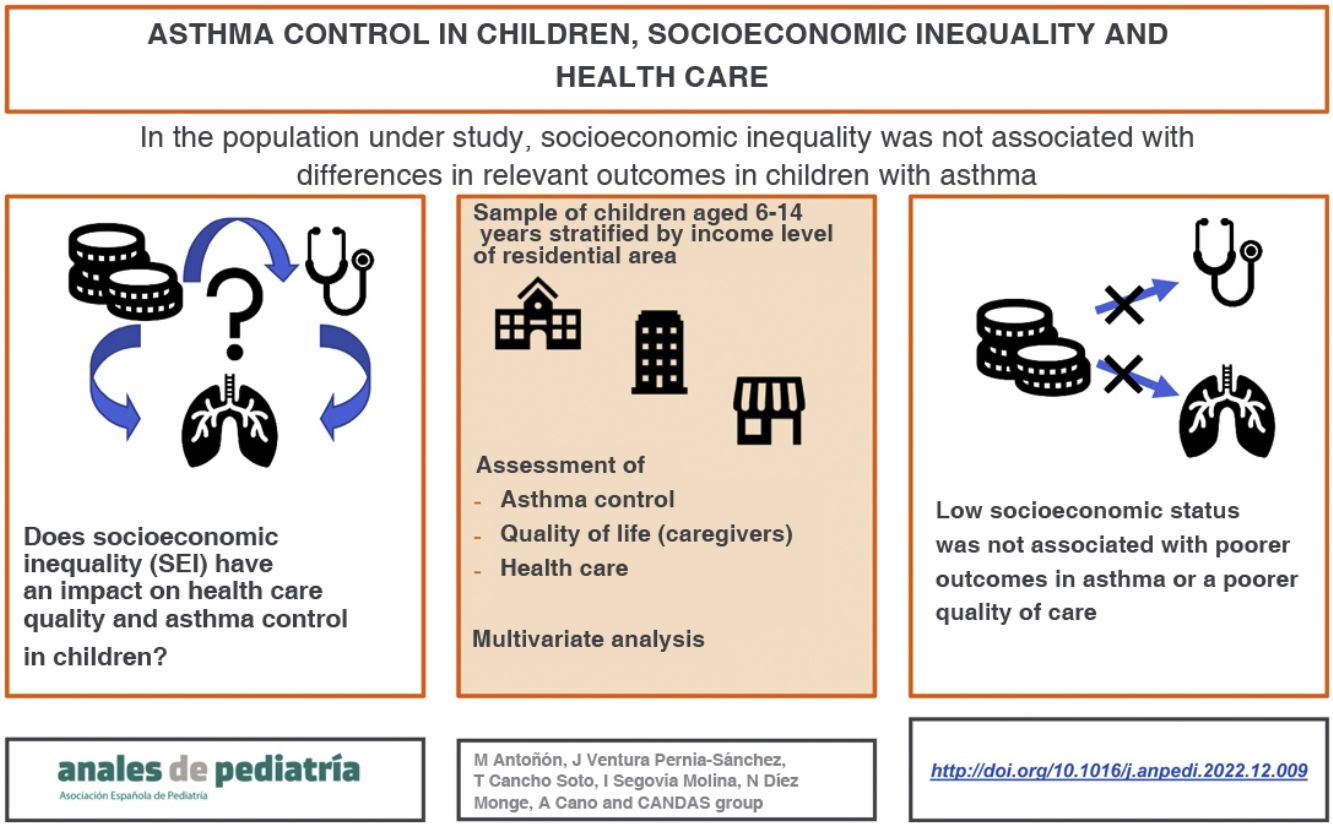
Socioeconomic inequality (SEI) can adversely affect asthma control. The aim of this study was to establish the association of SEI with asthma control in children and caregiver quality of life.
MethodsWe assessed socioeconomic status based on the area of residence, according to the at risk of poverty rate (ARPR). After stratifying the paediatric population of Castilla y León (Spain) in ARPR tertiles, we selected participants by stratified random sampling, and identified children with asthma aged 6–14 years from the health records of primary care centres. We collected data through questionnaires completed by parents. The primary outcomes were asthma control and caregiver quality of life. We assessed their association with SEI, health care quality measures and individual factors (such as parental educational attainment) by means of multivariate regression models.
ResultThe ARPR tertile was not associated with asthma control, quality of life or health care quality. A medium or high maternal educational attainment was associated with a lower risk of making an unscheduled or urgent visit (OR = .50; 95% CI, .27–.95; P = .034) and paternal educational attainment was associated with a lower risk of uncontrolled asthma (OR = 0.51; 95% CI, .28–.94; P = .030).
ConclusionIn the sample under study, SEI assessed at the local level was not associated with asthma control in children. Other factors, such as parental educational attainment, may have a protective effect.
La desigualdad socioeconómica (DSE) puede afectar negativamente al control del asma. El objetivo de este estudio fue identificar la relación de la DSE con el control del asma y la calidad de vida de los cuidadores.
