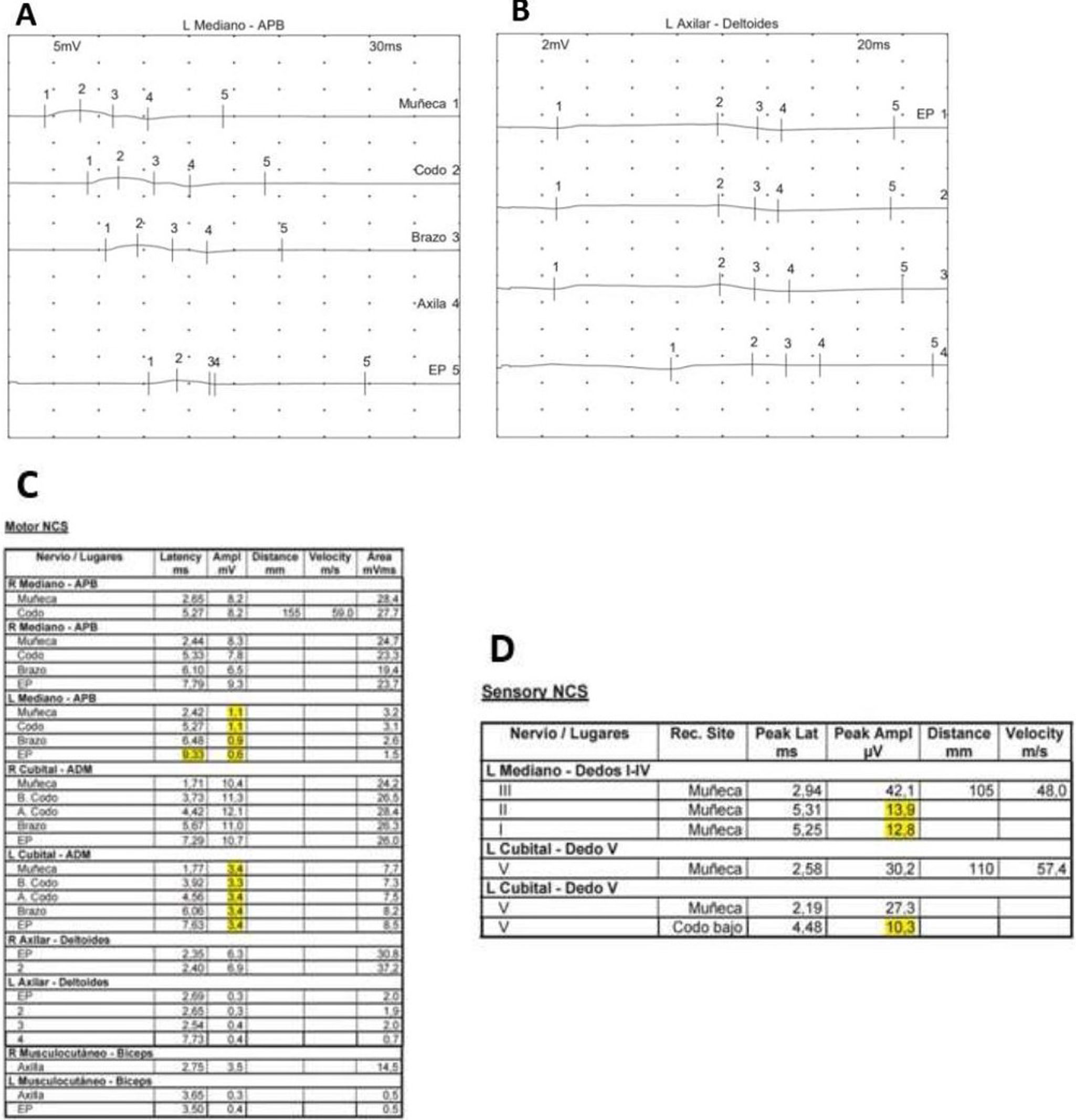
Nerve conduction studies of the LUE evinced left-sided acute pan brachial plexopathy with greater involvement of the upper trunk and axonotmesis in the median and distal ulnar nerves with reduced axonal amplitude. The needle electrode examination was inconclusive, with absence of fibrillation and fasciculation potentials (Fig. 3).
(C) The motor nerve conduction study assessed the axillary (B), musculocutaneous, median (A) and ulnar nerves on both sides, with stimulation at Erb point, arm, elbow and wrist, with recording electrodes placed at the deltoid, biceps, abductor pollicis brevis and abductor digiti minimi muscles, showing a late response of the median nerve to stimulation of Erb point. (D) The sensory nerve conduction study assessed the left median nerve at the level of the third digit and the left ulnar nerve at the level of the fifth digit. We obtained reduced amplitude values in the normal range on distal stimulation at the wrist, and significant reduction on stimulation at the elbow (axonal degeneration reached the elbow, but not the wrist). The electrophysiological findings were compatible with acute left pan brachial plexopathy with predominant involvement of the upper trunk and axonotmesis of the median and distal ulnar nerves.
The combination of electrodiagnostic, clinical and magnetic resonance features were compatible with Parsonage-Turner sydrome,1 a disease that is rare in the pediatric age group.2
The patient started rehabilitation and treatment with oral anti-inflamatories,3 and has exhibited progressive, albeit slow, improvement to date (one year of follow-up).