Acute appendicitis (AA) is the most common abdominal surgical emergency. No specific studies have been found that evaluate the impact of the coronavirus 2 (SARS-Cov-2) pandemic on AA and its surgical management. An analysis was made on the influence of this new pathology on the clinical course of AA.
Material and methodsRetrospective observational study was conducted on patients operated on for AA from January to April 2020. They were classified according to the time of the appendectomy, before the declaration of the state of alarm (Pre-COVID-19), and after its declaration (Post-COVID-19) in Spain, one the most affected countries in the world. An evaluation was made of demographic variables, duration of symptoms, type of appendicitis, surgical time, hospital stay, and postoperative complications.
ResultsThe study included 66 patients (41 Pre-COVID-19; 25 Post-COVID-19) with mean age of 10.7 ± 3 and 9.3 ± 3.1; P = .073, respectively. Fever was found in a higher number of post-COVID-19 patients (52 vs 19.5%; P = .013), as well as a higher CRP (72.7 ± 96.2 vs 31.3 ± 36.2 mg/dL; P = .042). This group presented with a higher proportion of complicated appendicitis when compared to Pre-COVID-19 (32 vs 7.3%; P = .015). The mean hospital stay was longer in the Post-COVID-19 group (5.6 ± 5.9 vs 3.2 ± 4.3 days; P = .041). No differences were found in the time of onset of symptoms or surgical time.
ConclusionsThe SARS-Cov-2 pandemic influenced the time of diagnosis of appendicitis, as well as its course, and mean hospital stay. Peritonitis was more frequently seen. As a result of the significant circumstances, delaying diagnosis and treatment of AA during SARS-Cov-2 pandemic, inappropriate management of this common surgical disorder has been noticed.
La apendicitis aguda (AA) es la urgencia quirúrgica abdominal más frecuente. No encontramos estudios específicos que evalúen el impacto de la pandemia causada por el coronavirus 2 (SARS-Cov-2) sobre la AA y su tratamiento quirúrgico. Analizamos la influencia de esta nueva patología sobre la AA.
Material y métodosEstudio observacional retrospectivo en pacientes intervenidos por AA desde enero hasta abril de 2020. Fueron clasificados según el momento de la apendicectomía, antes de la declaración del estado de alarma (Pre-COVID19) y después de la declaración del estado de alarma (Post-COVID19) en España. Se evaluaron variables demográficas, duración de la sintomatología, tipo de apendicitis, tiempo quirúrgico, estancia hospitalaria y complicaciones postoperatorias.
ResultadosSe incluyeron 66 pacientes (41 Pre-COVID19; 25 Post-COVID19 con edad media de 10.7 ± 3 y 9.3 ± 3.1; P = .073; respectivamente). La fiebre se encontró en un mayor número de pacientes post-COVID19 (52 vs 19.5%; P = .013), así como una PCR más elevada (72.7 ± 96.2 vs 31.3 ± 36.2 mg/dl; P = .042). Este grupo presentó una mayor proporción de apendicitis complicada al compararle con el Pre-COVID19 (32 vs 7.3%; P = .015). La estancia media hospitalaria fue mayor en el grupo Post-COVID19 (5.6 ± 5.9 vs 3.3 ± 4.3 días; P = .041). No se encontraron diferencias en el tiempo de evolución de los síntomas ni en el tiempo quirúrgico.
ConclusionesLa pandemia por SARS-Cov-2 influye en el momento de diagnóstico de la apendicitis, así como en su grado de evolución y estancia hospitalaria. La peritonitis fue lo más frecuentemente observado. Una sospecha y orientación clínica más temprana, es necesaria para evitar un manejo inadecuado de este trastorno quirúrgico común.
Acute appendicitis (AA) is the most frequent surgical emergency in the paediatric population.1,2 Of the children that visit the emergency department with a complaint of acute abdominal pain, 1%–8% receive a diagnosis of AA.3 Delayed diagnosis and delayed initiation of treatment are associated with increased severity of AA.4,5
Early diagnosis and treatment are the best tools to reduce the incidence of complications. Different scores have been developed to estimate the risk of AA, such as the Appendicitis Inflammatory Response (AIR) or the Alvarado score, always used as a complementary tool and not as a means to confirm the diagnosis.6,7
Once AA is confirmed, the most widespread approach among paediatric surgeons is appendectomy, either open or laparoscopic. However, in recent years several studies on the conservative management of uncomplicated acute appendicitis with antibiotherapy have been conducted with promising results, albeit not yet conclusive, so their findings must be interpreted with caution.8,9
Since the emergence of the pandemic brought on by novel coronavirus (SARS-CoV-2), of which the main symptomatic form is an acute respiratory syndrome, all diseases that existed previously now intersect with this new disease context in health care facilities.10 We did not find studies in the literature published to date analysing the impact of the pandemic on acute appendicitis and its surgical management.