MétodosEl nivel socioeconómico se determinó por área de residencia, según la tasa de riesgo de pobreza (TRP). La población pediátrica de la comunidad autónoma se estratificó en terciles de TRP, y se seleccionó una muestra mediante muestreo aleatorio estratificado, identificando a los niños (6–14 años) con asma activa en los registros clínicos de centros de atención primaria. La información se obtuvo mediante cuestionarios cumplimentados por los padres. Las variables primarias fueron el control del asma y la calidad de vida de los cuidadores. Se analizó su relación con la DSE, la calidad de la atención sanitaria y factores individuales (como el nivel educativo de los padres) mediante modelos multivariantes de regresión.
ResultadosEl tercil de TRP no se relacionó con ninguna medida de control del asma, calidad de vida ni calidad de la asistencia. El nivel educativo de la madre (educación media o superior) se asociaba a menor riesgo de consulta no programada/urgente (OR = 0,50, IC 95%: 0,27−0,95, p = 0,034) y el del padre a menor riesgo de asma mal controlada (OR = 0,51, IC 95%: 0,28−0,94, p = 0,030).
ConclusiónEn la población que hemos estudiado, no se encuentra asociación entre DSE, medida por área de residencia, y el control del asma en niños. Otros factores, como la educación de los padres, pueden ser factores protectores.
Asthma is the most frequent chronic disease in the paediatric population,1 with a prevalence of approximately 10% in school-age children in Spain, although with some variation between geographical areas (6%–8% in Castilla y León).2 The goals of asthma management are to achieve symptom control and reduce the risk of exacerbations so that patients can lead normal lives for their age.3 However, in developed countries, 30%–50% of school-age children and adolescents with asthma have poor asthma control.4,5
In a large proportion of cases, poor asthma control is due to factors modifiable through health care, such as poor inhaler technique6 or low adherence to treatment.7 Therefore, education on asthma self-management is crucial to achieve adequate control and an efficient use of health care resources,8,9 and clinical guidelines recommend it as one of the cornerstones of asthma management.3,10 In 2004, a specific programme for the management of children and adolescents with asthma was launched in the region of Castilla y León in Spain, including health care quality criteria, a written asthma action plan for the management of exacerbations, the evaluation of inhaler technique and assessment of lung function at regular intervals. However, there is variation in the actual capacity of the health care system to implement these practices, especially at the primary care (PC) level.11
Socioeconomic inequality (SEI) may preclude the achievement of favourable health care outcomes, and low socioeconomic status (SES) has been consistently identified as a risk factor for poor asthma control.12–14 Some studies have also found an association between low SES and a decreased quality of the care received by children with asthma,15–18 which in turn increases the risk of poor asthma control.19,20 In Spain, one of the mission statements of the National Health System is to guarantee health care equity and quality, thereby reducing the potential deleterious effects of SEI on health, including differences in asthma control among children with different SES.
The degree of asthma control at the population level can serve as a health care quality indicator, with a high prevalence of poorly controlled asthma indicating inadequacy or inappropriate use of the existing health care resources. In Spain, it has yet to be established whether SEI is associated with health care quality and asthma control in the paediatric population.
The aim of our study was to identify the association of SEI with asthma control measures, caregiver quality of life and health care quality in school-age children and adolescents in Castilla y León, an autonomous region in Spain with a population of 2.5 million people.
MethodsSampleWe conducted a cross-sectional study between March and April of 2022. The study universe comprised all school-age children and adolescents (age 6–14 years) with active asthma managed by the public health care system of the region of Castilla y León.
We selected patients by stratified random sampling. First, we established 3 strata defined by the 3 tertiles of the “at risk of poverty rate” (ARPR) distribution by census section in Castilla y León. The ARPR is the percentage of the population aged less than 18 years residing in households with incomes of less than 60% of the median equivalent income (income per consumption unit).21 We obtained the ARPR distribution of each census section from the Household Income Distribution Map developed by the national institute of statistics of Spain, the Instituto Nacional de Estadística (INE),22 which combines data from 2 sources23: (1) fiscal data from the Spanish tax administration agency (Agencia Estatal de Administración Tributaria) and (2) data from the INE on the population residing in the area as of January 1st the year after the period covered by the income tax data. In our study, we used the most recently published data (2018 fiscal year).
To identify patients with asthma in each stratum, we revised the health records of the primary care centres (PCCs) that provide health care services in each census section. We established the geographical boundaries of each census section through the Cartociudad24 application (Ministry of Transport, Mobility and Urban Planning of Spain) and determined how they corresponded to the catchment area of each PCC using the Health Care Organization Guide of the Department of Health of Castilla y León.25 We randomly selected PCCs within each stratum (ARPR) in proportion to the population of children aged 6–14 years of each province in the region (data from the INE as of July 2020). We excluded PCCs that included census sections with different ARPR levels. After, we invited the paediatricians who worked in the selected PCCs to participate in the study. If they did not respond or declined to participate, they were replaced by other paediatricians in the same province and ARPR stratum, who were also selected at random. The collaborating paediatricians identified all children managed in their respective PCCs who met the inclusion criteria, contacted their parents and invited them to participate in the study.
The inclusion criteria were: documentation in the electronic health record, as of 1/1/2022, of an asthma-related condition for which the patient had received health services in 2021 (at the PCC or hospital level) or prescription of any asthma medication (inhaled corticosteroids or leukotriene receptor antagonists) in order to include only cases of currently or recently active asthma. We excluded children whose families had language barriers precluding effective written communication.
