Foetal abuse is that intentional or negligent act that causes a harmful effect to the foetus. It is a type of abuse difficult to diagnose and handle. Some indicators of suspicion are the absence of gestational control, the maternal consumption of toxic substances, or the problematic maternal social environment.
ObjectiveTo analyse the cases of foetal abuse registered in Catalonia between 2011 and 2014 to identify the risk profile.
MethodsA cross-sectional descriptive study was conducted on a sample of 222 cases of prenatal abuse registered in Catalonia between 2011 and 2014.
ResultsThe mean maternal age was 28.11 years, with 63% of Spanish nationality, 76% were unemployed, 60% had not followed correct gestational control, 76% had previous pregnancy interruptions, 20% reported to have been mistreated by the partner, had history of social problems (76% social intervention, 30.5% previous child retention, 13% custody of the mother by the administration, 7% deprivation of liberty), with high rates of mother-to-child transmission of infection (HIV 4.95%, HCV 9%, HIV+HCV co-infection 1.8%), and 73% reported toxic use (in order of frequency, cannabis, cocaine and heroin). In newborns, the rate of prematurity (26.3%) is highlighted, as well as the diagnosis of withdrawal syndrome in 34 cases. Just over half (51.6%) of the infants are currently with their mother.
ConclusionsIn our reference population with a diagnosis of prenatal abuse, there are high rates of maternal toxic consumption, HIV-HCV infection, unemployment, history of previous social intervention, and poor gestational control.
El maltrato prenatal es aquel acto intencionado o negligente que causa un efecto nocivo al feto. Es un tipo de maltrato difícil de diagnosticar y manejar. Algunos indicadores de sospecha son la ausencia de control gestacional, el consumo materno de tóxicos o la problemática social del entorno materno.
ObjetivoAnalizar los casos de maltrato prenatal registrados en Cataluña entre 2011 y 2014 para identificar el perfil de riesgo.
MétodosEstudio descriptivo de corte transversal de una muestra de 222 casos de maltrato prenatal registrados en Cataluña entre 2011 y 2014.
ResultadosLa edad media materna fue de 28,11 años. El 63% de los casos eran de nacionalidad española, un 76% estaba sin trabajo, el 60% no había seguido un correcto control gestacional, un 76% tenía interrupciones de embarazo previas, un 20% manifestaba haber sido maltratada por la pareja. Fueron frecuente los antecedentes de problemática social (76% intervención social; 30,5% retenciones de hijos previos; 13% tutela de la madre por la administración; 7% privación de libertad), con tasas elevadas de infección por enfermedades de transmisión vertical (VIH 4,95%, VHC 9%, coinfección VIH+VHC 1,8%), el 73% manifestó consumo de tóxicos (por orden de frecuencia cannabis, cocaína y heroína). En los neonatos, destacó el alto índice de prematuridad (26,3%) y el diagnóstico de síndrome de abstinencia en 34 casos. En el 51,6% el hijo está en la actualidad con su madre.
ConclusionesEn nuestra población de referencia con diagnóstico de maltrato prenatal destacan unos índices elevados de consumo materno de tóxicos, infección por VIH-VHC, desempleo, antecedentes de intervención social previa y mal control gestacional.
Prenatal abuse is defined as the mother failing to take adequate care of her body, whether knowingly or not, consuming illicit substances or psychotropic drugs, or being physically abused by another party.1,2 This concept is still not well known, although it has been regulated by Catalonian law since 2010 with the introduction of Law 14/2010 of May 27,3 which recognises the rights of the unborn child and places an unprecedented value on the foetus.
