In Spain, children and their families make frequent use of paediatric emergency departments (PEDs).1,2 The Sociedad Española de Urgencias de Pediatría (Spanish Society of Paediatric Emergency Medicine, SEUP) promotes excellence in education in emergency care, demanding that the acquisition of certain competencies and skills by paediatricians-in-training (medical intern-resident programme, MIR) to be guaranteed. In 2012, the SEUP developed an educational curriculum and established training in the context of the MIR as a strategic plan. In 2015, the Research Network of the SEUP approved the performance of a study to assess the training in emergency care received by paediatrics MIR residents in Spain. The primary objective of the study was to analyse the training in emergency care received by paediatrics residents, and the secondary objective was to identify factors associated with an increased satisfaction of MIR residents with the training received.
In the second semester of 2016, we conducted a cross-sectional observational study approved by the Ethics Committee of the Valladolid Oeste Health Area based on survey data obtained through submission of one online questionnaire to the heads of the PEDs and submission of another questionnaire to the paediatrics residents of hospitals members of the SEUP offering MIR residency programmes in paediatrics. We analysed the training received on the subject of emergency care, both during the rotation in the emergency department and in the after-hours urgent primary care setting. We included in the analysis those hospitals for which we received responses from at least 33% of the paediatrics residents. We performed a multivariate analysis to identify the variables associated with greater satisfaction in residents.
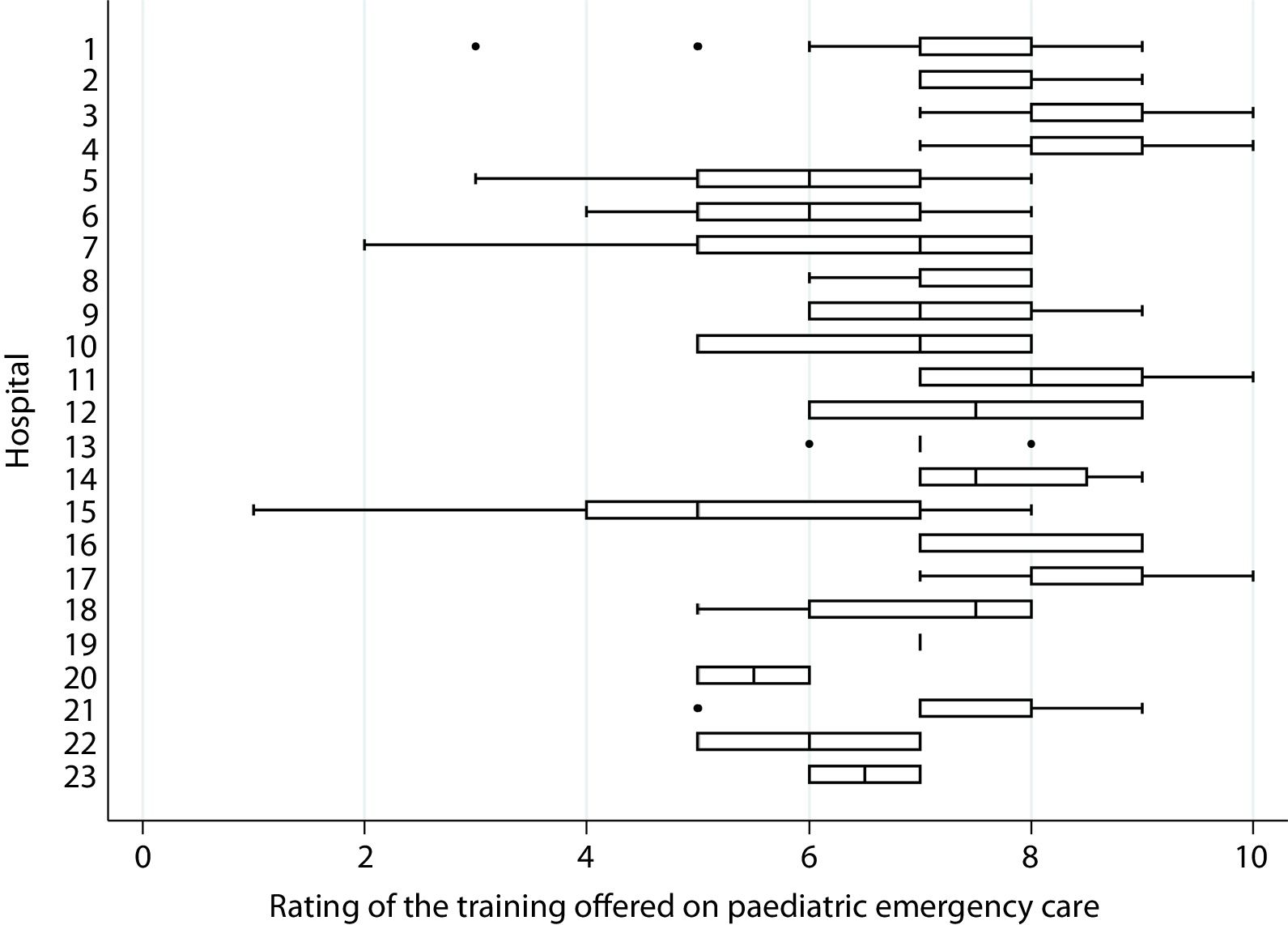