VariablesAfter consenting to participation, the main caregivers of the patients completed questionnaires from which data for the variables of interest were retrieved, which concerned:
- 1
Sociodemographic characteristics. Age, sex, residential setting (urban/rural municipality, defined by the threshold of 20 000 inhabitants), number of members in the household, exposure to tobacco smoke (smoker in the household).
- 2
Asthma control. We assessed the components of impairment and risk. Impairment, defined by the current level of control (at the time of the survey in 2022), was assessed with the parent proxy version of the CAN questionnaire (Control del Asma en Niños, or asthma control in children).26 This instrument is used to assess asthma control in the past 4 weeks and comprises 9 items rated on a Likert scale ranging from 0 to 4 points (total possible score, 0–36 points), with higher scores indicating poorer asthma control. Poorly controlled asthma was defined as a CAN score of 8 or higher.26 We assessed risk through 3 variables in reference to year 2021: on-demand or urgent visits to PCC or hospital, having received at least 1 course of oral corticosteroids, hospital admission due to asthma.
- 3
Parent/caregiver asthma-related quality of life. This was assessed with the IFABI-R (revised version of the Impacto Familiar del Asma Bronquial Infantil, or Family Impact of Childhood Bronchial Asthma questionnaire), specifically designed to measure the impact on the quality of life of the primary caregivers of children with asthma in the past 3 months.27 It consists of 15 items rated on a Likert scale exploring the functional, emotional and socio-occupational dimensions of quality of life. The scores range from 1 to 4, and higher scores represent a greater impact of asthma and a poorer quality of life in caregivers. The minimum clinically important difference is of 0.3 points.27
- 4
Health care-related variables. Use (or not) of daily maintenance treatment, and number of drugs used, physician chiefly responsible for managing asthma in the child (only PC physician, involvement of allergologist), previous allergy testing (in vivo or in vitro), previous lung function testing with spirometry (ever and in 2021), verification by a health care professional of correct inhaler technique (ever and in 2021), having a written asthma action plan for management of exacerbations, having received guidance to avoid tobacco exposure, scheduled follow-up visit in 2021.
- 5
Other social and family-related aspects: parental educational attainment (having completed at least secondary education or a higher education degree) and whether the parents lived with the child.
We calculated the sample size necessary to estimate the prevalence of poorly controlled asthma, assuming a prevalence of asthma of 7% and a prevalence of poorly controlled asthma of 30%, with a precision of 5% and a confidence level of 95%, and found that we needed 313 patients evenly distributed through the 3 ARPR strata.