Some cases may be difficult to detect and risk indicators may be useful, such as the lack of prenatal care, the use of illegal substances, alcohol or psychotropic drugs without a prescription, unwanted pregnancy or indifference towards the pregnancy, a history of previous children in foster care, the presence of psychiatric disorders or untreated illnesses that may lead to congenital anomalies or infection in the foetus, physical abuse of the mother, maternal involvement in criminal activity or prostitution, or maternal neglect of her own body in terms of health, nutrition and hygiene. After birth, clinical manifestations of neonatal abstinence syndrome (NAS) should be considered a red flag suggestive of potential prenatal abuse.2,4
The consequences of prenatal abuse may be dire and alter the subsequent growth and development of the child. The potential deleterious effects on the foetus of drug exposure during gestation are well known, and include changes in neural proliferation, differentiation and migration, preterm birth, low birth weight, length and head circumference and NAS (with an increased incidence in newborns exposed to opiates). Potential postnatal consequences include psychomotor retardation and behavioural disorders. Furthermore, a history of prenatal abuse is a risk factor for future child abuse.5,6
Pregnancy provides an opportunity to detect situations where there is a higher risk of prenatal abuse due to the increased contact with health care providers (midwives, obstetricians, nurses). Social workers, psychiatrists and professionals employed in substance use treatment and recovery services should assess any situation indicative of risk in pregnant women. The early detection of risk factors makes it possible to inform the mother of the potential adverse effects on the foetus, redirect the situation, or activate the established protocol for the protection of the foetus or newborn.
The aim of the study was to analyse the cases of prenatal abuse documented in Catalonia between 2011 and 2014 to identify the risk profile for prenatal abuse in the population in our catchment area and determine its social impact.
Materials and methodsWe conducted a cross-sectional descriptive study of 222 cases of prenatal abuse reported to the Dirección General de Atención a la Infancia y Adolescencia (General Directorate of Child and Adolescent Services [DGAIA]) in Catalonia between 2011 and 2014. We extracted data for the variables of interest from the electronic records of each subject held in the Childhood and Adolescence database: medical reports with clinical and laboratory data, and social services reports based on interviews with parents and other kin, as well as the outcome of social intervention. We assigned a code to each case to safeguard the confidentiality of the individuals included in the study.
We structured the variables into three categories: maternal, perinatal and social intervention.
Maternal variables: age, nationality, occupation, number of previous children, prenatal care (considered appropriate if the mother made a minimum of 5 prenatal visits; poor in case of <5 visits; and absent if no visits were made),7 wanted or unwanted pregnancy, past history of voluntary termination of pregnancy, desire to terminate current pregnancy, support from partner, support from family, gender violence during pregnancy as reported by the mother), removal of previous children, previous involvement of social services, infectious diseases (the study considered HIV, HCV and syphilis), mental disorders (grouped according to the DSM-IV),8 substance use during gestation (reported by the mother), maternal history of foster care under DGAIA as a minor, and maternal history of deprivation of liberty (incarceration or placement in juvenile correctional facility before, during or after the pregnancy).
Perinatal variables: type of delivery (normal/complicated); gestational age at birth (extremely preterm, <32 weeks; moderately preterm, 320 to 366 weeks; full term, 370 to 420 weeks; post term, >420 weeks); birth weight, length and head circumference; Apgar score at 1 and 5minutes; perinatal complications during hospital stay.
Social intervention variables: professional that detected the case, measures taken at birth (placement with mother in nuclear family, placement in kinship care, emergency placement with a foster care family or foster care facility), whether the decision for the intervention was made before or after birth, and lastly, the current placement of the child (mother, kinship care, foster/adoptive family, emergency foster care family or children's home) and time when the current custody arrangement was established.
We performed the statistical analysis with the software SPSS for Windows (version 22). We have expressed categorical variables as absolute frequencies and percentages. We compared qualitative or categorical variables by means of the chi square test or Fisher's exact test as appropriate. We analysed quantitative variables with the Mann–Whitney U test when the normality assumption was not met. We defined statistical significance as a P-value of less than 0.05.
The study was approved by the research ethics committee of the hospital.
