Lung ultrasound is a useful tool for diagnosis and follow-up of diseases in critically ill neonates. Its use is increasingly widespread thanks to its advantages over other imaging tests and the rapidly growing body of evidence to support it, and “point-of-care ultrasound” (POCUS) has become a key component in neonatal guidelines. The objective of this special article is to present the foundations and the established diagnostic and therapeutic applications of lung ultrasonography as well as introducing new applications.
Methods and resultsThe Lung Ultrasound Section of the Neonatal Ultrasonography Working Group of the Spanish Neonatology Society has summarised the current scientific evidence. The article describes the sonographic features of the most common respiratory diseases, discusses some of the applications of ultrasound in neonatal care (such as prediction of admission and need of surfactant, ultrasound-guided procedures or monitoring of lung development in premature infants) and proposes its introduction in other scenarios in which its use is not quite established at present, such as resuscitation or respiratory management. This article reaffirms the usefulness of lung ultrasound in guiding diagnosis, clinical decision-making and prognosis and facilitating procedures.
ConclusionsLung ultrasound should be established as the gold standard for diagnosis of respiratory diseases in neonates. Therefore, training in lung ultrasound should be included in the educational curriculum of neonatologists and in diagnostic and therapeutic care protocols. Research on the subject should continue to be pursued with performance of rigorous multicentre studies to increase the quality of the evidence.
La ecografía pulmonar es una herramienta útil para el diagnóstico y seguimiento de la patología del paciente crítico neonatal. Su uso está cada vez más extendido gracias a sus ventajas sobre otras pruebas de imagen y el rápido incremento en la evidencia científica a su favor, constituyendo así, un pilar básico de las guías «point of care ultrasound» (POCUS) neonatal. El objetivo de este artículo especial es proporcionar las bases y aplicaciones diagnóstico-terapéuticas establecidas de la ecografía pulmonar, y dar a conocer nuevas aplicaciones.
Métodos y resultadosLa sección de ecografía pulmonar del Grupo de Trabajo de Ecografía Neonatal de la Sociedad Española de Neonatología resume la evidencia científica actual. Se describen los patrones ecográficos de las principales patologías respiratorias, aborda algunas de sus aplicaciones en la asistencia neonatal (predicción de ingreso, necesidad de surfactante, procedimientos ecoguiados, seguimiento del desarrollo pulmonar en el prematuro, entre otros) y propone su incorporación en otros escenarios actualmente menos establecidos como la reanimación o el manejo ventilatorio. Este artículo reafirma los beneficios de esta herramienta para ayudar en el diagnóstico, toma de decisiones terapéuticas, apoyo en procedimientos y valoración pronóstica.
ConclusionesLa ecografía pulmonar debe establecerse como la prueba diagnóstica de elección en la patología respiratoria neonatal. Por ello, su entrenamiento debería formar parte de la formación de los neonatólogos e incluirse en los protocolos diagnóstico-terapéuticos asistenciales. Se deben seguir desarrollando líneas de investigación con estudios sólidos y multicéntricos que aumenten la calidad de la evidencia científica.
Lung ultrasound (LUS) performed and interpreted by clinicians is a tool that has demonstrated advantages compared to other imaging techniques (chest radiograph). It offers a higher sensitivity (Sen) and specificity (Spe), greater interrater agreement and absence of exposure to ionising radiation.1 It is easy to learn how to use it with adequate training, quick and reproducible. For these reasons, its use has spread widely in recent years, attracting considerable interest in the field of neonatology and becoming one of the most important applications of neonatal point-of-care ultrasound (POCUS).
Still, the use of LUS in neonatal care is limited due to the lack of standardised protocols and diagnostic criteria.2 In 2020, the Working Group on Neonatal Ultrasound was created within the Sociedad Española de Neonatología (Spanish Society of Neonatology, SENeo) to promote and spread the use of neonatal ultrasound and collaborate in educational efforts and facilitate research on the technique. The Working Group has developed this document to summarise the current scientific evidence on LUS and its emerging applications. On one hand, it describes the sonographic features of the main neonatal respiratory diseases,3 and on the other, it addresses its main applications in different health care scenarios for the purpose of prognosis and clinical decision-making, thereby evincing that LUS is the gold standard for respiratory assessment in newborn infants.