Statistical analysisThe main outcomes under study were asthma control (poor control in 2022 based on the CAN questionnaire and 3 risk indicators in reference to 2021: on demand/urgent visits, hospital admission, use of oral corticosteroids) and caregiver quality of life in 2022. We assessed their association with the ARPR stratum, other sociodemographic variables (urban/rural setting, parental educational attainment, exposure to tobacco smoke at home) and with health care-related variables (management exclusively at PC level) with bivariate tests (χ2 test, Mantel–Haenzsel statistic, Pearson correlation, Student t test and analysis of variance, as applicable) and multivariate regression methods (logistic regression and multiple regression). We adjusted the multivariate models for age, sex, ARPR stratum, urban/rural setting, exclusive PC management, presence of smoker in the household and paternal and maternal educational attainment. The models of asthma control in 2022 and of caregiver quality of life were also adjusted for the history of on demand/urgent visits in 2021. We defined statistical significance as a probability of α error of less than 0.05.
Ethical considerationsThe study was approved by the Clinical Research Ethics Committee of the Hospital Universitario Río Hortega. The parents of the participants received written information about the study and signed an informed consent form.
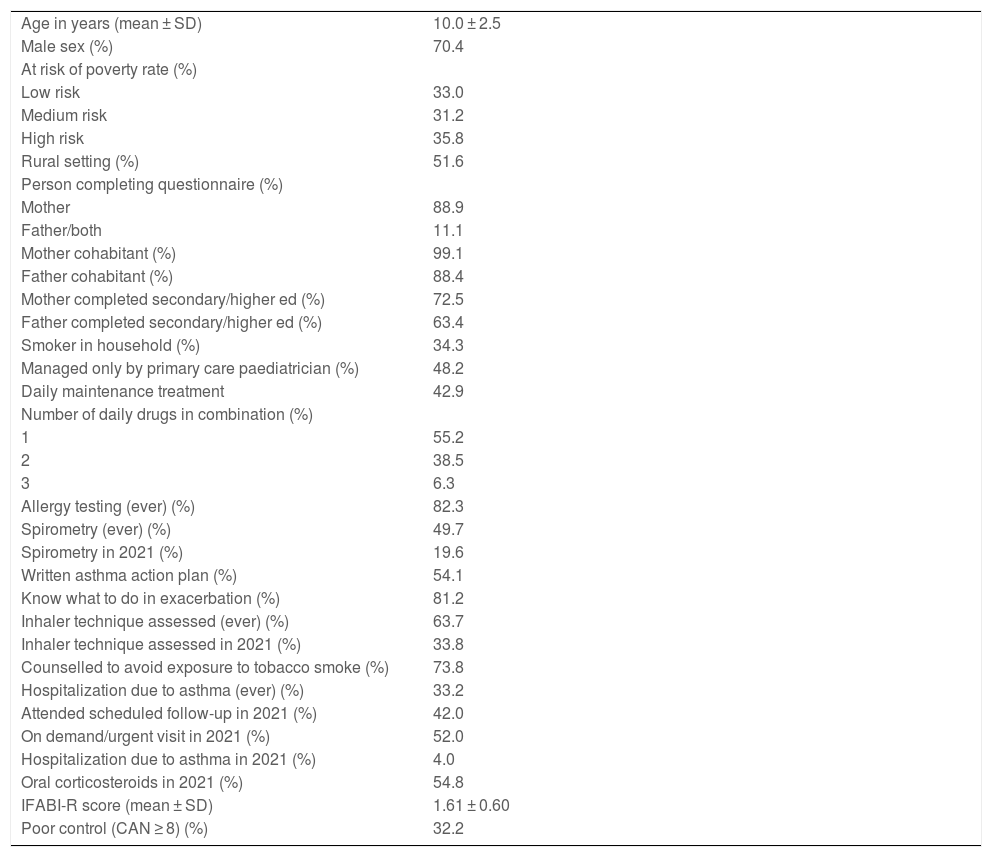
ResultsW contacted a total of 108 paediatricians, of who 40 (37.0%) agreed to collaborate. There were no significant differences in the percentage of paediatricians that agreed to collaborate between ARPR strata (41.0%, 28.6% and 41.2%; P = .971). We did not obtain data for one of the 9 provinces because no paediatrician in the province was included in the study. The collaborating paediatricians identified 586 patients who met the inclusion criteria, of who 80 (13.7%) could not be reached and 349 (59.6%) agreed to participate. We also found no significant differences in the participation of patients between ARPR strata (54.2%, 68.6% and 58.1%; P = .418). Table 1 summarises the demographic and clinical characteristics of the sample, which were evenly distributed between the ARPR strata. Of the total patients, 32.2% had poorly controlled asthma in 2022, and in 2021, 52.0% made on demand/urgent visits, 54.8% received oral corticosteroids and 4.0% were hospitalised.
Sample characteristics.
| Age in years (mean ± SD) | 10.0 ± 2.5 |
| Male sex (%) | 70.4 |
| At risk of poverty rate (%) | |
| Low risk | 33.0 |
| Medium risk | 31.2 |
| High risk | 35.8 |
| Rural setting (%) | 51.6 |
| Person completing questionnaire (%) | |
| Mother | 88.9 |
| Father/both | 11.1 |
| Mother cohabitant (%) | 99.1 |
| Father cohabitant (%) | 88.4 |
| Mother completed secondary/higher ed (%) | 72.5 |
| Father completed secondary/higher ed (%) | 63.4 |
| Smoker in household (%) | 34.3 |
| Managed only by primary care paediatrician (%) | 48.2 |
| Daily maintenance treatment | 42.9 |
| Number of daily drugs in combination (%) | |
| 1 | 55.2 |
| 2 | 38.5 |
| 3 | 6.3 |
| Allergy testing (ever) (%) | 82.3 |
| Spirometry (ever) (%) | 49.7 |
| Spirometry in 2021 (%) | 19.6 |
| Written asthma action plan (%) | 54.1 |
| Know what to do in exacerbation (%) | 81.2 |
| Inhaler technique assessed (ever) (%) | 63.7 |
| Inhaler technique assessed in 2021 (%) | 33.8 |
| Counselled to avoid exposure to tobacco smoke (%) | 73.8 |
| Hospitalization due to asthma (ever) (%) | 33.2 |
| Attended scheduled follow-up in 2021 (%) | 42.0 |
| On demand/urgent visit in 2021 (%) | 52.0 |
| Hospitalization due to asthma in 2021 (%) | 4.0 |
| Oral corticosteroids in 2021 (%) | 54.8 |
| IFABI-R score (mean ± SD) | 1.61 ± 0.60 |
| Poor control (CAN ≥ 8) (%) | 32.2 |
SD, standard deviation.