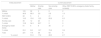
ResultsMaternal variables (Table 1)The mean maternal age was 28.11 years, with a range of 14–47 years, with 36 cases occurring in mothers aged less than 20 years. Most of the mothers were Spanish nationals, and only 40% had obtained appropriate prenatal care. Most mothers expressed that the pregnancy was unwanted at some point of gestation. In approximately half of the cases, the pregnant mother did not have the support of the biological father or a partner. Furthermore, 1 in 5 women reported having been physically abused by her partner. Up to 30.5% of mothers that had previous children had at least 1 child placed under the custody of the DGAIA, in the past or at the time of the study. Fourteen percent of mothers (30 cases) had an infectious disease that could be vertically transmitted: a total of 20 cases of HCV infection (9%) and 11 of HIV infection (4.95%), with HIV-HCV coinfection in 4 cases (1.8%), and 5 cases of syphilis (2.25%). In the 158 cases where the mothers had mental health disorders, the most frequent were substance use disorders (127 cases in total, with psychiatric comorbidities in 51), followed by personality disorders (41 cases), schizophrenia or psychotic disorder not otherwise specified (19 cases), anxiety and mood disorders (17 cases) and mental retardation (14 cases). Seventy-three percent of mothers reported using substances during the pregnancy, either sporadically or habitually. The most frequently used drugs were cannabis and cocaine, followed by heroin (Table 2). Thirteen percent of mothers had a history of being in the custody of the DGAIA as minors. Sixteen mothers had a history of deprivation of freedom, in 7 during pregnancy (6 in prison and 1 in a juvenile correction facility).
Results for maternal variables [n and (%)].
| Maternal age | ||
| ≤15 years | 5 | (2.25) |
| 16–20 years | 31 | (13.96) |
| 21–25 years | 48 | (21.62) |
| 26–30 years | 52 | (23.42) |
| 31–35 years | 51 | (22.97) |
| 36–40 years | 28 | (12.61) |
| >40 years | 7 | (3.15) |
| Nationality | ||
| Spanish | 139 | −0.63 |
| Other | 83 | −0.37 |
| Employment | ||
| Unemployed | 169 | −0.76 |
| Employed | 53 | −0.24 |
| Number of previous children | ||
| 0 | 91 | (40.99) |
| 1 | 62 | (27.93) |
| 2 | 31 | (13.96) |
| ≥3 | 38 | (17.12) |
| Prenatal care | ||
| None | 89 | (40.09) |
| Inadequate | 44 | (19.82) |
| Adequate | 89 | (40.09) |
| Wanted pregnancy | ||
| Yes | 56 | (25.23) |
| No | 166 | (74.77) |
| History of voluntary termination of pregnancy | ||
| Yes | 53 | (23.87) |
| No | 169 | (76.13) |
| Wish to terminate current pregnancy | ||
| Yes | 28 | (12.61) |
| No | 194 | (87.39) |
| Support from partner | ||
| Yes | 113 | (50.90) |
| No | 109 | (49.10) |
| Support from family | ||
| Yes | 131 | (59.01) |
| No | 91 | (40.99) |
| Gender violence during pregnancy | ||
| Yes | 45 | (20.27) |
| No | 177 | (79.73) |
| Removal of previous children | ||
| Yes | 40 | (30.5) |
| No | 91 | (69.5) |
| Previous social intervention | ||
| Yes | 169 | (76.13) |
| No | 53 | (23.87) |
| Infectious disease | ||
| HCV | 14 | (6.30) |
| HIV | 7 | (3.15) |
| HIV+HCV | 4 | (1.80) |
| Syphilis | 3 | (1.35) |
| Syphilis+HCV | 2 | (0.90) |
| Mental disorders | ||
| Yes | 158 | (71.17) |
| No | 64 | (28.83) |
| Substance use | ||
| Yes | 162 | −0.73 |
| No | 60 | −0.27 |
| History of mother in care of DGAIA | ||
| Yes | 29 | (13.06) |
| No | 193 | (86.94) |
| Deprivation of liberty | ||
| Yes 16 | −0.07 | −7 |
| No | 206 | −0.93 |
DGAIA, Dirección General de Atención a la Infancia y Adolescencia; HCV, hepatitis C virus; HIV, human immunodeficiency virus.
