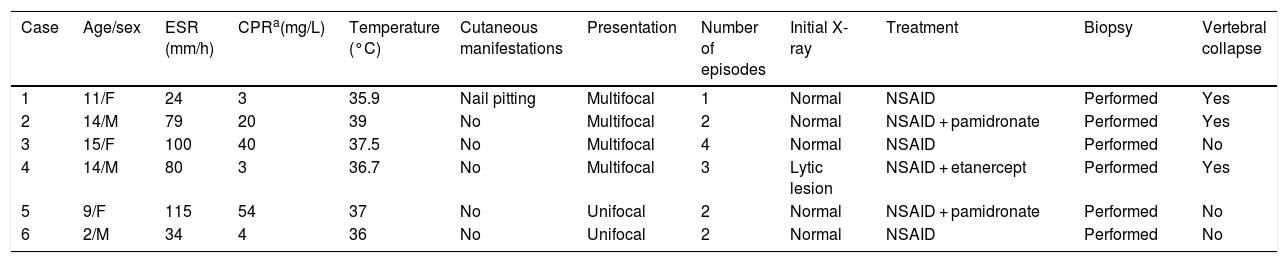
We present 6 cases of chronic recurrent multifocal osteomyelitis (CRMO) in a cohort of children and adolescents; the clinical and demographic characteristics of the cases are summarised in Table 1, and radiological images can be found in Fig. 1. The patients presented with insidious bone or joint pain associated with local swelling, warmth and tenderness at the affected site and functional impairment.
Characteristics of the cohort.
| Case | Age/sex | ESR (mm/h) | CPRa(mg/L) | Temperature (°C) | Cutaneous manifestations | Presentation | Number of episodes | Initial X-ray | Treatment | Biopsy | Vertebral collapse |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 11/F | 24 | 3 | 35.9 | Nail pitting | Multifocal | 1 | Normal | NSAID | Performed | Yes |
| 2 | 14/M | 79 | 20 | 39 | No | Multifocal | 2 | Normal | NSAID + pamidronate | Performed | Yes |
| 3 | 15/F | 100 | 40 | 37.5 | No | Multifocal | 4 | Normal | NSAID | Performed | No |
| 4 | 14/M | 80 | 3 | 36.7 | No | Multifocal | 3 | Lytic lesion | NSAID + etanercept | Performed | Yes |
| 5 | 9/F | 115 | 54 | 37 | No | Unifocal | 2 | Normal | NSAID + pamidronate | Performed | No |
| 6 | 2/M | 34 | 4 | 36 | No | Unifocal | 2 | Normal | NSAID | Performed | No |
CPR, C-reactive protein; ESR, erythrocyte sedimentation rate; F, female; M, male; NSAID, nonsteroidal anti-inflammatory drug.
(A and B) Boy aged 2 years who presented with pain and signs of local inflammation in the right lower extremity with mild elevation of the ESR (34 mm/h) y la CPR (4 mg/L). (A) The initial MRI detected metaphyseal and diaphyseal oedema in the right tibia (arrow). A pathogen was not isolated, and the disease was classified as bacterial osteomyelitis of unknown aetiology. (B) Five months later, he had a similar episode in the left lower extremity, and the MRI scan revealed metaphyseal and diaphyseal oedema in the left tibia (arrow), leading to diagnosis of CRMO. (C–E) Girl aged 11 years who presented with pain and local inflammatory signs in the right lower extremity with mild elevation of the ESR (24 mm/h) and CPR level (3 mg/L). History of back pain of one year’s duration. The short tau inversion recovery (STIR) whole body MRI images revealed multiple foci of bony oedema: in the tibial metaphysis (arrows in C), in the body of T7 (arrow in D), and in the posterior wall acetabulum (arrow in E). (F–K) Male adolescent aged 14 years who presented with pain and signs of local inflammation in the left lower extremity and mild elevation of the ESR (80 mm/h) and CPR (3 mg/L). (F) The initial anteroposterior radiograph detected an eccentric lytic lesion adjacent to the physis at the level of the metaphysis of the distal tibia (arrow), with a discontinuous periosteal reaction (arrowhead). (G) Five months later, the lesion had decreased in size (arrow) and the periosteal reaction was continuous (arrowhead). (H) Two years later, the lesion had resolved with minimum residual bone sclerosis (arrow). (I) MRI at diagnosis with visualization of a transphyseal lesion: hypointense in T1-weighted images (arrow) and (J) hyperintense in T2-weighted images (arrow). (K) Intense enhancement of the bony lesion and surrounding soft tissues (arrow).