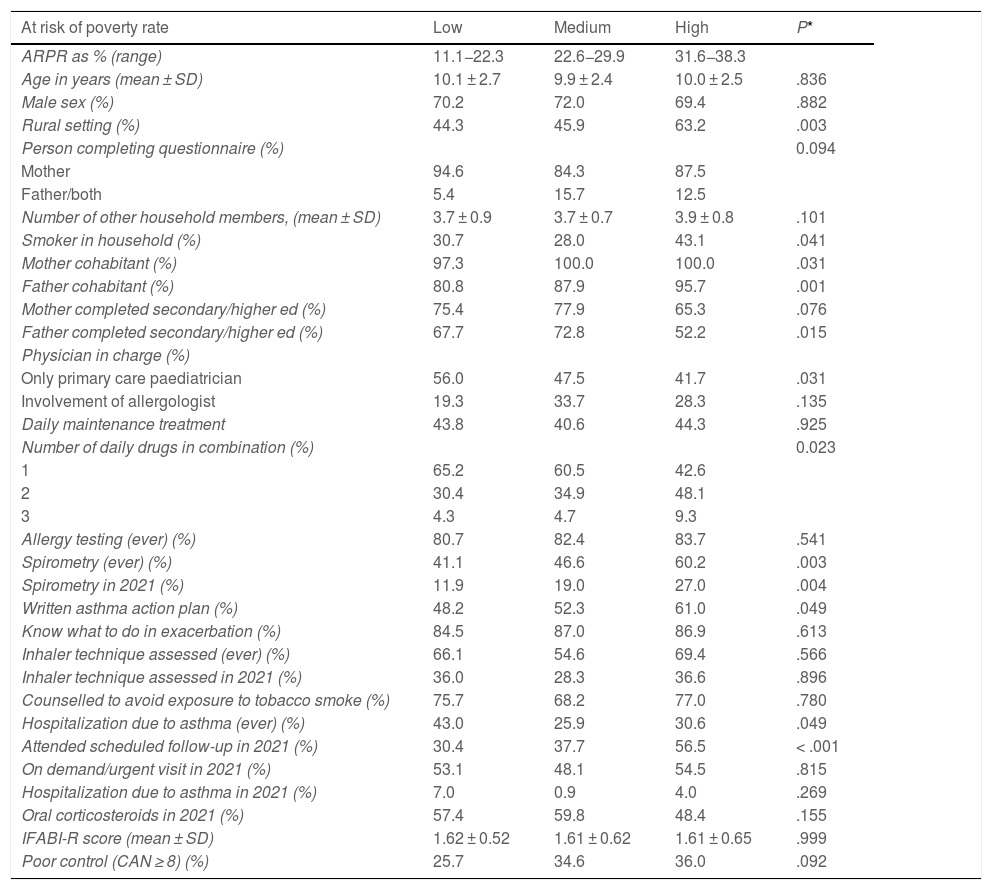
Low SES (the high ARPR category) was significantly associated with residing in a rural area, the father and mother living with the patient, a higher likelihood of exposure to tobacco smoke in the home, lower paternal educational attainment, a lower likelihood of management exclusively at the PC level, a greater likelihood of polypharmacy, greater frequency of spirometry (ever and in 2021), having a written asthma action plan and having had a scheduled follow-up visit in 2021(Table 2). WE found no differences in variables related to asthma control or quality of life.
Association between ARPR stratum and other sociodemographic and clinical variables.
| At risk of poverty rate | Low | Medium | High | P* |
|---|---|---|---|---|
| ARPR as % (range) | 11.1−22.3 | 22.6−29.9 | 31.6−38.3 | |
| Age in years (mean ± SD) | 10.1 ± 2.7 | 9.9 ± 2.4 | 10.0 ± 2.5 | .836 |
| Male sex (%) | 70.2 | 72.0 | 69.4 | .882 |
| Rural setting (%) | 44.3 | 45.9 | 63.2 | .003 |
| Person completing questionnaire (%) | 0.094 | |||
| Mother | 94.6 | 84.3 | 87.5 | |
| Father/both | 5.4 | 15.7 | 12.5 | |
| Number of other household members, (mean ± SD) | 3.7 ± 0.9 | 3.7 ± 0.7 | 3.9 ± 0.8 | .101 |
| Smoker in household (%) | 30.7 | 28.0 | 43.1 | .041 |
| Mother cohabitant (%) | 97.3 | 100.0 | 100.0 | .031 |
| Father cohabitant (%) | 80.8 | 87.9 | 95.7 | .001 |
| Mother completed secondary/higher ed (%) | 75.4 | 77.9 | 65.3 | .076 |
| Father completed secondary/higher ed (%) | 67.7 | 72.8 | 52.2 | .015 |
| Physician in charge (%) | ||||
| Only primary care paediatrician | 56.0 | 47.5 | 41.7 | .031 |
| Involvement of allergologist | 19.3 | 33.7 | 28.3 | .135 |
| Daily maintenance treatment | 43.8 | 40.6 | 44.3 | .925 |
| Number of daily drugs in combination (%) | 0.023 | |||
| 1 | 65.2 | 60.5 | 42.6 | |
| 2 | 30.4 | 34.9 | 48.1 | |
| 3 | 4.3 | 4.7 | 9.3 | |
| Allergy testing (ever) (%) | 80.7 | 82.4 | 83.7 | .541 |
| Spirometry (ever) (%) | 41.1 | 46.6 | 60.2 | .003 |
| Spirometry in 2021 (%) | 11.9 | 19.0 | 27.0 | .004 |
| Written asthma action plan (%) | 48.2 | 52.3 | 61.0 | .049 |
| Know what to do in exacerbation (%) | 84.5 | 87.0 | 86.9 | .613 |
| Inhaler technique assessed (ever) (%) | 66.1 | 54.6 | 69.4 | .566 |
| Inhaler technique assessed in 2021 (%) | 36.0 | 28.3 | 36.6 | .896 |
| Counselled to avoid exposure to tobacco smoke (%) | 75.7 | 68.2 | 77.0 | .780 |
| Hospitalization due to asthma (ever) (%) | 43.0 | 25.9 | 30.6 | .049 |
| Attended scheduled follow-up in 2021 (%) | 30.4 | 37.7 | 56.5 | < .001 |
| On demand/urgent visit in 2021 (%) | 53.1 | 48.1 | 54.5 | .815 |
| Hospitalization due to asthma in 2021 (%) | 7.0 | 0.9 | 4.0 | .269 |
| Oral corticosteroids in 2021 (%) | 57.4 | 59.8 | 48.4 | .155 |
| IFABI-R score (mean ± SD) | 1.62 ± 0.52 | 1.61 ± 0.62 | 1.61 ± 0.65 | .999 |
| Poor control (CAN ≥ 8) (%) | 25.7 | 34.6 | 36.0 | .092 |
ARPR, at risk of poverty rate; SD, standard deviation.