The aim of this study was to analyse the impact of the SARS-CoV-2 pandemic on the time elapsed between onset of symptoms and diagnosis of AA and the effect of this delay on disease progression, the surgical approach, the length of stay and postoperative complications in paediatric patients.
Material and methodsStudy designWe conducted a retrospective observational study on paediatric patients with a diagnosis of AA managed in our hospital from January to April 2020.
We classified patients in 2 groups based on the date that the Spanish government declared the state of alarm due to the SARS-CoV-2 pandemic (Royal Decree 463/2020 of 14 March 2020): operated before the declaration of the state of alarm (preCOVID-19) and operated after the declaration of the state of alarm (postCOVID-19).
We included all patients aged less than 18 years that underwent an appendectomy (open or laparoscopic), diagnosed in our hospital or transferred to our hospital from other facilities with suspected or confirmed AA, after obtaining the signed informed consent of their parents or legal guardians. We excluded patients in whom the decision was made to manage the AA conservatively without surgery, those whose parents or guardians refused to consent to surgery, and those for who we were unable to obtain the necessary data for the variables under study.
The approach to surgical management applied in these patients did not differ from the customary approach to AA in our hospital and was the same in both groups.
Data collectionWe obtained data on demographic characteristics, clinical manifestations and results of blood, microbiological and imaging tests from the electronic health records database of the hospital.