Substances used.
| Substance | Absolute frequency (%) among the 162 users | % of substance use in the 222 mothers |
|---|---|---|
| Cannabis | 90 (55.5) | 40.5 |
| Cocaine | 87 (53.7) | 39.1 |
| Heroin | 38 (23.4) | 17.1 |
| Alcohol | 34 (20.9) | 15.3 |
| Methadone | 30 (18.5) | 13.5 |
| Benzodiazepines | 19 (11.7) | 8.5 |
| Amphetamines | 15 (9.2) | 6.7 |
| Methamphetamine | 2 (1.2) | 0.9 |
| Most frequent combinations | ||
| 1 substance | 72 (44.4) | 32.4 |
| 2 substances | 49 (30.2) | 22 |
| 3 substances | 27 (16.6) | 12.1 |
| ≥ 4 substances | 14 (8.6) | 6.3 |
| Cannabis (only) | 45 (27.7) | 20.7 |
| Cannabis and cocaine | 19 (11.7) | 8.5 |
| Cocaine | 19 (11.7) | 8.5 |
| Cocaine and alcohol | 9 (5.5) | 4 |
| Cocaine, heroin and methadone | 8 (4.9) | 3.6 |
| Alcohol | 6 (3.7) | 2.7 |
| Heroine and methadone | 6 (3.7) | 2.7 |
| Cannabis and alcohol | 3 (1.8) | 1.3 |
| Cocaine, cannabis and alcohol | 3 (1.8) | 1.3 |
| Other | 44 (27.1) | 19.8 |
The most salient finding was that 26.3% of children were born preterm (22.1% moderately preterm and 4.2% extremely preterm). The mean birth weight was 2776.97g, while 28.5% of the newborns had birth weights of less than 2500g.
Results of perinatal variables, overall and by maternal substance use [n and (%)].
| No substance use | Substance use | Total | |
|---|---|---|---|
| Type of delivery | |||
| Data not available | 5 | 13 | 18 |
| Normal | 37 (67.3) | 95 (63.7) | 132 (64.7) |
| Complicated | 18 (32.7) | 54 (36.3) | 72 (35.2) |
| Caesarean | 12 (21.8) | 36 (24.1) | 48 (23.5) |
| Vacuum extraction | 3 (5.4) | 7 (4.7) | 10 (4.9) |
| Spatula-assisted | 2 (3.6) | 6 (4) | 8 (3.9) |
| Forceps | 1 (1.8) | 5 (3.3) | 6 (2.9) |
| Gestational age | |||
| Data not available | 9 | 23 | 32 |
| Post term | 0 | 0 | 0 |
| Full term | 40 (78.4) | 100 (71.9) | 140 (73.7) |
| Preterm | 11 (21.6) | 39 (28) | 50 (26.3) |
| Moderately | 6 (11.8) | 36 (25.9) | 42 (22.1) |
| Extremely | 5 (9.8) | 3 (2.2) | 8 (4.2) |
| Neonatal anthropometric measurements | |||
| Data not available | 6 | 23 | 29 |
| Mean weight (g) | 2995.74 | 2691.99 | 2776.98 |
| ≥2500g | 46 (85.2) | 92 (66.2) | 138 (71.5) |
| <2500g | 8 (14.8) | 47 (33.8) | 55 (28.5) |
| 1500–2500g | 6 (11.1) | 45 (32.4) | 51 (26.5) |
| <1500g | 2 (3.7) | 2 (1.4) | 4 (2) |
| Mean length (cm) | 47.66 | 46.38 | 46.74 |
| Mean head circumference (cm) | 33.41 | 32.54 | 32.78 |
| Apgar score | |||
| Data not available | 11 | 29 | 40 |
| 1 minute ≤8 | 9 (18.4) | 23 (17.3) | 32 (17.6) |
| >8 | 40 (81.6) | 110 (82.7) | 150 (82.4) |
| 5 minutes ≤8 | 3 (6.1) | 7 (5.3) | 10 (5.5) |
| >8 | 46 (93.9) | 126 (94.7) | 172 (94.5) |
The most common perinatal risk factor was the presence of toxic substances in urine in 133 cases, detected in the urine of both mother and child, and in 14 cases only in maternal urine). Also in relation to substance use, 34 newborns received a diagnosis of NAS.