Guidelines for performance of lung ultrasound3,4- 1
Technical aspects: choose a preset in the ultrasound system and set the scanning depth based on the selected transducer (4−5 cm) to ensure a proportionate image, and do not modify it to make images uniform. We recommend a high-definition linear transducer (12−14 MHz). If not available, it is possible to use a high-frequency convex array probe (≥8 MHz).
- 2
We recommend the use of nonpharmacological infant comfort measures (such as swaddling, administering breastmilk or sucrose or preheating the ultrasound gel). The ultrasound system and transducer must be cleaned and disinfected appropriately.
- 3
Exploration protocol: scan every region, adapting the examination to the personal circumstances of the patient (stickers, sensors, position, etc). (Fig. S1)
- 3.1
Placement of transducer: slide the transducer along the wide axis and occasionally along the short axis. Keep the transducer perpendicular to the ribs and avoid slanting or turning movements that can generate inaccurate images.
- 3.2
Areas for exploration:
- a
Anterior mid-transverse plane: between the nipples.
- b
Anterior-parasternal plane: between the mid-clavicular line (MCL) and anterior axillary line (AAL).
- c
Lateral plane: between the AAL and the posterior axillary line (PAL).
- d
Posterior plane: between the PAL and the mid-scapular line, it can be scanned with the patient in the lateral decubitus or prone positions.
- a
- 3.1
The images do not look like any recognisable structures, but result from the reflection of the beam and reverberation of echoes on tissue interfaces, creating what is known as artefacts. The most important are:
- 1
Pleural line: straight hyperechoic line formed by the difference in acoustic impedance between subcutaneous cell tissue/muscle (filled with liquid) and the lung (filled with gas).
- 1.1
Lung sliding: movement of the pleural line synchronized with respiratory movement produced by the change in the relative positions of the chest wall (parietal pleura) and the lung surface (visceral pleura). Video S1.
- 1.1
- 2
A-lines: horizontal hyperechoic lines that are a reflection of the pleural line and parallel to it that repeat at intervals equal to the skin-pleural line distance. They appear in variable numbers and, in some cases, there may be A’-lines between 2 A-lines. Their presence is indicative of lung aeration.
- 3
B-lines: vertical hyperechoic artefacts that arise from the pleural line in varying numbers throughout the entire screen. B-lines move with respiration and erase A-lines. They indicate the presence of liquid in the interstitial space and/or alveoli.
Table S1 describes the main artefacts and signs in lung ultrasound, both in the healthy lung and in specific diseases. Fig. S2.
Lung ultrasound patterns.1 (Table 1)Normal patternThe normal pattern, characteristic of a well-aerated lung, is characterised by a clearly defined pleural line, lung sliding, A-lines and discrete, non-confluent B-lines3 (Fig. S3, Video S2).
Lung ultrasound patterns.
| Lung pattern | Ultrasound signs | Figure | Video (link) |
|---|---|---|---|
| Normal pattern | Defined pleural line | Video S2 | |
| Lung sliding | |||
| Presence of A-lines | |||
| Discrete B-lines | |||
| Seashore sign (M-mode) | |||
| Interstitial pattern | Discrete B-lines | Video S3 | |
| Defined pleural line | |||
| Alveolar-interstitial pattern | Confluent B-lines | Video S4 | |
| Irregular or thickened pleural line | |||
| Pneumothorax | Absence of lung sliding | Video S5 | |
| Absence of B lines | |||
| Exclusive presence of A-lines | |||
| Lung point | |||
| Stratosphere sign (M-mode) | |||
| Consolidation pattern | Absence of pleural line | Video S6 | |
| Alveolar collapse with bronchogram | |||
| Hepatization | |||
| Shred sign | |||
| Pleural effusion | Anechoic area between parietal and visceral pleura | Video S7 | |
| Jellyfish sign (2D-mode) (A) | |||
| Sinusoid sign (M-mode) (B) | |||
| Quad sign (2D-mode) (C) |
They appear when the air-to-fluid ratio in the lung decreases and are characterised by the presence of B-lines. If the B-lines are clearly defined and discrete (non-confluent) with a defined pleural line, they are indicative of interstitial syndrome (Fig. S4, Video S3) and interstitial oedema, and if they are confluent, they are indicative of alveolar-interstitial (AI) syndrome and an even lower air-to-liquid ratio either due to alveolar oedema or decreased lung aeration, and the pleural line is usually irregular, thickened or poorly defined. The presence of a homogeneous AI pattern (compact B-lines through the entire lung field) is known as ‘white lung’ (Fig. S5, Video S4).