We collected information on demographic variables, clinical variables, surgical variables and outcomes.
Statistical analysisWe collected data using Microsoft Excel®, version 16.35, and analysed the variables under study with the software IBM SPSS Statistics® 25.0. We have summarised categorical variables as absolute frequencies and percentages and continuous variables as mean and standard deviation (SD). We assessed the shape of the distribution (normal vs not normal) with the Kolmogorov-Smirnoff (with the Lilliefors correction). We compared categorical data with the χ2 test or the Fisher exact test, and quantitative data with the Student t test (in case of a normal distribution) or the Mann-Whitney U test (otherwise). We defined statistical significance as a P-value of less than .05 and calculated 95% confidence intervals (CIs).
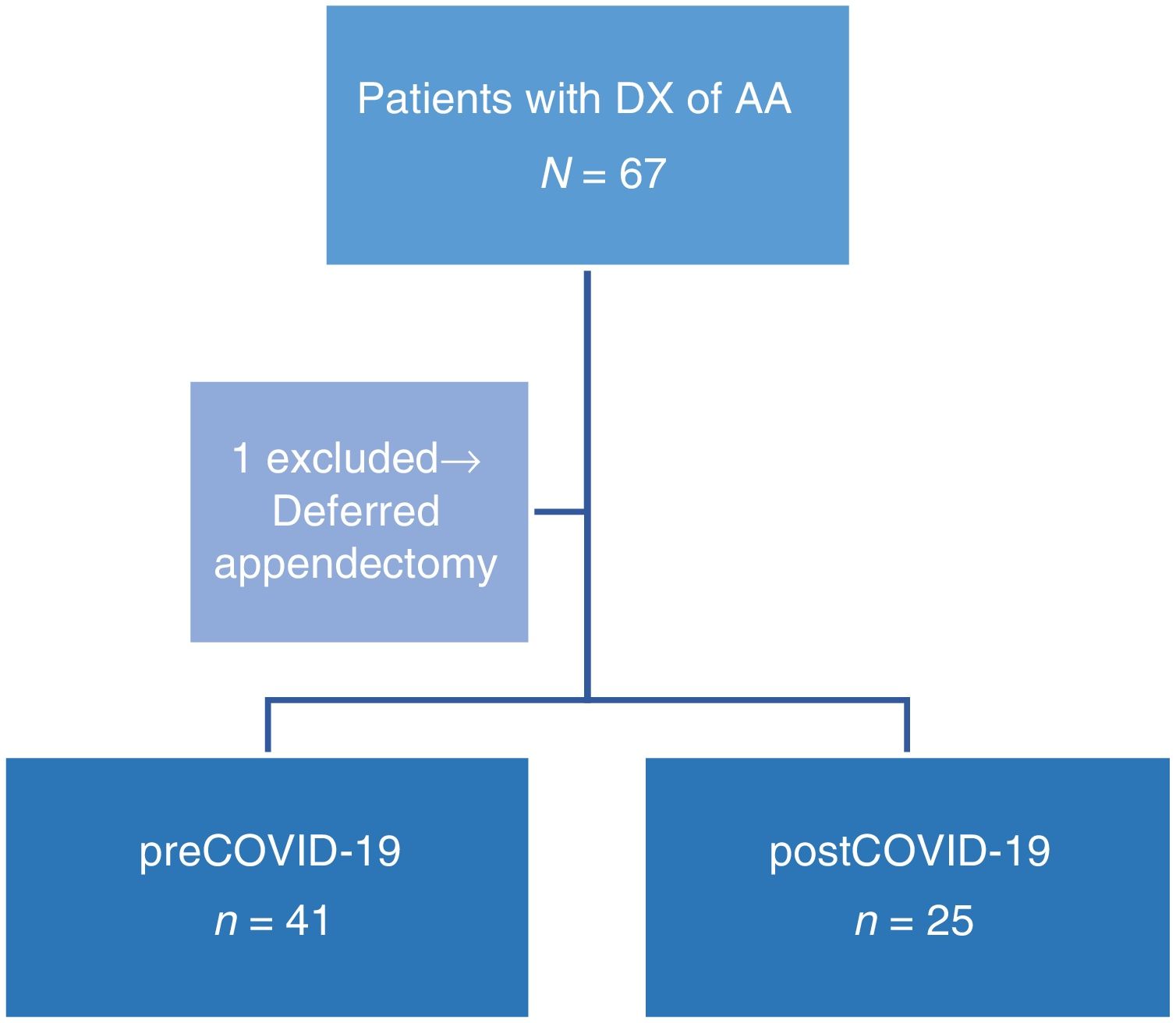
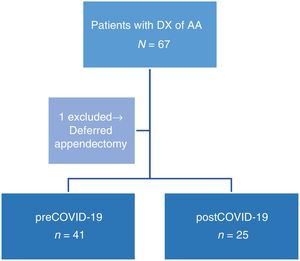
ResultsA total of 66 patients underwent surgery for AA in our hospital between January and April 2020, 41 in the group operated before the declaration of the state of alarm (preCOVID-19) and 25 in the group operated after the declaration of the state of alar (postCOVID-19). We excluded 1 patient in who the chosen approach was conservative, deferring appendectomy (Fig. 1).
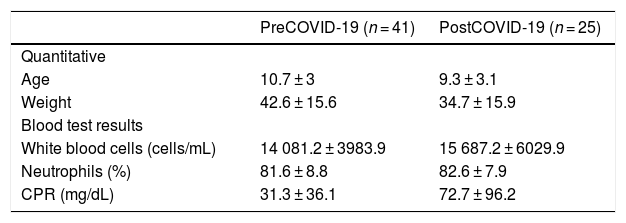
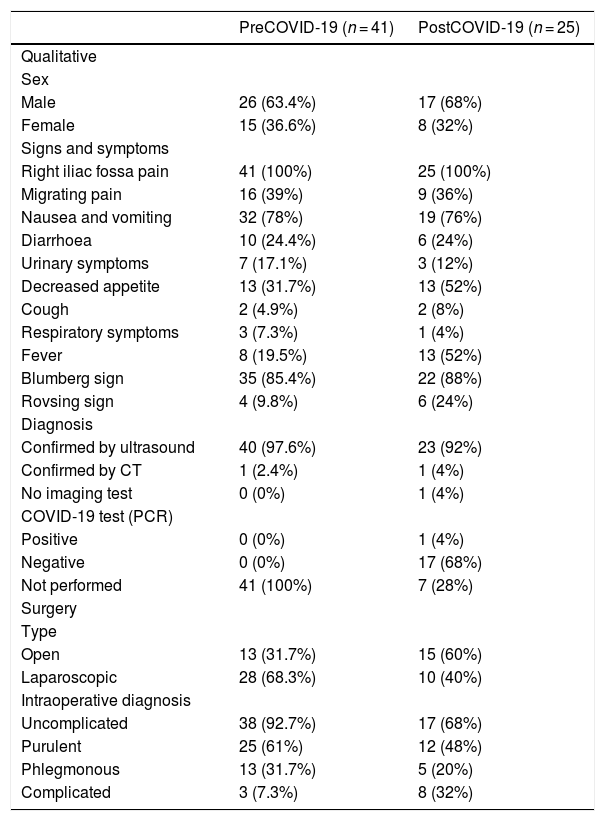
We performed a descriptive analysis of the variables of interest in both groups, the results of which are shown in Tables 1 and 2.