We included the responses of the heads of 23 PEDs and 198 MIR residents in those hospitals (year 2, 32.3%; year 3, 37.4%; year 4, 30.3%). Of the 23 department heads, 6 (26.1%) reported that their department had a designated staff member responsible for managing the training programme, 12 (52.2%) that it used quality indicators (QI) to assess the quality of training, and 17 (73.9%) that it had an established training curriculum, while 20 departments (86.9%) performed some form of evaluation of the residents’ clinical work. In the PEDs where the department head answered each of these questions in the affirmative, 28.7% of the residents were unaware that there was a designated staff member in charge of training, 70.6% were unaware of the existence of QIs, 42.3% believed there was no established curriculum and 14.8% reported that their performance was not evaluated in any way, respectively. Table 1 shows the level of supervision of the clinical work of MIR residents in participating PEDs. In rating their satisfaction with the training received, the median score given by residents was 7 out of 10 (IQR, 7–8; interhospital range, 5–9) (Fig. 1). Direct supervision at the bedside of the clinical work of the resident (ß: –4.01; 95% CI, –6.75 to –1.27) and awareness of the application of training QIs (ß: 0.9; 95% CI, 0.37 a 1.44) were independently associated with a greater satisfaction of MIR residents with the training received.
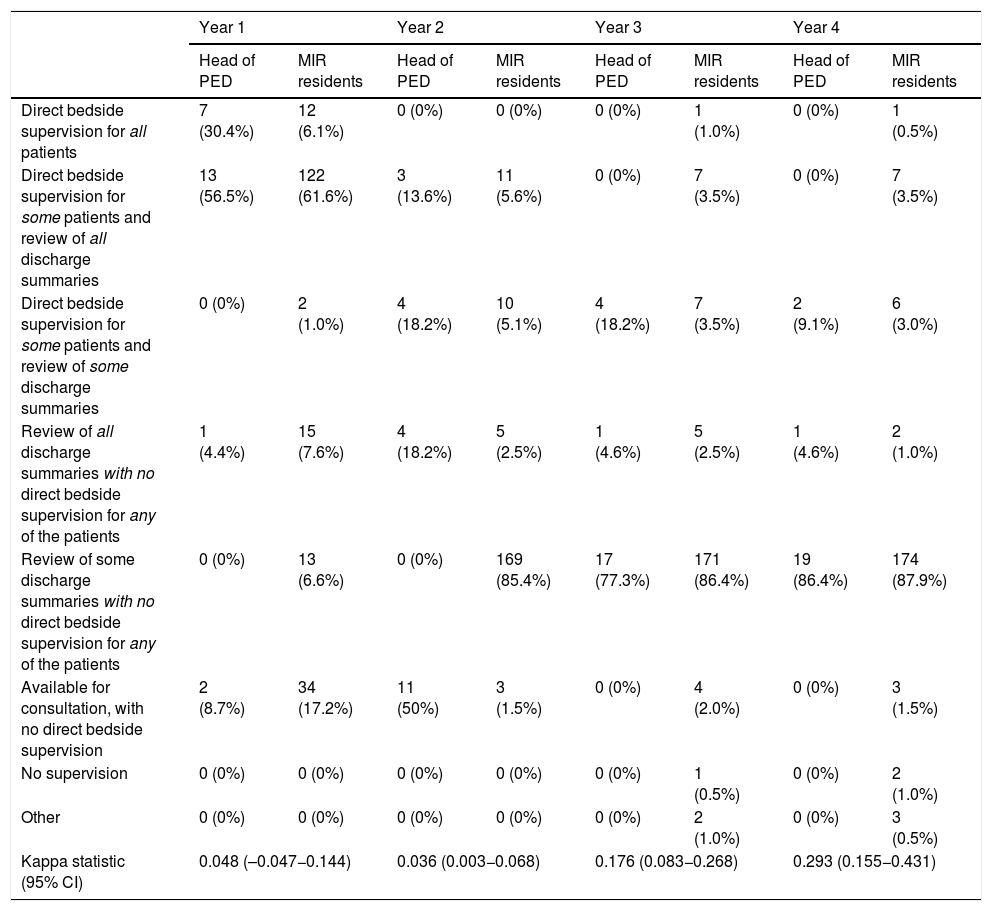
Level of supervision reported by the heads of the paediatric emergency departments and the medical residents (all residents provided information about the level of supervision in each of the 4 years of residency).
| Year 1 | Year 2 | Year 3 | Year 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Head of PED | MIR residents | Head of PED | MIR residents | Head of PED | MIR residents | Head of PED | MIR residents | |
| Direct bedside supervision for all patients | 7 (30.4%) | 12 (6.1%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1.0%) | 0 (0%) | 1 (0.5%) |