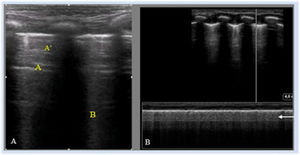
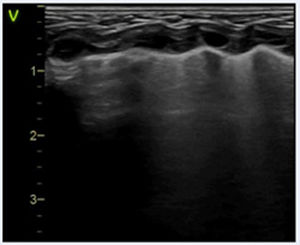
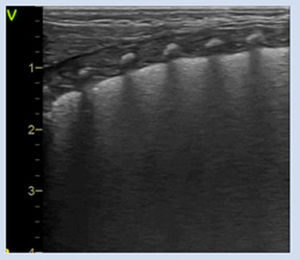
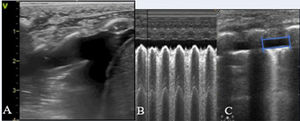
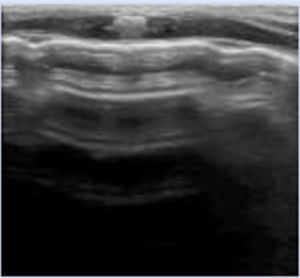
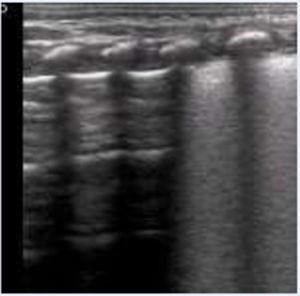
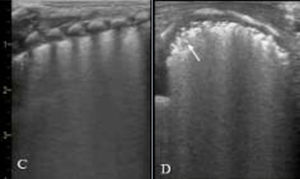
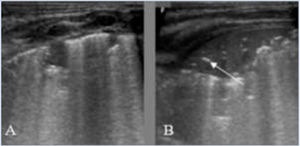
PneumothoraxThe sonographic features of pneumothorax are absence of lung sliding and of B-lines, exclusive presence of A-lines5 and the ‘lung point’ (LP), a sign that serves to locate the boundary between pneumothorax (absence of lung sliding) and any other lung pattern (with lung sliding) (Fig. 1, Video S5).
Pneumothorax. (A) Anterior longitudinal plane. Absence of lung sliding, absence of B-lines and clearly defined A-lines. (B) M-mode. Absence of lung sliding. Stratosphere sign: pleural line and clearly defined equidistant A-lines. (C) Transverse plane, 4th–5th intercostal space. Lung point (LP): sonographic sign that marks the boundary between pneumothorax (absence of lung sliding) and any other lung pattern (lung sliding). On ultrasound, pneumothorax is considered mild-moderate if the LP is in the mid-clavicular line or anterior axillary line and severe if it is posterior to the mid-axillary line.
Absence of pleural line, alveolar collapse with air bronchograms and lung tissue hepatization. Also characterised by the development of shred signs, irregular hyperechoic artefacts generated by the irregular boundary between consolidated lung tissue and aerated lung tissue (Fig. S6, Video S6).
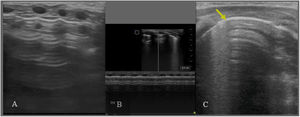
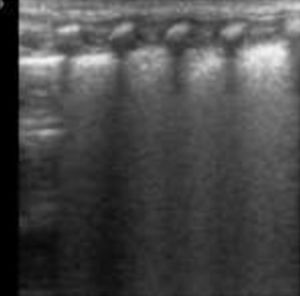
Pleural effusionIt has an easy to recognise pattern characterised by an anechoic area between the parietal and visceral pleura2,3 with a tendency for the effusion to accumulate in lower-level areas. The ‘quad’ sign may appear in 2D-mode, and the ‘sinusoid’ sign in M-mode. If the lung is compressed by the fluid, it will appear as lung consolidation with static bronchograms or even hepatization, and movement will create a lung flapping effect in the collapsed area known as the ‘jellyfish’ sign6 (Fig. 2, Video S7).