One of the patients had nail pitting secondary to psoriasis, which was diagnosed before CRMO. Another patient had fever of up to 39 °C. The rest did not present with constitutional symptoms, with a mean temperature at diagnosis of 37.1 °C.
Four patients had multifocal disease and 2 unifocal disease. Four experienced recurrences at the original site and 1 at a different site (Fig. 1, A and B), and one did not experience recurrence.
In every case, the results of laboratory tests at diagnosis were normal, with the exception of mild elevation of the erythrocyte sedimentation rate (ESR) and C-reactive protein (CPR), with mean values of 72 mm/h and 21 mg/L, respectively.
The initial radiographs were also normal in every case but one, in which a radiographic pattern indicative of aggressive disease was identified at the distal tibial metaphysis (Fig. 1, F–K).
All patients underwent a bone biopsy guided by computed tomography (CT) and a magnetic resonance imaging (MRI) scan of the involved regions. The findings ruled out infectious or malignant disease in every case and evinced mild inflammatory changes in the bone marrow. Four patients also underwent a whole body MRI scan (Fig. 1, C–E), which evinced vertebral involvement in all and vertebral collapse in 3.
Three patients received an initial diagnosis of bacterial osteomyelitis of unknown aetiology and empiric antibiotherapy until CRMO was diagnosed. In 3 patients, treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) achieved remission, while another 3 required second-line treatment: 2 with pamidronate and 1 with etanercept.
Chronic recurrent multifocal osteomyelitis is an autoinflammatory disease of bone that develops in children and adolescents.1 Comorbidities such as psoriasis, palmar plantar pustulosis, inflammatory bowel disease or inflammatory arthritis may cooccur or precede the diagnosis of CRMO.2 In this case series, one patient presented with nail pitting. Clinically, CRMO is characterised by insidious bone or joint pain in at least one site, with focal swelling, warmth and tenderness, and may cause functional impairment. At onset, the bone changes may be limited to a single location, or there may be multiple foci. Although our series did not include any patients with clavicular involvement, most previous studies agree that clavicular osteomyelitis is suggestive of CRMO.3
Symptoms may recur or remit, and fewer than 5% of affected patients have constitutional symptoms, like weight loss or fever.2 In agreement with the previous literature, the laboratory values at diagnosis of CRMO were normal or there was mild elevation of the ESR and CPR levels.2
There are no universally accepted criteria for the diagnosis of CRMO, although some have been proposed (Bristol criteria, Jansson criteria),4,5 and it continues to be a diagnosis of exclusion, chiefly through ruling out malignant disease and infection.1
Plain radiography is frequently the initial imaging modality used in the diagnosis of CRMO in the early stages, but it usually does not detect specific pathological features. When present, they tend to be focal metaphyseal lytic lesions,2 which was the case in only one of our patients (Fig. 1). Magnetic resonance imaging is particularly sensitive, even in the early stages, and frequently detects the presence of asymptomatic bony oedema and soft tissue changes.2
If the disease is multifocal, unifocal with involvement of the clavicle or recurrent, CRMO should be suspected, and whole-body MRI is the gold standard of diagnosis. Whole-body MRI can detect multifocal involvement and is useful for the assessment of disease activity and to identify potential skeletal complications, such as vertebral fractures or bony deformities due to premature physeal closure.4 In our series, half the patients experienced vertebral collapse during the course of disease. This highlights the importance of appropriate diagnosis, treatment and follow-up in these patients. Lastly, several studies show that at present, a bone biopsy is performed in 70%–80% of patients,2 particularly in those with unifocal involvement and atypical location of disease, early onset (age <2 years) or atypical response to treatment.5 However, in our case series, a biopsy was performed in every patient to rule out alternative diagnoses. In children presenting with unifocal pain, the differential diagnosis is broad, and CRMO should be considered when biopsy findings and blood culture results rule out infection and malignant disease.