Social intervention variables (Table 4)Nearly half of the cases were detected by neonatologists (45.4%). In 53.4% of cases, the child was not initially placed with the mother (placement in emergency foster family, kinship care or residential facility), and 48.4% were still not in the care of the mother at the time of the analysis.
Results for social intervention variables [n and (%)].
| Detection of case | |
| Neonatologist | 101 (45.4) |
| Obstetrician | 57 (25.6) |
| Removal of previous children | 22 (10) |
| Social rehabilitation services | 17 (7.6) |
| DGAIA due to long past history | 11 (4.9) |
| Psychiatrist/SUTRC | 6 (2.7) |
| Family/friends | 4 (1.8) |
| Prison | 2 (0.9) |
| Women's services | 1 (0.45) |
| Police (Mossos d’esquadra) | 1 (0.45) |
| Initial placement | |
| Not documented | 1 |
| Mother | 103 (46.6) |
| Emergency foster family | 51 (23.1) |
| Kinship care | 35 (15.8) |
| CHES/REF | 32 (14.5) |
| Decision on initial placement made before birth | |
| Yes | 70 (31.5) |
| No | 152 (68.5) |
| Current placement | |
| Not documented | 1 |
| Mother | 114 (51.6) |
| Foster/adoptive family | 63 (28.5) |
| Kinship care | 38 (17.2) |
| CHES/REF | 2 (0.9) |
| Emergency foster family | 2 (0.9) |
| Runaway | 2 (0.9) |
| Age at which placement changed | |
| Data not available | 3 |
| No changes | 122 (55.7) |
| Change | 97 (44.3) |
| Before 12 months | 50 (51.54) |
| Between 12 and 24 months | 34 (35.05) |
| More than 24 months | 13 (13.40) |
CHES, Children's home and emergency; DGAIA, Dirección General de Atención a la Infancia y Adolescencia; REF, residential educational facility; SUTRC, Substance Use Treatment and Recovery Centre.
The bivariate analysis of social intervention variables (Table 5) found that nationality, prenatal care, removal of previous children, whether the pregnancy was wanted, the presence of NAS, maternal substance use and the type of substance used, maternal schizophrenia and paternal/family support were significantly associated with the measures taken at birth. Out of the total cases in which DGAIA had removed a previous child (40), the decision was made before birth in 77.5% (P<.001).
Placement at birth (%) by different variables under study (bivariate analysis).