Pleural effusion. (A) Jellyfish sign, secondary collapse caused by pleural effusion (anechoic contents). (B) Sinusoid sign (M-mode), generated by the movement of the lung toward the parietal pleura with inspiration. (C) Quad sign (2D-mode): rectangular shape in which the anechoic area corresponds to the effusion, demarcated by the visceral pleura (below) and the parietal pleura (above) and on the sides by the shadows of a rib or the diaphragm.
Lung ultrasound is a valuable tool for assessment of lung aeration at birth (Fig. 3), as it can be used to confirm the presence of lung sliding, monitor alveolar recruitment during ventilation manoeuvres and detect potential complications during resuscitation.7
Ultrasound is also a quicker means to measure heart rate (HR), with a strong correlation with the values obtained by electrocardiogram (ECG) during cardiopulmonary resuscitation (CPR) in term neonates,8,9 and can help rule out other causes of pulseless electrical activity.
Recent protocols propose its use for aetiological diagnosis of sudden decompensation in previously stable neonates in the NICU setting (Sonographic Assessment of liFe-threatening Emergencies [SAFE])1 and SAFE-Revised (SAFE-R).10
Ultrasound assessment of lung transition and clearanceWhen it comes to the usefulness of LUS for assessment of lung fluid, one study analysed differences in lung clearance in term neonates based on the type of delivery, and found slower clearance in the first hours post birth in infants delivered by caesarean section (without labour) compared to vaginal birth.11 In newborn infants, the interlobular septae are thicker and the interstitial pattern is considered physiological, especially in the first hours post birth.
Recent observational studies in term and preterm neonates without respiratory distress have found evidence of lung aeration and partial clearance from the very first breaths and full lung clearance within 4 h of birth.12
Patterns for prediction of admissionKnowledge of the sonographic features of lung transition can help clinicians understand neonatal respiratory disease and assess the need for admission and/or respiratory support and/or early treatment (surfactant, chest drainage…). Thus, LUS can contribute to clinical decision-making from birth.
Lung patterns in term and late preterm neonates are easy to differentiate and reflect the pulmonary status of the infant. Thus, LUS performed between 60 and 120 min post birth in term and late preterm neonates is a highly accurate predictor of admission. The presence of white lung has a Sen of 77.7%, a Spe of 100% and a negative predictive value (NPV) of 97% in the prediction of admission.12
A recent prospective observational study that assessed the use of LUS for prediction of admission due to respiratory distress (respiratory distress syndrome [RDS] and transient tachypnoea of the newborn [TTN]) in term and late preterm neonates delivered by caesarean section had similar results, confirming the reliability of early LUS (performed at 30 min) for prediction of admission, with a positive predictive value (PPV) of 100% in the case of bilateral white lung and 54% in the case of unilateral white lung.14
Differential diagnosis of neonatal respiratory disease. Table 2Pneumothorax/PneumomediastinumLung ultrasound allows a quick and accurate diagnosis of pneumothorax, even in cases of subclinical leaks undetectable by plain radiography.7 However, lung sliding may also be absent in the context of selective intubation or lung hyperinflation.6 The presence of A-lines behind the sternum in the anterior mid-transverse plane has proven to be an easily identifiable sonographic feature with a high Sen, Spe and reproducibility for diagnosis of pneumothorax15 (Fig. S7, Video S8). The lung point is the most specific sign of pneumothorax and can help assess its severity based on its location relative to the different anatomical lines that define the regions of the thorax5 (Fig. 1C).
Differential diagnosis of neonatal respiratory disease.