Descriptive analysis of the sample. Quantitative variables.
| PreCOVID-19 (n = 41) | PostCOVID-19 (n = 25) | |
|---|---|---|
| Quantitative | ||
| Age | 10.7 ± 3 | 9.3 ± 3.1 |
| Weight | 42.6 ± 15.6 | 34.7 ± 15.9 |
| Blood test results | ||
| White blood cells (cells/mL) | 14 081.2 ± 3983.9 | 15 687.2 ± 6029.9 |
| Neutrophils (%) | 81.6 ± 8.8 | 82.6 ± 7.9 |
| CPR (mg/dL) | 31.3 ± 36.1 | 72.7 ± 96.2 |
Descriptive analysis of the sample. Quantitative variables. Data expressed as mean ± standard deviation.
Descriptive analysis of the sample. Qualitative variables.
| PreCOVID-19 (n = 41) | PostCOVID-19 (n = 25) | |
|---|---|---|
| Qualitative | ||
| Sex | ||
| Male | 26 (63.4%) | 17 (68%) |
| Female | 15 (36.6%) | 8 (32%) |
| Signs and symptoms | ||
| Right iliac fossa pain | 41 (100%) | 25 (100%) |
| Migrating pain | 16 (39%) | 9 (36%) |
| Nausea and vomiting | 32 (78%) | 19 (76%) |
| Diarrhoea | 10 (24.4%) | 6 (24%) |
| Urinary symptoms | 7 (17.1%) | 3 (12%) |
| Decreased appetite | 13 (31.7%) | 13 (52%) |
| Cough | 2 (4.9%) | 2 (8%) |
| Respiratory symptoms | 3 (7.3%) | 1 (4%) |
| Fever | 8 (19.5%) | 13 (52%) |
| Blumberg sign | 35 (85.4%) | 22 (88%) |
| Rovsing sign | 4 (9.8%) | 6 (24%) |
| Diagnosis | ||
| Confirmed by ultrasound | 40 (97.6%) | 23 (92%) |
| Confirmed by CT | 1 (2.4%) | 1 (4%) |
| No imaging test | 0 (0%) | 1 (4%) |
| COVID-19 test (PCR) | ||
| Positive | 0 (0%) | 1 (4%) |
| Negative | 0 (0%) | 17 (68%) |
| Not performed | 41 (100%) | 7 (28%) |
| Surgery | ||
| Type | ||
| Open | 13 (31.7%) | 15 (60%) |
| Laparoscopic | 28 (68.3%) | 10 (40%) |
| Intraoperative diagnosis | ||
| Uncomplicated | 38 (92.7%) | 17 (68%) |
| Purulent | 25 (61%) | 12 (48%) |
| Phlegmonous | 13 (31.7%) | 5 (20%) |
| Complicated | 3 (7.3%) | 8 (32%) |
Descriptive analysis of the sample. Qualitative variables. Data expressed as absolute frequency (percentage).
We found that the time elapsed was longer in the postCOVID-19 group compared to the preCOVID-19 group, although the difference was not statistically significant (46.1 ± 43.8 h vs 30.2 ± 30.5 h; P = .346). A higher percentage of the postCOVID-19 group had fever compared to the preCOVID-19 group, a difference that was statistically significant, (52% vs 19.5%; P = .013). The same was the case when it came to the serum level of C-reactive protein (CRP), with greater elevation in the postCOVID-19 group (72.7 ± 96.2 mg/dL vs. 31.3 ± 36.2 mg/dL; P = .042).