| Mother | Kinship care | Emergency foster family | Residential facility | |
|---|---|---|---|---|
| Maternal nationality (P=.007) | ||||
| Spanish | 52.5 | 18.7 | 21.6 | 7.2 |
| Other | 42.2 | 8.4 | 31.3 | 18.1 |
| Prenatal care (P<.001) | ||||
| Yes | 64 | 21.3 | 11.2 | 3.4 |
| No | 38.2 | 6.7 | 38.2 | 16.9 |
| Inadequate | 38.6 | 18.2 | 27.3 | 15.9 |
| Removal of previous children (P<.001) | ||||
| Yes | 9.5 | 19 | 61.9 | 9.5 |
| No | 57.8 | 13.9 | 16.7 | 11.7 |
| Placement decision made before birth (P<.001) | ||||
| Yes | 17.1 | 17.1 | 51.4 | 14.3 |
| No | 63.2 | 13.8 | 13.2 | 9.9 |
| Wanted pregnancy (P<.001) | ||||
| Yes | 76.8 | 17.9 | 3.6 | 1.8 |
| No | 39.2 | 13.9 | 32.5 | 14.5 |
| NAS at birth (P=.001) | ||||
| Yes | 20.6 | 32.4 | 38.2 | 8.8 |
| No | 53.7 | 11.7 | 22.9 | 11.7 |
| Maternal substance use | ||||
| Cannabis (P=.038) | 58.9 | 13.3 | 22.2 | 5.6 |
| Cocaine (P=.063) | 47.1 | 20.7 | 26.4 | 5.7 |
| Heroin (P<.001) | <12.8 | 28.2 | 46.2 | 12.8 |
| Alcohol (P=.042) | 35.3 | 14.7 | 44.1 | 5.9 |
| Psychotic disorder (P=.001) | ||||
| Yes | 10.5 | 10.5 | 57.9 | 21.1 |
| No | 52.2 | 15.3 | 22.2 | 10.3 |
| Support of father (P<.001) | ||||
| Yes | 65.5 | 14.2 | 8.8 | 11.5 |
| No | 31.2 | 15.6 | 42.2 | 11 |
| Support of family (P<.001) | ||||
| Yes | 66.2 | 24.6 | 4.6 | 4.6 |
| No | 23.1 | 1.1 | 54.9 | 20.9 |
| Maternal history of being in care of DGAIA (P=.419) | ||||
| Yes | 34.5 | 17.2 | 34.5 | 13.8 |
| No | 50.8 | 14.5 | 23.8 | 10.9 |
| Maternal history of deprivation of liberty (P=.1) | ||||
| Yes | 18.8 | 25 | 37.5 | 18.8 |
| No | 51 | 14.1 | 24.3 | 10.7 |
P values given for the Pearson chi square test.
NAS, neonatal abstinence syndrome.
A considerable percentage of the mothers that had been in the custody of the DGAIA as minors or who remained in its custody had a history of deprivation of freedom in prison or a correctional facility (24.1% vs 4.7%; P=.002), and this group was also more likely to use heroin compared to the group of mothers that had never been in care (31% vs 15.5%; P=.041).
When we compared children's placements based on maternal use of the most common substances (Table 5), we found that removal from the family home was most common in cases where the mother used heroin (59%; P<.001) or alcohol (50%; P=.042) and in newborns with NAS (47%; P=.001).
In the subset of mothers with mental health disorders, only 10% of children born to mothers with schizophrenia or a psychotic disorder not otherwise specified remained with the mother after birth, while 79% were placed with emergency foster families or in a residential home (Table 5; P=.001). We found that family support was lower in this group of mothers compared to the rest (38.9% vs 63.2%), and that as many as 94.7% had been subject to some type of social intervention in the past (vs 74.4% of other mothers).
When we compared current placement with the initial placement (Table 6), we found that 89.3% of the children (P<.001) that had been placed with the mother at birth remained with the mother. Of those who were initially placed in a children's home, most were placed in non-kinship families at the time of the study (foster or adoptive family). All children that were initially placed in kinship care were still placed with extended family or had reunified with the mother. Lastly, of those placed in emergency foster families during investigation, only 9.8% (P<.001) were in the care of the mother at the time of the study, while most of the rest remained in non-kinship foster families. In total, 51.6% of children (114) are currently with their mothers.
Comparison of initial placement and current placement [n and (%)].
| Initial placement | Current placement | ||||
|---|---|---|---|---|---|
| Mother | Kinship care | Non-kinship care | Other (REF/CHES, emergency foster family, runaway) | ||
| Mother | 103 | 92 | 3 | 6 | 2 |
| % initial | 46.6 | 89.3 | 2.9 | 5.8 | 1.9 |
| REF/CHES | 32 | 5 | 4 | 21 | 2 |
| % initial | 14.5 | 15.6 | 12.5 | 65.6 | 6.3 |
| Kinship care | 35 | 12 | 23 | 0 | 0 |
| % initial | 15.8 | 34.3 | 65.7 | 0 | 0 |
| Emergency foster family | 51 | 6 | 8 | 36 | 2 |
| % initial | 23.1 | 9.8 | 15.7 | 70.6 | 3.9 |
| Total | 221 | 114 | 38 | 63 | 6 |
| % current | 51.6 | 17.2 | 28.5 | 2.7 | |
P=.000 in Fisher exact test.