| Disease | Ultrasound pattern | Figure | Video (link) |
|---|---|---|---|
| Pneumothorax | Anterior mid-transverse plane: | Video S8 | |
| • A-lines behind sternum (Figure S7) | |||
| Longitudinal plane: | |||
| • Absence of lung sliding | |||
| Transverse plane: | |||
| • Lung point | |||
| Transient tachypnoea of newborn | Heterogeneous pattern with variable involvement in different areas, with: | Video S9 | |
| • Normal lung pattern | |||
| • Interstitial pattern | |||
| • Alveolar-interstitial pattern | |||
| • Double lung point sign (50%) (Figure S9) | |||
| Mild changes in pleural line | |||
| Mild pleural effusion | |||
| Neonatal respiratory distress syndrome | Homogeneous alveolar-interstitial pattern (Fig. 4C) | Video S10 | |
| Irregular or thickened pleural line | |||
| Consolidations of variable size: | |||
| • Small subpleural collapses (Fig. 4D) or atelectasis | |||
| Subclinical pleural effusion | |||
| Transient respiratory distress (in term neonates) | Variable pattern: | Video S11 | |
| • Alveolar-interstitial, no consolidations (video S11) | |||
| • Normal pattern | |||
| • Minimal air leaks | |||
| Meconium aspiration syndrome | Patchy pattern with areas of: | Video S12 | |
| • Consolidations with air bronchogram (bilateral, variable size). Figure S12 B | |||
| • Alveolar-interstitial pattern | |||
| • Normal pattern | |||
| Pleural effusion | |||
| Dynamic features | |||
| Congenital pneumonia | Nonspecific pattern, varies depending on severity: | Video S13 | |
| • Interstitial pattern and/or | |||
| • Alveolar-interstitial with consolidations | |||
| Irregular, thickened pleural line | |||
| Subclinical pleural effusion |
The sonographic signs of pneumomediastinum have not been defined formally.1 In the suprasternal plane, depending on the severity, there can be large A-line artefacts (Fig. S8) or small hyperechoic lines in the lateral margins of the thymus or in the thymic parenchyma.16
Transient tachypnoea of the newbornFrom a pathophysiological perspective, TTN is characterised by oedema in a structurally mature lung. The sonographic appearance is heterogeneous: zones of normal aeration, interstitial pattern or even fields of white lung.3,13 The presence of an alveolar-interstitial pattern in a gradient, that is, more marked in lower-level areas (lung base or posterior fields) is known as ‘double lung point’ sign (Fig. S9, Video S9), a frequent sign found in nearly 50% of cases, although not specific to TTN.17 There may be abnormalities in the pleural line or pleural effusion, but consolidations are rarely present.3,17,18
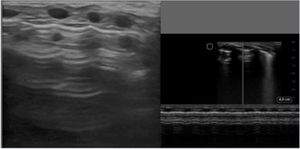
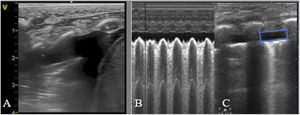
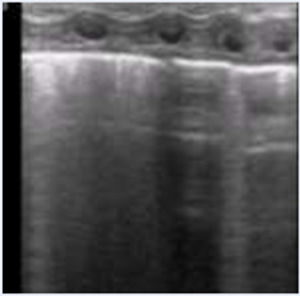
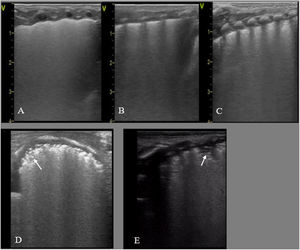
Neonatal respiratory distress syndromeRespiratory distress syndrome results from a primary (preterm neonates) or secondary (term neonates) deficiency of surfactant, and manifests with pulmonary oedema and decreased lung volume (collapse or atelectasis). It sonographic appearance is characterised by the loss of aeration with a homogeneous AI pattern and an irregular or thickened pleural line, resulting in a uniformly hyperechoic lung field (white lung),13 with condensations that may range from small subpleural collapses to large consolidations with air bronchogram (atelectasis), possibly associated with subclinical pleural effusion (Fig. 4, Video S10). Depending on the severity and course of disease, there may be different degrees of involvement in each field or hemithorax.1–3,19
Respiratory distress syndrome. A, B and C: preterm neonate born at 30+2 wk. Urgent caesarean section without prenatal steroids. Lung ultrasound at admission: (A) Anterior plane: homogeneous alveolar-interstitial pattern without areas of aeration (no A-lines) and irregular pleural line, white lung. (B) Lateral plane, similar findings. (C) Posterior plane: alveolar-interstitial pattern with pleural thickening and subpleural consolidations in lung base. (D) Transverse plane: alveolar-interstitial pattern with subpleural consolidations (arrow). (E) Posterior longitudinal plane with alveolar-interstitial pattern with pleural thickening, subpleural consolidations and consolidation with air bronchogram (atelectasis) in 2 intercostal spaces (arrow).