| Direct bedside supervision for some patients and review of all discharge summaries | 13 (56.5%) | 122 (61.6%) | 3 (13.6%) | 11 (5.6%) | 0 (0%) | 7 (3.5%) | 0 (0%) | 7 (3.5%) |
| Direct bedside supervision for some patients and review of some discharge summaries | 0 (0%) | 2 (1.0%) | 4 (18.2%) | 10 (5.1%) | 4 (18.2%) | 7 (3.5%) | 2 (9.1%) | 6 (3.0%) |
| Review of all discharge summaries with no direct bedside supervision for any of the patients | 1 (4.4%) | 15 (7.6%) | 4 (18.2%) | 5 (2.5%) | 1 (4.6%) | 5 (2.5%) | 1 (4.6%) | 2 (1.0%) |
| Review of some discharge summaries with no direct bedside supervision for any of the patients | 0 (0%) | 13 (6.6%) | 0 (0%) | 169 (85.4%) | 17 (77.3%) | 171 (86.4%) | 19 (86.4%) | 174 (87.9%) |
| Available for consultation, with no direct bedside supervision | 2 (8.7%) | 34 (17.2%) | 11 (50%) | 3 (1.5%) | 0 (0%) | 4 (2.0%) | 0 (0%) | 3 (1.5%) |
| No supervision | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.5%) | 0 (0%) | 2 (1.0%) |
| Other | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (1.0%) | 0 (0%) | 3 (0.5%) |
| Kappa statistic (95% CI) | 0.048 (–0.047−0.144) | 0.036 (0.003−0.068) | 0.176 (0.083−0.268) | 0.293 (0.155−0.431) | ||||
Data expressed as n (%).
Kappa statistic for the comparison of the answers of department heads and the medical interns, 0.275 (95% CI, 0.237−0.314), with a significant increase with each year of residency.
CI, confidence interval; IQR, interquartile range; PED, paediatric emergency department.
Rating of the training offered in the paediatric emergency department in each hospital.
The training was rated from 0 to 10, with 0 indicating the lowest satisfaction and 10 the highest. The left and right sides of the boxes correspond to the 25th (P25) and 75th (P75) percentiles and the central line represents median. The left whisker indicates the lowest value in the interval P25–1.5 × IQR. The right whisker indicates the highest value in the interval P75 + 1.5 × IQR.