CHES, Children's home and emergency; REF, residential educational facility; non-kinship care: foster or adoptive family.
The analysis of the association of substance exposure with neonatal anthropometric measures (Table 7) showed that the children of mothers who used substances had a lower birth weight, length and head circumference compared to the children of mothers that did not use, while there was no significant difference in the mean gestational age between these two groups. When it came to gestational age (Table 8), preterm birth was more frequent in mothers that used substances (28% vs 21.6%), a difference that mainly involved the number of children born moderately preterm, while mothers who did not use substances gave birth to more extremely preterm and full term newborns. All of these findings were statistically significant (P=.012).
Anthropometric values of newborns whose mothers used substances versus newborns whose mothers did not.
| Mean gestational age in weeks | Mean weight in g | Mean length in cm | Mean head circumference in cm | |
|---|---|---|---|---|
| No substance use | 37.87 (n 50) | 2995.74 (n 54) | 47.66 (n 48) | 33.41 (n 47) |
| Substance use | 37.67 (n 139) | 2691.99 (n 139) | 46.38 (n 124) | 32.54 (n 123) |
| Pa | 0.177 | 0.001 | 0.018 | 0.001 |
Gestational age by maternal substance use [n (%)].
| No substance use | Substance use | Total | |
|---|---|---|---|
| Extremely preterm (<32 wk) | 5 (9.8) | 3 (2.1) | 8 (4.2) |
| Moderately preterm (320–366 wk) | 6 (11.8) | 36 (25.9) | 42 (22.1) |
| Total preterm (<370 wk) | 11 (21.6) | 39 (28) | 50 (26.3) |
| Full term (370–420 wk) | 40 (78.4) | 100 (71.9) | 140 (73.7) |
| Total | 51 | 139 | 190 |
P=.012 (Pearson chi square test).
The results of our study were consistent with the risk factors for prenatal abuse described in the literature.1,2
The mean age of the mothers (28.11 years) was low compared to the mean age of mothers in Catalonia in 2014 (31.7 years),9 with a considerable difference in the proportion aged less than 20 years (16.2% in our study compared to 2.45% in Catalonia in 2014).9 Young maternal age is a risk factor for foetal abuse, which may be due to a lack of awareness about health, greater substance use, unwanted/unplanned pregnancy or lower economic resources.10,11
The employment rate in Catalonia in women aged 16–64 years between 2011 and 2014 ranged from 54.7% to 59.7%,9 while only 24% of the women in our study were employed.
Although there is no consensus in the literature as to what constitutes appropriate prenatal care, for the purpose of this study we used the pregnancy care protocol of the Government of Catalonia as reference.7 A study conducted in Barcelona in 2013 found that 98.6% of pregnant women had at least 6 obstetrics appointments.12 The absence of care is in itself an indicator of risk and a reason to report prenatal abuse. In our study, this factor was strongly associated with the decision made at birth: babies were twice as likely to stay with the mother if the prenatal care had been adequate.
Gender violence against the pregnant mothers was 10 times as frequent as the violence experienced in the past 12 months reported by women residing in Spain in a large-scale survey conducted between September and November 201413 (20% vs 1.9%), and is considered prenatal abuse and neglect in and of itself based on Law 14/2010 of May 27.3
In Spain, the prevalence in of HIV infection in mothers of live newborns is estimated at 1.41‰ based on a study conducted in 2008,14 while the prevalence in our group was as high as 49.55‰. There was also a significantly higher prevalence of HCV infection (9%) compared to pregnant women in the general population (of around 1% based on the reviewed sources).15,16 The rate of HIV-HCV coinfection in our study was 36.36%, compared to an estimated 20–25% in the general population.17,18 This could be related to the high prevalence of substance use in our study.