There is no characteristic pattern for transient respiratory distress in term neonates, characterised by mild symptoms and quick resolution with a few hours of respiratory support. There is frequently a patchy AI pattern without consolidations and/or a normal lung pattern, sometimes with minimal air leaks3 (Fig. S10, Video S11). Less frequently, there may be an AI pattern on a gradient or small consolidations. This heterogeneity may be due to the different pathophysiological mechanisms that can lead to respiratory distress. Usually, transient respiratory distress resolves quickly within 12–24 h, with normalization of clinical and sonographic features.20
Meconium aspiration syndromeThe ultrasound findings in meconium aspiration syndrome are heterogeneous and correlate to the variable severity of this disease. Published descriptions include the presence of consolidations with air bronchograms (bilateral, disperse and of variable size). There may also be a bilateral AI pattern, diffuse or patchy,21,22 with an irregular pleural line with areas of normal aeration and of pleural effusion (Fig. S11, Video S12). These features are dynamic, and their location may change with the course of disease.1
These features can also be seen in other forms of aspiration, such as aspiration of clear fluid, blood or milk, which have a more favourable sonographic presentation.
Congenital pneumoniaCongenital pneumonia presents with an interstitial or AI pattern associated with consolidations, an irregular and thickened pleural line and in some cases minimal pleural effusion23 in the context of risk factors for infection, respiratory distress and elevation of acute phase reactants (Fig. S12, Video S13).
Applicability of LUS in diagnostic and therapeutic protocolsLung ultrasound for prediction of surfactant administrationThere are several semiquantitative tools that assess the sonographic features of RDS and correlate well to parameters of oxygenation in preterm infants (oxygen index, alveolar-arterial oxygen gradient, the ratio of the oxygen saturation and the fraction of inspired oxygen [S/F ratio]) and the need of surfactant in infants delivered before 34 weeks24 (Table S3). The goal is to identify the need for surfactant administration earlier than allowed by traditional clinical criteria to also initiate treatment earlier and reduce the complications associated with delayed treatment.
In this regard, a cohort study in neonates delivered before 32 weeks used a LUS score to determine the need for surfactant and found a significant increase in the proportion of patients that received surfactant before 3 h post birth, with no increase in the total proportion of infants that received surfactant at any time.25 A randomised controlled trial in preterm neonates delivered before 32 weeks that received surfactant in the case of a LUS score greater than 8 or a FiO2 greater than 0.3 found significant differences in the timing of surfactant administration and greater S/F ratio values after surfactant administration in the group given surfactant based on the LUS, without significant differences in the proportion that received surfactant.26 Later studies have developed models for prediction of surfactant administration combining the LUS score and clinical parameters (S/F ratio). These models had an excellent predictive value, and both are now available for application as online calculators.27,28
There are few studies in preterm neonates delivered after 34 weeks are few and include few patients of vastly different characteristics, so their results must be interpreted with caution.13 One of them, conducted by Brat et al.,24 established a cut-off point with a low specificity, which limits its application in clinical practice. Contrary to extremely preterm neonates, respiratory disease in late preterm neonates is more diverse, with the possible coexistence of different diseases with similar clinical and sonographic features.
When it comes to the usefulness of LUS to predict the need of repeated doses of surfactant, only 2 studies in patients born before 32 weeks have been published to date24 that, in addition, used different criteria to determine the need of surfactant. Although the precision was good, the proposed cut-off points had a low sensitivity.
Monitoring and detection of complications in patients receiving respiratory supportOne of the main applications of LUS is the diagnosis of complications associated with ventilation, which justifies its integration in clinical practice for diagnostic purposes.
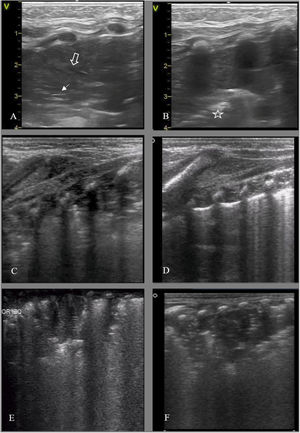
Lung ultrasound allows early detection of consolidations indicative of endotracheal tube (ETT) malposition (Fig. 5 A–B) or due to the decubitus position in patients with bronchopulmonary dysplasia (BPD). The combination of LUS findings and clinical manifestations increases the PPV of diagnosis of ventilator-associated pneumonia (VAP). A semiquantitative multiparameter score has been proposed for diagnosis of VAP that takes into account the most frequent sonographic findings of the disease: consolidations greater than 0.5 cm, bilateral consolidation, posterior consolidation, non-translobar consolidation and bronchogram (static, present in 100%, and dynamic, present in 70% of cases of VAP), highlighting the inability to completely reopen the consolidated area with the customary ventilation as a specific sign of VAP29 (Fig. 5C–F).