Exclusive management at the PC level was associated with a lower frequency of several care quality criteria: scheduled follow-up visit in 2021 (17.7% vs 67.6%; P < .001), having undergone spirometry for lung function testing at any point in the past (30.5% vs 69.5%; P < .001) and in 2021 (10.4% vs 29.5%; P < .001), having a written asthma action plan (41.0% vs 66.5%; P < .001), knowing what to do in the case of an exacerbation (78.1% vs 95.2%; P < .001) and assessment of inhaler technique in 2021 (28.4% vs 40.0%; P = .028).
Some social and family variables were significantly associated with some of the outcomes:
- -
In patients who lived with a smoker, the frequency of on demand/urgent visits in 2021 was higher (62.1% vs 47.1%; P = .009), as was the frequency of poorly controlled asthma in 2022 (39.3% vs 28.6%; P = .044).
- -
In patients whose mothers completed secondary/higher education, the frequency of on demand/urgent visits in 2021 was lower (46.7% vs 67.4%; P = .001).
- -
In patients whose fathers completed secondary/higher education, the frequency of poorly controlled asthma in 2022 was lower (26.2% vs 40.0%; P = .013).
- -
The quality of life assessed by means of the IFABI-R was somewhat poorer (higher score) in urban vs rural settings (mean, 1.68 [standard deviation [SD] 0.63] vs 1.55 [SD, 0.56]; P = .045) and improved with increasing patient age (r = −0.177; P = .001).
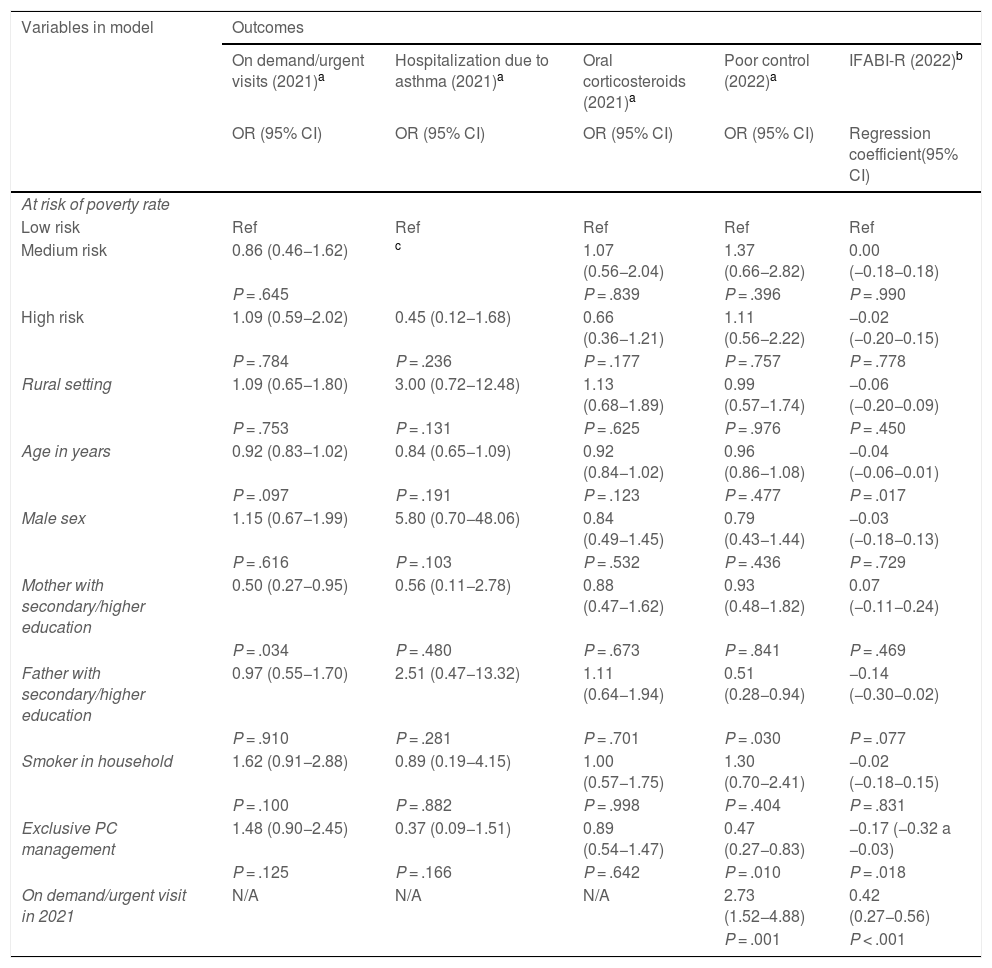
Table 3 presents the results of the multivariate analysis. The probability of on demand/urgent visits in 2021 was lower if the mother had completed secondary education or a higher education degree. The probability of poor asthma control in 2022 was lower if the patient was managed exclusively at the PC level and if the father had completed secondary education or a higher education degree, but poor asthma control was most strongly associated with the history of on demand/urgent visits in 2021. The quality of life of caregivers was better (lower score on the IFABI-R) when the patient was followed up exclusively at the PC level and with increasing patient age, but the only variable associated with a clinically important difference in quality of life (difference >0.3 points in the IFABI-R) was the history on demand/urgent visits in 2021. None of the multivariate models evinced an independent association of SEI with the outcome variables.