Stage of AA diagnosed intraoperatively and surgical timeThe number of patients with complicated AA in the form of peritonitis was higher in patients operated after the declaration of the state of alarm compared to those operated before the declaration (32% vs 7.3%; P = .015). We did not find differences in the duration of surgery from the initiation of the incision/incisions to closure of the incision/incisions between the groups (preCOVID-19 group, 53.1 ± 22.1 min vs postCOVID-19 group, 52.5 ± 28.5 min; P > .286).
Mean length of stayWe also analysed the length of stay calculated as the number of days of hospitalization after surgery in the groups of patients based on the date of the declaration of the state of alarm in Spain. The length of stay was longer in the postCOVID-19 group compared to the preCOVID-19 group (5.6 ± 5.9 days vs 3.2 ± 4.3 days; P = .041).
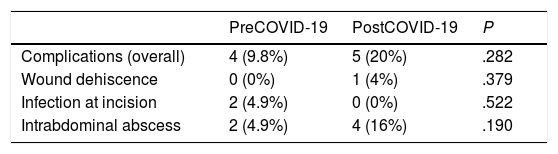
ComplicationsOverall, there were more complications in the postCOVID-19 group compared to the preCOVID-19 group (20% vs 9.8%; P = .239). Table 3 presents the results of this comparison.
DiscussionOur study demonstrated that the appendectomies performed after the declaration of the state of alarm in Spain corresponded to more advanced stages of AA (peritonitis), compared to those performed before the declaration of the state of alarm. This finding was supported by evidence of a longer delay from the onset of symptoms to diagnosis and surgery patients operated after the lockdown started. After analysing the information collected by interviewing parents on arrival to hospital, we surmise that one possible reason for this delay was fear of exposing children to confirmed coronavirus cases in the hospital. We did not analyse these opinions as part of our results, as we had not included this qualitative analysis in the study design.
We also ought to mention that, as reported in several previous studies, infection by SARS-may present with gastrointestinal manifestations in some cases, which could interfere with the diagnosis of AA or be a source of confusion in the diagnostic process.11,12 In all of our patients, the gastrointestinal manifestations could be explained by the AA diagnosis.
On the other hand, the data we collected show that the mean length of stay increased in patients operated after the lockdown was established, which adds to an already challenging situation in which material and human resources in health care are strained. An earlier diagnosis at a time when acute appendicitis has not progressed to further stages would reduce the hospital stay, thus contributing to increasing the availability of beds and health care staff devoted to fighting the pandemic. Another strategy already in use by some hospitals before the pandemic was conservative treatment of uncomplicated AA, with results that were not always favourable, as seen in the study published by Huang et al., who reported an increased length of stay and that a certain proportion of children ended up requiring an appendectomy due to poor outcome of medical treatment.13 Furthermore, appendicitis that do not fulfil the criteria of uncomplicated AA, such as gangrenous AA or peritonitis, require surgical management.14
Therefore, in light of the impact of the pandemic on the care delivery for patients with AA, paediatric surgeons, paediatricians, primary care physicians and family members must be aware of this problem and attempt to minimise delays in diagnosis once symptoms develop, so that patients seek care when they are in better condition and recover as soon as possible. Similarly and indirectly, this would contribute to an increased availability of material and human resources in hospitals.
Given the current circumstances, it is only to be expected that no other studies assess the impact of the pandemic on AA, which poses challenges in the extrapolation of our findings. However, we wanted to share our experience to convey to the wider paediatric care community of the risk of underestimating or undertreating a disease that is usually mild but that carries a high risk of complications in case diagnosis or treatment are delayed.
We must strongly raise awareness in the paediatric care community to ensure that the management of diseases that are highly prevalent in childhood, such as AA, does not suffer, or their outcomes worsen, due to the current severe epidemiological crisis, as children should not be left unprotected, regardless of their infectious or contagious status.
Limitations of the studyThe main limitations of this study are its retrospective design, which precluded random selection of patients, the small sample size and the short followup.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Velayos M, Muñoz-Serrano AJ, Estefanía-Fernández K, Sarmiento Caldas MC, Lapeña LM, López-Santamaría M, et al. Influencia de la pandemia por coronavirus 2 (SARS-Cov-2) en la apendicitis aguda. An Pediatr (Barc). 2020;93:118–122.