Detection of complications, forms of consolidation. A and B: Lung collapse/atelectasis due to endotracheal tube malposition. (A) Left anterior field: disappearance of pleural line with lung tissue hepatization and air bronchogram (hyperechoic, solid white arrow) and fluid (anechoic, hollow arrow). (B) Lateral field: absence of pleural line and hepatization, shred sign (hyperechoic border, boundary of collapsed lung/aerated lung) (star). (C) Preterm neonate born at 25+3 wk. Bronchopulmonary dysplasia. Consolidation/atelectasis in posterior field, disorganized bronchogram. (D) Same patient, follow-up ultrasound 2 h after change to prone position: resolution of consolidation. (E) Preterm neonate born at 23+5 wk, 50 h post birth, consolidation in left posterior field in the context of derecruitment. (F) Same patient at 35 days post birth, consolidation of homogeneous appearance in the clinical context compatible with ventilator-associated pneumonia.
Lung ultrasound can also be used to monitor oedema or extravascular lung fluid and optimise their management in neonates with poor lung clearance or congenital heart disease (CHD) and pulmonary overflow.30 Based on the severity of oedema, the sonographic appearance ranges from the interstitial to the AI pattern, possibly associated with pleural effusion.
Ultrasound-guided proceduresThoracocentesisThe size of the pneumothorax is determined based on the location of the lung point. Placing the infant in the supine position, the puncture site is chosen, ensuring it corresponds to the area where lung sliding is absent. In the case of pleural effusion, LUS allows quantification of its magnitude31 and can also guide thoracocentesis for releasing the fluid or for safer placement of a chest drain.
In both cases, ultrasound offers the advantage of allowing immediate verification of lung re-expansion (Fig. S13) and pulmonary follow-up until resolution.6
Verification of endotracheal tube placementDifferent approaches have been described to assess ETT placement32,33 and depth ETT34 by means of ultrasound (Fig. S14). However, there is a quick albeit indirect means to verify correct placement by confirming the presence of bilateral lung sliding with LUS.
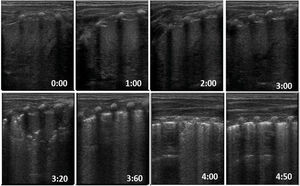
Lung ultrasound as a prognostic toolMonitoring and follow-up of lung development in preterm infants. Prediction of bronchopulmonary dysplasiaLung ultrasound is an adequate tool to predict the development of bronchopulmonary dysplasia (BPD) in infants born preterm before 32 weeks of gestation: several multicentre studies35–37 demonstrate that a LUS score similar to the one used to predict the need of surfactant performs well for diagnosis of BPD from as early as 3 days post birth, although the optimal timing for its use is 1 week post birth.
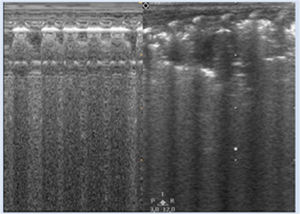
The usual evolution of pulmonary patterns in neonates delivered before 32 weeks starts with a pattern characteristic of RDS at birth, with high LUS score values in the first days, but then normally improve thereafter as the primary surfactant deficiency resolves, reaching LUS score values near 0 at around 1 week post birth.38 The patients whose LUS scores do not exhibit this decrease or actually increase are more likely to develop BPD (Fig. 6). On the other hand, in preterm infants born before 28 weeks, this decrease in the LUS score delays, even after the initial surfactant deficiency stage has passed, to up to 4 weeks post birth39–41 (Table S4).
Sonographic evaluation in the first week of life in preterm neonate born at 25 weeks whose mother developed chorioamnionitis and was a carrier of Ureaplasma parvum in cervical fluid. (A) Normal pattern at 4 h post birth. (B) Day 3 post birth: alveolar-interstitial pattern with pleural thickening and fragmentation of the pleural line only in posterior fields. (C) Week 1 post birth: the same abnormal features are visible in every lung field. At this point, the respiratory support needs of the patient did not increase significantly, but starting from 2 weeks post birth she required aggressive scalation of ventilatory parameters and eventually developed severe bronchopulmonary dysplasia.
