Breastfeeding (BF) offers multiple short-and long-term health benefits to preterm and ill infants. Therefore, BF support should be apriority in neonatal intensive care units (NICUs).
The European Standards of Care for Newborn Health1 and the Eight principles for patient-centred and family-centred care for newborns in the neonatal intensive care unit have been published recently.2 Both documents include BF support as an essential intervention. In addition, they highlight the need to establish enteral feeding with human milk early on, supporting mothers before, during and after the hospital stay in adherence with the 3 guiding principles and the 10 steps of the Baby-friendly Hospital Initiative for Neonatal Wards (Neo-BFHI).3 On the other hand, the rate of BF at discharge from the neonatal unit is considered a key indicator of the quality of care.4
In order to assess the current situation and the progress in recent years in the introduction of specific measures for BF support in NICUs in Spain, we compared the responses given by level III NICUs in 2 nationwide surveys carried out in 20135 and 2018.
The questionnaires included questions regarding: (1) BFHI accreditation (any phase); (2) systematic training of health care staff on BF; (3) antenatal information provided to hospitalised pregnant women (generally); (4) recommended timing to start breast milk pumping (<6 hours); (5) initiation of feedings in very preterm infants (<6 hours); 6) protocol for handling of human milk; (7) availability of freezers in the NICU.
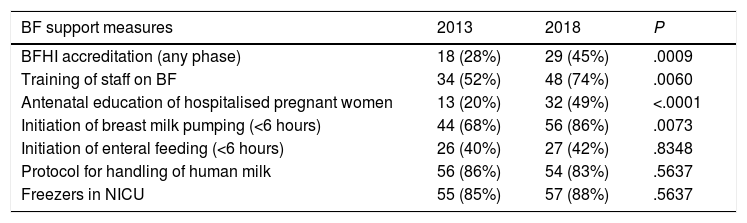
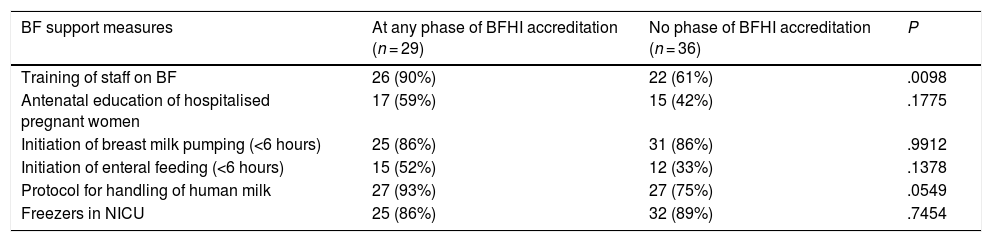
The response rate was 97% (77/79) in 2013 and 87% (65/77) in 2018, and 65 NICUs responded in both periods. We compared the responses at each time point of the NICUs that participated in both periods and also the responses of the units that participated in the 2018 survey based on their BFHI accreditation phase. Tables 1 and 2 present the results of these comparisons.
Breastfeeding support measures, comparison of paired data for neonatal intensive care units that participated in both the 2013 and the 2018 surveys (N = 65).
| BF support measures | 2013 | 2018 | P |
|---|---|---|---|
| BFHI accreditation (any phase) | 18 (28%) | 29 (45%) | .0009 |
| Training of staff on BF | 34 (52%) | 48 (74%) | .0060 |
| Antenatal education of hospitalised pregnant women | 13 (20%) | 32 (49%) | <.0001 |
| Initiation of breast milk pumping (<6 hours) | 44 (68%) | 56 (86%) | .0073 |
| Initiation of enteral feeding (<6 hours) | 26 (40%) | 27 (42%) | .8348 |
| Protocol for handling of human milk | 56 (86%) | 54 (83%) | .5637 |
| Freezers in NICU | 55 (85%) | 57 (88%) | .5637 |
BF, breastfeeding; BFHI, baby-friendly hospital initiative; NICU, neonatal intensive care unit.
Breastfeeding support measures, comparison of neonatal intensive care units that participated in 2018 based on BFHI accreditation phase.
| BF support measures | At any phase of BFHI accreditation (n = 29) | No phase of BFHI accreditation (n = 36) | P |
|---|---|---|---|
| Training of staff on BF | 26 (90%) | 22 (61%) | .0098 |
| Antenatal education of hospitalised pregnant women | 17 (59%) | 15 (42%) | .1775 |
| Initiation of breast milk pumping (<6 hours) | 25 (86%) | 31 (86%) | .9912 |
| Initiation of enteral feeding (<6 hours) | 15 (52%) | 12 (33%) | .1378 |
| Protocol for handling of human milk | 27 (93%) | 27 (75%) | .0549 |
| Freezers in NICU | 25 (86%) | 32 (89%) | .7454 |
BF, breastfeeding; BFHI, baby-friendly hospital initiative; NICU, neonatal intensive care unit.
We found that the implementation of most of the BF support measures under study had improved significantly in the past 5 years in Spanish NICUs. Nevertheless, there are still many opportunities for improvement, mainly as regards antenatal education on BF of hospitalised mothers and early initiation of enteral feedings with human milk. An interesting finding in our study was that while 86% of units recommended pumping of breastmilk from an early stage, only 42% initiated enteral feedings with human milk in very preterm infants within 6 h of birth.
On the other hand, when we compared the 2018 results based on the phase of BFHI accreditation we found that more units in the group of units at some phase in the BFHI accreditation pathway trained their health care staff on BF. A previous study5 found that NICUs with BFHI accreditation or in the process of being accredited had better implementation of measures to promote and support BF compared to units that had not started the accreditation process.
In short, our study, of a national scope, detected significant changes through time. It also identified opportunities for improvement that could help prioritise the particular needs of Spanish NICUs as regards BF support.
We thank all the neonatal intensive care units that participated in the study.
Please cite this article as: Alonso Díaz C, Morales Betancourt C, de la Cruz Bertolo J, López Maestro M, Vázquez Román S. Cambio en las prácticas de apoyo a la lactancia materna en unidades neonatales españolas. An Pediatr (Barc). 2020;93:123–124.