The prevalence of substance use in pregnant women is typically much lower than that in the general population. Although the published data are scarce, a study conducted in the United States found that 5.4% of pregnant women used illicit drugs, compared to 11.4% of women in the same age group who were not pregnant.19 The proportion in our group was much higher. In Spain, the EDADES study of 2013 found that in the general population, the prevalence of cannabis, cocaine and heroin use was 9.2%, 2.2% and 0.1%, respectively, figures that were considerably lower than those found in our study.11
The effects of these drugs on the foetus, in terms of preterm birth and alterations in foetal growth and development, are well known and were observed in our study. The percentage of preterm birth was considerably higher than the percentage reported for Catalonia in 2014 (6.3%).9 This difference was greater in the subset of mothers that used substances and manifested as an increase in the rate of moderately preterm birth. Also consistent with the above, the percentage of low birth weight of less than 2500g was also greater compared to infants born in the same year (7.4%)9: the children of substance-using mothers had a lower birth weight, length and head circumference than the children of non-using mothers.
Heroin was the drug associated with the greatest number of foster care placements, probably due to the problems associated with heroin addiction: social and family problems, marginalisation, and lack of economic resources, among others.
The age of the minor at the time the last placement decision is made has a significant impact on former: greater age is directly correlated to social and neurobehavioural problems and hinders bonding with the family.20 In our series, nearly in half the cases where there were changes in the placement of the minor, these occurred after age 12 months.
Since a high percentage of mothers did not seek any form of prenatal care, it was neonatologists that detected most of the cases. Thus, we need to emphasise the importance of the efforts of other professionals that interact with pregnant women in detecting prenatal abuse, especially in the field of social services, as a high percentage of the pregnant women in our study had a history of social intervention.
While current law recognises the rights of the foetus and calls for the detection of prenatal abuse, in cases involving maternal substance abuse its detection may be hindered by the need to obtain consent to collect biological samples for testing, a method that is considerably more reliable than the use of questionnaires.21,22 The current protocol for prenatal care does not include performance of laboratory tests aimed at detecting maternal substance use, and only stipulates that clinicians should ask about it, so a high level of suspicion is required for its detection.
One of the limitations of this study is that we extracted the data from the reports included in the DGAIA database, some of which were based on interviews with mothers and other relatives (social services reports). Thus, the responses may be biased due to subjective perception or concealment of information on the part of interviewees. Another limitation is the large number of interrelated variables, which hinders their analysis and interpretation, as each case is highly complex; this requires an individualised and multidisciplinary approach.
In conclusion, based on the results of this study, the profile of mothers that engage in prenatal abuse in our catchment area is that of a woman aged approximately 28 years, of Spanish nationality, unemployed, who does not adhere to adequate prenatal care, does not want the pregnancy, in many cases reports being abused by her partner, with a high incidence of HIV/HCV, uses substances (cannabis, cocaine, heroin) and a personal history of social intervention. There was a significantly high proportion of history of deprivation of liberty (prison or juvenile detention centre) and substance use (heroin) among mothers who had themselves been in the custody of the DGAIA.
We ought to highlight that prenatal abuse has a considerable impact on Spanish society and that there is still little awareness of it. Its detection is essential, and its prevention even more so, as once abuse occurs, the foetus may suffer consequences in the short as well as the long term. Adequate knowledge of risk indicators alerting of potential harmful situations is essential for the purpose of activating the established inter-institutional networks and implement the intervention that is most suitable to each case.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Garcia Garcia J, Campistol Mas C, López-Vilchez MÁ, Morcillo Buscato MJ, Mur Sierra A. Análisis del maltrato prenatal en Cataluña entre los años 2011 y 2014. An Pediatr (Barc). 2018;88:150–159.