Risk factors (RFs) in paediatric stroke differ from those of adults, and they include a wide range of diseases such as heart disease, infections, leukemias, and inborn errors of metabolism.
ObjectivesTo describe RF for ischaemic stroke in a paediatric population, and to examine the relationship of RF with age, sex and type of stroke.
Patients and methodsAn analysis was performed on a database of 114 children and adolescents with ischaemic stroke from January 2003 to July 2012. Risk factors were stratified into 6 categories and ischaemic strokes were classified as arterial and venous. We compared the RF with age, sex, and type of stroke (chi2 and OR).
ResultsThe median age was 2.5 years, with 74 (62.2%) males. No RF was identified in 7.9% of patients, and 67% had more than one RF. The most common RFs were acute systemic diseases (56.1%), heart disease (35.1%), and chronic systemic diseases (29.8%). There was a statistically significant association between acute systemic disease and age less than 5 years (P<0.001), and between chronic systemic disease and age 5 years or more (P<0.02). The RF of heart disease was associated with arterial infarction (P<0.05), and the acute head and neck disease RF was associated with venous infarction (P<0.05).
ConclusionsThe RFs for ischaemic stroke are multiple in the paediatric population, and some of them are associated with a specific age and type of stroke. The detection of these factors may help in the primary prevention of people at risk, an early diagnosis, and treatment and prevention of recurrences.
Los factores de riesgo (FR) para accidente vascular encefálico (AVE) pediátrico difieren del adulto e incluyen un amplio rango de enfermedades, como pueden ser cardiopatías, infecciones, leucemias y errores congénitos del metabolismo.
ObjetivosDescribir FR en AVE isquémico en población pediátrica y explorar asociación de los FR con edad, sexo y tipo de AVE.
Pacientes y métodoSe analizaron 114 casos pediátricos con AVE isquémico ocurridos entre enero del 2003 y julio del 2012. Los FR se estratificaron en 6 categorías, los AVE isquémicos se clasificaron como arterial y venoso. Se compararon los FR con edad, sexo y tipo de infarto (chi al cuadrado y odds ratio).
ResultadosLa mediana de edad fue 2,5 años, 74 (62,2%) hombres. El 7,9% de los pacientes no tenía FR identificable y el 67% tenía más de uno. La mayor frecuencia de FR fue: enfermedades sistémicas agudas (56,1%), cardiopatías (35,1%) y enfermedades crónicas sistémicas (29,8%). Hubo asociación estadísticamente significativa entre FR enfermedad sistémica aguda y edad menor de 5 años (p<0,001) y entre enfermedad crónica sistémica y edad mayor o igual a 5 años (p<0,02). El FR cardiopatía se asoció a infarto arterial (p<0,05) y el FR enfermedad aguda de cabeza y cuello con infarto venoso (p<0,05).
ConclusionesLos FR de AVE isquémico en la población pediátrica son múltiples y algunos de ellos se asocian a edades específicas y tipo de AVE. La detección de estos factores permitirá la prevención primaria en la población de riesgo así como un diagnóstico y tratamiento precoz, haciendo igualmente posible la prevención de recurrencias.
The World Health Organisation (WHO) defines stroke as rapidly developing clinical signs of focal or global disturbance of cerebral function, lasting more than 24h or leading to death, with no apparent cause other than that of vascular origin.1
In the paediatric population, stroke is emerging as a severe and frequent disease. It has become one of the 10 leading causes of death worldwide, with a mortality nearing 10%, a rate of neurological sequelae of 70%, and a recurrence rate of up to 35%.2–4
Paediatric stroke is not something new. Since Willis and Osler published series of clinical cases in the XVII and XIX century, respectively, the number of reports on paediatric stroke has been rising exponentially.5–7 Previous studies have identified a wide range of associated factors, commonly termed risk factors (RFs), that are different from the RFs for stroke in adults.8–11 The RFs associated with adult stroke, such as hypertension, atheromatosis, tobacco use, and diabetes, are rarely found in children. The most common RFs associated to paediatric stroke are acute infections, congenital diseases such as cardiac disorders, some chronic systemic conditions and head and neck disorders.
