Suppurative acute otitis media (AOM) is defined as the acute and symptomatic presence of exudate and inflammation in the middle ear. The presence of otorrhoea in AOM is considered a risk factor and an indication for prescribing systemic antibiotherapy. The use of topical antibiotherapy is widespread in both inpatient and outpatient emergency departments, in spite of the fact that the most recent evidence only supports its use in patients with tympanostomy tubes (TTs), which is what is recommended in current protocols.1 Topical ciprofloxacin is the first-line agent, and the use of local steroids is not recommended due to the lack of standardised clinical trials evaluating their efficacy.
The aim of our study was to analyse the use of topical antibiotherapy in suppurative AOM by paediatricians, and whether it conforms to the current recommendations of scientific societies. To this end, we developed an online questionnaire with 9 questions and conducted a survey of medical intern-residents in paediatrics, primary care paediatricians and hospital-based paediatricians from 6 hospitals (2 of which were tertiary care centres) and 3 primary care centres between November and December of 2023. We used the Google Forms platform to upload the questionnaire as an online form, and provided access to it to potential participants through the distribution of a QR code.
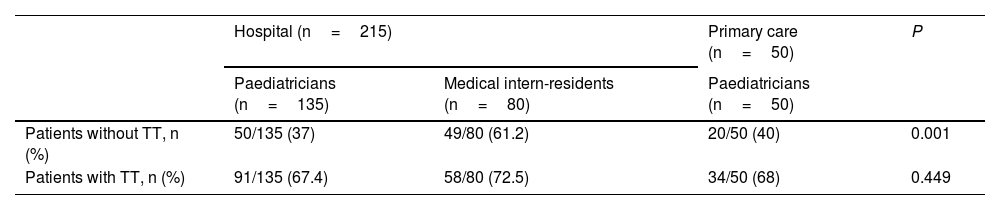
We received 265 valid responses. Of this total, 69.8% (185/265) were submitted by paediatricians and 30.2% (80/265) by medical intern-residents. In addition, 18.8% worked in primary care and 81.1% in hospital. Of all respondents, 44.9% (119/265) reported using topical antibiotherapy in patients with suppurative AOM who did not carry TTs, a percentage that increased to 61.2% in medical intern-residents (P<0.001). In the case of patients with TTs, the percentage rose to 69.1% (183/265), with no significant differences based on the care setting or professional category (Table 1). Furthermore, 4.2% reported prescribing topical antibiotherapy alone, without the addition of a systemic antibiotic. Ciprofloxacin was the most frequently used topical antibiotic, prescribed as monotherapy (71.5%) or combined with steroids (41.6%). Last of all, 65.2% of respondents considered that topical treatment improved outcomes in cases of suppurative AOM.
Use of topical antibiotherapy for suppurative AOM based on care setting and professional category.
| Hospital (n=215) | Primary care (n=50) | P | ||
|---|---|---|---|---|
| Paediatricians (n=135) | Medical intern-residents (n=80) | Paediatricians (n=50) | ||
| Patients without TT, n (%) | 50/135 (37) | 49/80 (61.2) | 20/50 (40) | 0.001 |
| Patients with TT, n (%) | 91/135 (67.4) | 58/80 (72.5) | 34/50 (68) | 0.449 |
AOM, acute otitis media; TT, tympanostomy tube.
Our study evinces the heterogeneity among health care providers in the use of topical antibiotherapy for AOM. Almost half of respondents, independently of the care setting, did not adhere to current recommendations, especially in the group of physicians in training. The use of topical antibiotics, alone or in combination with systemic antibiotics, for management of suppurative AOM remains controversial. The protocol of the Sociedad Española de Infectología Pediátrica (Spanish Society of Paediatric Infectious Disease)1 and updated treatment guidelines published in Italy based on recent evidence2 do not recommend prescription of topical antibiotherapy for suppurative AOM in the general paediatric population. However, the latest consensus documents on the management of AOM published in Spain barely address topical treatment.3,4 The most recent paediatric otorhinolaryngology guideline from 2022 only recommends it for use in patients with TTs.5 A multicentre study demonstrated the superiority of the combination of topical antibiotic and steroid therapy over oral antibiotherapy, so this could be considered a valid treatment option in this particular group of patients.6 Otorrhoea is a common complication in patients with TTs following their insertion, and it usually results from a viral infection with bacterial superinfection and biofilm formation, for which treatment with topical antibiotics is effective; however, these outcomes should not be extrapolated to patients without TTs who present with spontaneous perforation.
Ciprofloxacin was the topical antibiotic respondents prescribed most frequently for suppurative AOM, and up to 41.6% reported prescribing it combined with topical steroids, a combination that is not currently recommended in clinical guidelines.
The main limitation of our study is the small sample size, it was challenging to assess the degree of participation bias since it was an online survey and respondents’ answers may have differed from actual clinical practice. Nevertheless, the results suggest that the prescription of topical antibiotics for suppurative AOM is a widespread practice in paediatric care and that prescribing practices in these providers are not in adherence with the latest recommendations.