Multivariate analysis.
| Variables in model | Outcomes | ||||
|---|---|---|---|---|---|
| On demand/urgent visits (2021)a | Hospitalization due to asthma (2021)a | Oral corticosteroids (2021)a | Poor control (2022)a | IFABI-R (2022)b | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | Regression coefficient(95% CI) | |
| At risk of poverty rate | |||||
| Low risk | Ref | Ref | Ref | Ref | Ref |
| Medium risk | 0.86 (0.46−1.62) | c | 1.07 (0.56−2.04) | 1.37 (0.66−2.82) | 0.00 (−0.18−0.18) |
| P = .645 | P = .839 | P = .396 | P = .990 | ||
| High risk | 1.09 (0.59−2.02) | 0.45 (0.12−1.68) | 0.66 (0.36−1.21) | 1.11 (0.56−2.22) | −0.02 (−0.20−0.15) |
| P = .784 | P = .236 | P = .177 | P = .757 | P = .778 | |
| Rural setting | 1.09 (0.65−1.80) | 3.00 (0.72−12.48) | 1.13 (0.68−1.89) | 0.99 (0.57−1.74) | −0.06 (−0.20−0.09) |
| P = .753 | P = .131 | P = .625 | P = .976 | P = .450 | |
| Age in years | 0.92 (0.83−1.02) | 0.84 (0.65−1.09) | 0.92 (0.84−1.02) | 0.96 (0.86−1.08) | −0.04 (−0.06−0.01) |
| P = .097 | P = .191 | P = .123 | P = .477 | P = .017 | |
| Male sex | 1.15 (0.67−1.99) | 5.80 (0.70−48.06) | 0.84 (0.49−1.45) | 0.79 (0.43−1.44) | −0.03 (−0.18−0.13) |
| P = .616 | P = .103 | P = .532 | P = .436 | P = .729 | |
| Mother with secondary/higher education | 0.50 (0.27−0.95) | 0.56 (0.11−2.78) | 0.88 (0.47−1.62) | 0.93 (0.48−1.82) | 0.07 (−0.11−0.24) |
| P = .034 | P = .480 | P = .673 | P = .841 | P = .469 | |
| Father with secondary/higher education | 0.97 (0.55−1.70) | 2.51 (0.47−13.32) | 1.11 (0.64−1.94) | 0.51 (0.28−0.94) | −0.14 (−0.30−0.02) |
| P = .910 | P = .281 | P = .701 | P = .030 | P = .077 | |
| Smoker in household | 1.62 (0.91−2.88) | 0.89 (0.19−4.15) | 1.00 (0.57−1.75) | 1.30 (0.70−2.41) | −0.02 (−0.18−0.15) |
| P = .100 | P = .882 | P = .998 | P = .404 | P = .831 | |
| Exclusive PC management | 1.48 (0.90−2.45) | 0.37 (0.09−1.51) | 0.89 (0.54−1.47) | 0.47 (0.27−0.83) | −0.17 (−0.32 a −0.03) |
| P = .125 | P = .166 | P = .642 | P = .010 | P = .018 | |
| On demand/urgent visit in 2021 | N/A | N/A | N/A | 2.73 (1.52−4.88) | 0.42 (0.27−0.56) |
| P = .001 | P < .001 | ||||
CI, confidence interval; N/A, not applicable; OR, odds ratio; PC, primary care; Ref, reference group in the given variable.
In this study, we did not find evidence that lower SES is associated with differences in asthma control in children in our population nor with a poorer quality of life in caregivers or poorer quality of the care received. A higher parental educational attainment seems to be associated with better asthma control.
LimitationsThere are several limitations to this study that may have reduced the observed effect of SEI:
- 1
The identification of the income level based on the place of residence is considered an efficient method with a low risk of bias that generates results in the same direction as measures at the individual level.28,29 However, there is a risk of incorrect classification, which could have diluted the actual impact of SEI.
- 2
The fact that census sections and the catchment areas of PCCs do not match may have resulted in contamination bias. Although we excluded PCCs with catchment areas across census sections in different ARPR categories, we cannot rule out the possibility of contamination, which would also reduce the apparent effect of SES.
- 3
The census section income data correspond to 2018, but we collected data on asthma control variables in 2022. If there were changes in the income distribution, they would have hindered the detection of an association between income and asthma control.
- 4
The COVID pandemic affected both the health care services provided to children with asthma as well as asthma control at the global level,30 which may have also affected the association between SEI and asthma control.
- 5
Spain is very diverse in certain socioeconomic and health care aspects, so our results cannot be generalised without carrying out similar studies in other regions. Our region is sparsely urbanised, there are no large cities and no large economically depressed areas, which are the main targets of studies conducted in countries such as the United States. Thus, the impact of urban poverty, which may be substantial, is not adequately represented in our sample.
- 6
We used instruments (CAN, IFABI-R) validated in Spanish, so we excluded families with language barriers. As a result, our study is not representative of the immigrant population with language barriers, which may be particularly socioeconomically vulnerable.