Since children differ from adults in their RFs, the characteristics of their vascular and haematologic systems, and in their various stages of brain development, it is not possible to extrapolate the results of studies with adults or the treatment guidelines for adults to the paediatric population.12–14
Since 2003, the paediatric neurology department of the Pontificia Universidad Católica de Chile (PUC) started keeping a stroke registry for patients aged 0–18 years, and found an unusually high prevalence that had not been described in Chilean studies. This led to the creation of a paediatric stroke research programme, which associated with the International Paediatric Stroke Study (IPSS) Group15 in 2005. Access to the IPSS allows consulting and obtaining feedback in complex cases and participation in this multicentre study.
The aim of our study was to describe the RFs associated to ischaemic stroke in a paediatric population ranging from 1 month to 18 years of age, and to find the association of RFs to the different ages, types of stroke, and sexes.
Patients and methodsWe conducted a descriptive observational study of a cohort of 114 children with ischaemic stroke. Participants enrolled in the study during their hospitalisation or while being monitored in the outpatient services of the Hospital Clínico of the PUC from January 2003 to July 2012. The study was approved by our Ethics Committee.
Inclusion criteria were ischaemic stroke experienced between ages 1 month and 18 years diagnosed by brain neuroimaging (magnetic resonance imaging [MRI] or computer tomography [CT]). Exclusion criteria were haemorrhagic stroke, transient ischaemic attack, and incomplete records.
The data were collected in a clinical form designed for the purpose. The form gathered information on the clinical picture at onset, RFs, investigations performed, outcome at discharge, and subsequent follow-ups. The variables under study were demographic variables, risk factors, and subtype of ischaemic stroke.
DefinitionsStroke: acute neurological deficit lasting more than 24h with no apparent cause other than that of a vascular origin, confirmed by neuroimaging.16
Arterial ischaemic stroke: stroke, with brain CT or MRI showing parenchymal infarct(s) conforming to known arterial territory(ies) and corresponding to the clinical presentation.17
Cerebral sinovenous thrombosis: stroke or headache with venous thrombosis seen on neuroimaging study (CT or MRI).18
Arteriopathy: any stenosing abnormality of a cervical or intracranial artery, which is further characterised by the size of the affected vessels – small, medium, or large.19
RFs: we established 6 categories based on the IPSS definitions15: (1) acute systemic conditions, (2) acute head and neck disorders, (3) chronic systemic conditions, (4) chronic head and neck disorders, (5) cardiac disorders, and (6) arteriopathies. The RF categories were not mutually exclusive. We defined idiopathic stroke as stroke with no identified RFs.
Data analysis: we described the biodemographic characteristics of the sample at the time of the stroke, and stratified the sample by age (<5 years and ≥5 years) taking into account the major neurodevelopmental changes that occur before 5 years, as has been done in most multicentre studies.9 We analysed the RFs by age group, sex, and stroke subtype (chi2) and calculated the estimated risk as odds ratios (OR) with a 95% confidence interval. We performed the statistical analysis with the SPSS software, version 15.
ResultsOf the 114 patients, 74 (62.2%) were male. The median age was 2.5 years (interquartile range, 0.44–8.8 years), with 71 (62.3%) patients younger than 5 years. The stroke was of arterial origin in 100 children (84%), and affected the anterior circulation (anterior cerebral, middle cerebral, and internal carotid artery) in 67% of them. Cerebral sinovenous thrombosis occurred in 14 patients (12%), with predominance of superficial system thrombosis (superior sagittal and transverse sinuses and cortical veins) in 9 out of 14 cases (Table 1).
Affected territories in 114 cases of ischaemic stroke in children, 2003–2012. PUC, Chile.
| Territory | N° | % |
| Arterial ischaemic stroke | 100 | 100 |
| Anterior circulation | 67 | 67 |
| Right | 23 | |
| Left | 23 | |
| Bilateral | 24 | |
| Posterior circulation | 13 | 13 |
| Right | 3 | |
| Left | 6 | |
| Bilateral | 4 | |
| Both circulations | 20 | 20 |
| Cerebral sinovenous thrombosis | 14 | 100 |
| Superficial | 9 | 64 |
| Deep | 2 | |
| Both | 3 |
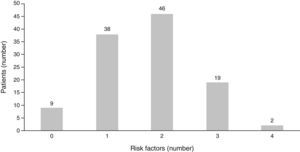
When it came to the number of RFs for stroke, no RF was identified in 9 children (7.9%) while 67 patients (58.7%) had more than one RF (Fig. 1).