In Spain, the training in emergency care of residents in paediatrics is very heterogeneous, and we identified significant areas for improvement. Among the most important are that few PEDs had a designated staff member in charge of the training programme to put forward educational activities to promote the acquisition of skills and competencies specific to emergency care.3 Furthermore, approximately half of the PEDs did not use QIs to assess training outcomes. On the other hand, the level of supervision offered to residents decreased progressively throughout the residency programme, but not as gradually as would be expected. The association of the level of supervision with the greater satisfaction of MIR residents with their training highlights the importance of bedside teaching. Nevertheless, the residents reported considerable satisfaction with the training received, possibly because they appreciate the efforts devoted to its improvement, such as the educational curriculum developed by the SEUP and accepted and adapted by most of the PEDs affiliated to the society, and because most PEDs carried out some form of evaluation of the performance of the MIR residents. However, it is also important to consider the significant variation between departments in the level of satisfaction of the residents, and the fact that a sizeable percentage of the residents were not aware of the existence of a training curriculum, the specific staff member in charge of training or the use of QIs. There are several limitations to our study. We did not get a response from the head of every PED affiliated to the SEUP, which may have resulted in overrepresentation in the survey of departments with a greater interest in training. Furthermore, not all PEDs of hospitals offering residencies in paediatrics are affiliated to the SEUP, which ought to be taking into account on extrapolating our findings to other emergency departments. However, we believe that the areas in need of improvement identified in our study may be applicable to most PEDs in Spain.
The training received by Spanish MIR residents is widely heterogeneous and we identified several areas that could be significantly improved. The SEUP and the different PEDs should take these findings into account to develop strategies aimed at standardising and improving residency training.
Carles Luaces (Paediatric Emergency Department, Hospital Universitario Sant Joan de Deu, Barcelona); Mercedes de la Torre (Paediatric Emergency Department, Hospital Universitario Niño Jesús, Madrid); Sebastià González (Paediatric Emergency Department, Hospital Universitario Vall d’Hebron, Barcelona); Javier Benito (Paediatric Emergency Department. Hospital Universitario de Cruces, Barakaldo); Paula Vázquez (Paediatric Emergency Department, Hospital General Universitario Gregorio Marañón, Madrid); Izaskun Olaciregui (Paediatric Emergency Department, Hospital Universitario Donostia, San Sebastian); Carmen Campos (Paediatric Emergency Department, Hospital Universitario Miguel Servet, Zaragoza); Sandra Moya (Paediatric Emergency Department, Hospital Universitario Parc Taulí, Sabadell); Andrés González (Paediatric Emergency Department, Hospital Universitario Basurto, Bilbao); Carmen Vázquez (Paediatric Emergency Department, Hospital Universitario Ramón y Cajal, Madrid); Olga Serrano (Paediatric Emergency Department, Hospital Universitario de Salamanca, Salamanca); Carlos M. Angelats (Paediatric Emergency Department, Hospital Universitario Francesc de Borja, Gandía); Ramón Fernández (Paediatric Emergency Department, Hospital Universitario Cabueñes, Gijón); Jerónimo J. Pardo (Paediatric Emergency Department, Hospital Universitario A Coruña, La Coruña); Ester Castellarnau (Paediatric Emergency Department, Hospital Universitario Joan XXIII, Tarragona); Esther Ballester (Paediatric Emergency Department, Hospital Universitario Dr. Peset, Valencia); Lizar Aguirre (Paediatric Emergency Department, Hospital Universitario Txagorritxu, Vitoria); Abel Martínez (Paediatric Emergency Department, Hospital Universitario Tarrassa, Tarrassa); Neus Pociello (Paediatric Emergency Department, Hospital Universitario Arnau de Vilanova, Lleida); Maria A. García (Paediatric Emergency Department, Hospital Universitario Príncipe de Asturias, Alcalá de Henares); Miriam Gutiérrez (Paediatric Emergency Department, Hospital Universitario Burgos, Burgos); Pau Ventosa (Paediatric Emergency Department, Hospital Universitario General de Catalunya, Sant Cugat del Valles).
All of them submitted the initial questionnaire and collected data for the study in their respective hospitals.
Please cite this article as: Velasco R, Mintegi S. Evaluación de la formación en urgencias por parte de los médicos internos residentes de pediatría en España. An Pediatr (Barc). 2020;93:124–127.
The members of the Training Working Group of the Research Network of the Spanish Society of Pediatric Emergencies (RISeuP-SPERG) are presented in Appendix A.