The Beveridge health care system model (National Health Service model, such as the systems found in Spain, United Kingdom, Denmark, Portugal, Sweden and other European countries) aims at providing universal coverage for health care services in order to decrease the impact of SEI on health. It is important to confirm that this objective is achieved, but in Spain the evidence on socioeconomic health determinants is scarce, especially in relation child health.31 As for asthma, most of the evidence comes from countries with other types of health care systems (especially the United States) and studies in adults. A recent metanalysis (61 studies, most conducted in the USA, only 2 including paediatric participants), found that a lower SES was associated with adverse events during asthma follow-up (emergency visits, hospital admission, readmission, need of ventilation).32 However, there is also recent evidence in Europe of an adverse impact of SEI on asthma control in children and adolescents.33 Our findings were not in agreement with those results, which could be due to several reasons:
- 1
Some studies found an association between lower SES and less frequent use of asthma medication,13 which could contribute to poorer asthma control. In our study, however, we found a higher frequency of polypharmacy in patients who resided in low-income areas.
- 2
The impact of SEI on asthma-related outcomes is chiefly mediated by factors like social and family support, caregiver stress and self-management education, while factors such as access to the health care system, individual behaviour and lifestyle habits are less important.18,34 This may explain why standardised management has been found not to eliminate the effect of SEI in asthma control in the United States,14 while interventions aimed at reducing social risks do achieve this goal.35 Social and family-related variables and stress may differ significantly in our population compared to the populations of these other studies.
- 3
Particularities of the Spanish health care system, with a high number of paediatricians on staff in the PC network, which is not the case of other European countries.36 Furthermore, while other studies found that patients of lower SES were less frequently managed by specialists,37 the opposite was observed in our sample: exclusive follow-up in the PC system was less frequent with decreasing SES. We found that management exclusively at the PC level was associated with lower adherence to certain care quality standards, but at the same time was associated with better asthma control and caregiver quality of life, which we attributed to the lower severity of asthma cases managed exclusively at the PC level.
In conclusion, we found that in the population of our region, SEI was not associated with relevant outcomes of asthma in children, nor with differences in health care quality. We consider that this evinces the effectiveness of the National Health System in reducing the health care disparities that may result from SEI. Nevertheless, the quality of health care should improve, especially at the PC level.
FundingThe study was funded by a research grant of the Gerencia Regional de Salud de Castilla and León (GRS 2349/A/21).
Conflicts of interestThe authors have no conflicts of interest to declare.
Ana Belén Camina Gutiérrez (Centro de Salud [CS] Casa del Barco, Valladolid); Ana Rodríguez González (CS Lerma, Burgos); Ana Librán Peña (CS Circunvalación, Valladolid); David García Vaquero (CS Villarcayo, Burgos); Elena González García (CS Eras de Renueva, Leon); Francisco Fernández Pastor (CS Santa Elena, Zamora); Ignacio Ledesma Benítez (CS Trobajo del Camino, Leon); Isabel Redondo Díez (CS Peñafiel, Valladolid); José Francisco Colinas Herrero (CS Jardinillos, Palencia); José Francisco García de la Fuente (CS Ponferrada I, Leon); José Jorge Martín Martín (CS Alba de Tormes, Salamanca); José Luis Urquiza Físico (CS Huelgas, Burgos); Juncal Reguera Bernardino (CS Astorga I, Leon); Leyre López Villanueva (CS Miranda Este, Burgos); María Isabel Gómez Martin (CS Tudela de Duero, Valladolid); María Jesús Alonso Ballesteros (CS Medina del Campo, Valladolid); María Jesús Vaquerizo Pollino (CS Circular, Valladolid); María José Díez Huerga (CS Saldaña, Palencia); María José Martín Sierra (CS Tudela de Duero, Valladolid); María Montserrat Rodríguez Fernández (CS José Aguado I, Leon); María Romero Calvo Díaz (CS Miranda Este, Burgos); María Domínguez Villoria (CS Casto Prieto, Salamanca); María Polo de Dios (CS Zamora Sur, Zamora); María Rodríguez Rodríguez (CS Aguilar de Campoó, Palencia); María Teresa Sánchez Vélez (CS Béjar, Salamanca); Marta Esther Vázquez Fernández (CS Circunvalación, Valladolid); Marta Pascual Sánchez (CS Estación, Avila); Miriam Mata Jorge (CS Magdalena, Valladolid); Montserrat Piriz Veloso (CS Peñafiel, Valladolid); Nieves San José Calleja (CS Huelgas, Burgos); Olga García Bodega (CS Soria Rural, Soria); Patricia González Ildefonso (CS Estación, Avila); Pedro Florencio Martínez (CS Miranda Oeste, Burgos); Pilar Álvarez Mingorance (CS Medina del Campo, Valladolid); Pilar Gómez Sorrigueta (CS Eras de Renueva, León); Rafael Peñalver Penedo (CS Almazán, Soria); Raquel Rollón Casillas (CS Estación, Ávila); Sara Anibarro Pérez (CS Tordesillas, Valladolid); Soledad López Palacios (CS Alba de Tormes, Salamanca); Susana Alberola López (CS Jardinillos, Palencia) y Teresa Centeno Robles (CS Rondilla I, Valladolid).