The most common RFs were acute systemic conditions, cardiopathies, and chronic systemic conditions, found in 56.1, 35.1, and 29.8% of patients, respectively. The most common entities in the acute systemic condition category were sepsis, acute kidney failure, shock, and anoxia/hypoxia, with 16, 10, 9, and 5 cases of each, respectively. Acute systemic conditions showed a statistically significant association with the younger-than-5-years age group (P<0.001), with an OR of 4.1 (CI, 1.8–9.2). Congenital cardiopathies (82.5%) predominated in the cardiac disorder RF, and were more frequent in the younger-than-5-years age group (Table 2).
Frequency of risk factors and association of risk factors with age group in children with ischaemic stroke, 2003–2012. PUC, Chile.
| N (%) | Age group | P value | OR | CI (95%) | ||
| <5 years | ≥5 years | |||||
| Acute systemic condition | 64 (56.1) | 49 | 15 | 0.001 | 4.1 | 1.8–9.2 |
| Sepsis | 20 | 14 | 2 | |||
| Acute kidney failure | 8 | 8 | 2 | |||
| Hypoxia-cardiac arrest | 6 | 7 | 1 | |||
| Shock | 5 | 9 | 0 | |||
| Fever without sepsis | 6 | 3 | 2 | |||
| Acute heart failure | 5 | 2 | 2 | |||
| Other ASCs | 14 | 10 | 6 | |||
| Cardiopathy | 40 (35.1) | 25 | 15 | 0.9 | 1.01 | 0.24–2.2 |
| Congenital | 33 | 23 | 10 | |||
| Acquired | 7 | 2 | 5 | |||
| Chronic systemic condition | 34 (29.8) | 16 | 18 | 0.02 | 2.47 | 1.08–5.63 |
| Mesenchymal disorder | 4 | 1 | 3 | |||
| Genetic disorder | 6 | 4 | 2 | |||
| Neurocutaneous disorder | 3 | 3 | 0 | |||
| Thrombophilia | 5 | 3 | 2 | |||
| Epilepsy | 5 | 2 | 3 | |||
| Metabolic-neurodegenerative disorder | 5 | 2 | 3 | |||
| Kidney disease | 3 | 1 | 2 | |||
| Non-CNS tumour | 2 | 0 | 2 | |||
| Ulcerative colitis | 1 | 0 | 1 | |||
| Acute head and neck disorders | 29 (25.4) | 21 | 8 | 0.19 | 1.8 | 0.7–4.6 |
| Bacterial meningitis | 10 | 9 | 0 | |||
| Acute encephalitis | 2 | 2 | 0 | |||
| Upper respiratory tract infection | 7 | 3 | 4 | |||
| TBI | 3 | 1 | 2 | |||
| Decompensated brain tumour | 2 | 2 | 1 | |||
| Other | 5 | 4 | 1 | |||
| Arteriopathies | 16 (14) | 13 | 3 | 0.09 | 2.9 | 0.8–11.1 |
| Small vessel | 13 | 12 | 1 | |||
| Large vessel | 3 | 1 | 2 | |||
| Chronic head and neck conditions | 7 (6.1) | 3 | 4 | 0.27 | 1.4 | 0.09–2.0 |
| CNS malformation | 3 | 2 | 1 | |||
| Brain tumour | 2 | 1 | 1 | |||
| Other | 2 | 0 | 2 | |||
ASC: acute systemic condition; CI: confidence interval; CNS: central nervous system; OR: odds ratio; PUC: Pontificia Universidad Católica; TBI: traumatic brain injury.
Chronic systemic conditions were significantly associated to age 5 years and older, with an OR of 2.5 (Table 2). Arteriopathies accounted for 14% of all RFs and were more frequent in children younger than 5 years (the difference was not statistically significant).
Acute head and neck diseases tended to cluster in patients younger than 1 year, and consisted mainly of meningitis/encephalitis (12 cases) and upper respiratory tract infections (7 cases).
There were no significant differences for RFs between sexes.
As for the association between RFs and type of stroke, the cardiopathy RF was significantly associated to arterial ischaemic stroke (P<0.01) with an OR of 8.3 (CI, 1.05–66) and the acute head and neck condition was associated to cerebral sinovenous thrombosis (P<0.04, OR=3.5, CI 1.12–11.19) (Table 3).