Lung ultrasound is an ideal technique for assessment of lung aeration, lung fluid and alveolar collapse, information that is crucial for the dynamic monitoring of pulmonary status and the response to treatment, including changes in respiratory support, adjustment of fluids, etc.
Studies in preterm neonates have found a correlation between semiquantitative assessment instruments and oxygen saturation,24 the probability of NIV13 as early as the delivery room42 and the need of invasive mechanical ventilation (IMV). However, further research is required to determine whether changes in non-invasive or invasive ventilation parameters are reflected in changes in LUS scores.
Lung ultrasound also plays a key role in decision-making regarding weaning from IMV in combination with the clinical assessment, diaphragmatic ultrasound and respiratory parameters, as it allows ruling out complications and assessing the degree of lung aeration taking into account the lung features associated with the underlying disease and gestational age35,43,44 (Fig. 5C and D).
Other diseasesCongenital lung malformationsIn most cases, lung malformations are suspected before birth. The attenuation or resolution of abnormal features in prenatal imaging, the absence of clinical manifestations or a normal chest radiograph do not exclude the presence of congenital lung malformations.
Early performance of LUS at birth before the lungs are fully aerated can detect lung malformations. There are consolidation patterns of varying extent, with or without hypoechoic cystic lesions within, with or without air bronchograms and in some instances afferent vessels arising from the systemic circulation (Fig. S15).45,46
Congenital diaphragmatic herniaThe affected area is characterised by a pattern of consolidation involving solid organs, or round shapes with moving hyperechoic artefacts (air) inside, in the case of the bowel. The scant surrounding lung parenchyma is characterised by an AI pattern with a thickened pleural line that is typical of pulmonary hypoplasia. The mediastinum is displaced toward the contralateral hemithorax in the transverse plane, while the sonographic appearance of the lung that is not affected is usually normal (Fig. S16).47,48
In the subcostal plane, there is a discontinuity in the hyperechoic line that demarcates the diaphragm.
Congenital chylothoraxIn addition to the previously described features pleural effusion, there are usually abnormalities in the pleural line (thickened and irregular with subpleural collapses) that persist for weeks, even in patients in whom the accumulation resolves spontaneously before birth, which is attributed to the pleural inflammation caused by the prolonged presence of chyle in the pleural space.49
Application in postoperative care after cardiac surgeryLung ultrasound has proven useful for monitoring of pulmonary oedema, diagnosis of atelectasis and ultrasound-guided recruitment manoeuvres and detection of postoperative complications (pleural effusion, pneumothorax or haematomas).50,51
The assessment of the diaphragm by means of ultrasound is important given the prevalence of diaphragmatic paralysis secondary to trauma and its impact on lung function.
From a functional perspective, there is a correlation between different semiquantitative LUS scoring systems and the duration of mechanical ventilation or the length of stay, and their inclusion can increase the predictive power of multiparametric models based on clinical variables.52
Thus, LUS should be recommended in the non-invasive monitoring required for the daily evaluation of cardiac patients, as it offers useful information that may contribute to improved management.
ConclusionThe use of LUS in neonatal units is increasing in parallel to the mounting evidence that it should be considered the gold standard for diagnosis of neonatal respiratory disease. Although the scientific evidence already calls for a change in practice and the inclusion of this technique in the routine protocols for management of respiratory distress in neonates, further, more thorough research conducted in multiple centres is still required. The use of LUS can extend to the assessment of the diaphragm and airway and other applications that should be subject to further study. The Section on Lung Ultrasound of the Working Group on Ultrasound of the SENeo was created with the aim of supporting the widespread introduction of LUS in clinical practice and promote research on subjects of interest, such as the application of sonographic criteria to the prognosis of preterm infants that require surfactant administration or the usefulness of LUS for monitoring of NIV/IMV or in the weaning of IMV.
FundingThis work has not received any type of funding.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Fernández LR, Hernández RG, Guerediaga IS, Gato JM, Fanjul JR, Bilbao VA, et al. Utilidad de la ecografía pulmonar en el diagnóstico y seguimiento de la patología respiratoria neonatal. An Pediatr (Barc). 2022;96:252.