Risk factor category by ischaemic stroke subtype in children, 2003–2012, PUC, Chile.
| Stroke subtype | P value | OR | CI (95%) | ||
| AIS | CSVT | ||||
| Cardiopathy | 39 | 1 | 0.01 | 8.31 | 1.05–66.08 |
| Arteriopathy | 13 | 3 | 0.41 | 0.55 | 0.13–2.23 |
| Acute systemic condition | 53 | 11 | 1.08 | 0.31 | 0.08–1.17 |
| Chronic systemic condition | 29 | 5 | 1.7 | 0.74 | 0.23–2.38 |
| Acute head and neck condition | 22 | 7 | 1.04 | 3.54 | 1.12–11. 19 |
| Chronic head and neck condition | 7 | 0 | 0.5 | – | |
AIS: arterial ischaemic stroke; CI: confidence interval; CSVT: cerebral sinovenous thrombosis; OR: odds ratio; PUC: Pontificia Universidad Católica.
Our results showed that paediatric stroke was more common in the early years of life (median: 2.5 years) and in males, as has been described in different international studies.20,21
The most common RF was acute systemic condition (56.1%), which was also associated to the younger-than-5-years age group (P<0.01, OR=4.1). The acute systemic condition RF included diseases that led to haemodynamic alterations with impairment of systemic and cerebral perfusion, something that had been described by Bladin and Chambers as early as 1994.22 The second most common RF was cardiac disorder (35.1%), which was associated to arterial ischaemic stroke, followed by chronic systemic condition (29.8%), which was significantly associated to stroke in the ≥5 age group.
The literature on paediatric stroke in South America is scarce, with the exception of the publications in Brazil.23–25 The study by Noce et al.23 of 39 children aged between 2 months and 15 years with ischaemic stroke reported that the largest number of cases with known aetiology corresponded to stroke secondary to dehydration (7 of these cases happened in patients <2 years of age). Dehydration can be considered an acute systemic condition, which is consistent with our results. In the Noce study, cardiac disorders were also the second most common aetiology, found in 7 of the 39 patients. Noce et al. remarked on the high percentage of cases (23.1%) in which a RF could not be identified.
We believe that cardiac disorders, the second most-common risk factor in our study, are underrepresented, as some cases of heart disease are probably left undiagnosed. Chile has a national plan for the treatment of congenital cardiopathies funded entirely by the government, but unfortunately this funding does not cover neuroimaging, neurophysiological, or genetic studies, which makes it hard to diagnose, treat, and make a prognosis of acute stroke. It is not unusual to find signs of a past stroke during the investigation of convulsions or delays of motor development in children with heart disease (this observation is based on the author's personal experience).
The literature in Europe26 describes the presence of cerebral artery abnormalities in up to 79% of the cases, while the multicentre studies of the IPSS Group show that arteriopathies are the most frequent RF in Asia, Europe, Canada, and Australia, but have a low prevalence in South America.11 Intracranial and cervical angiography studies were not done in every patient included in our study, and arteriopathies were detected in only 14% of the patients. We believe that these entities are underdiagnosed, and that the investigation of arteriopathies should be prioritised. Ideally, a conventional angiography or magnetic angioresonance study of intracranial and cervical vessels would be performed in all children with stroke, as this RF is the one most commonly associated with recurrences in the international literature.27
Our study included a significant sample of children with stroke, which allowed us to establish correlations and identify a population at higher risk for stroke, information that is important in prevention and early treatment. Given that acute systemic conditions accounted for the most frequent RF in our study, the risk of stroke should be taken into account in paediatric intensive care units, where routine assessment of cerebral function should be added to the monitoring of heart, kidney, and liver function. We also believe that hospitals should implement a specific protocol for neurological assessment in patients with cardiac disorders, and perform cerebral and cervical vessel studies in all stroke patients.
The detection of RFs for ischaemic stroke in children enables its early diagnosis and treatment, the optimisation of the management of acute stroke, and the long-term prevention of recurrence. The association between RFs and specific age groups allows targeted research of at-risk populations. The association between specific RFs and types of ischaemic stroke permits a better description of specific risks.
One of the limitations of our study is its selection bias, as we are a semi-private tertiary hospital and a leading reference in the surgical correction of congenital heart defects. It would be necessary to include public hospitals in order to obtain results that can be generalised to the population of Chile.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Hernández Chávez M, Samsó Zepeda C, López Espejo M, Escobar Henríquez R, Mesa Latorre T. Factores de riesgo para accidente vascular encefálico en un hospital universitario. An Pediatr (Barc). 2014;81:161–166.