Juvenile idiopathic arthritis (JIA) is the most prevalent chronic inflammatory joint disease in the paediatric age group, and it affects one in two thousand children aged less than 16 years. It is a diagnosis by exclusion that encompasses all cases of arthritis of unknown aetiology of more than six weeks duration and with onset prior to age 16 years. There are seven clinical subtypes, the most common of which is oligoarticular JIA.
The disease may have different extra-articular manifestations, of which JIA-associated uveitis (JIAU) is the most prevalent, affecting 12%–20%1 of patients.
On account of its singularity, we present the case of a girl aged 7 years with silent oligoarticular JIA and chronic anterior uveitis whose first symptom was unilateral amaurosis.
The patient sought care in our emergency department in August of 2015 for esotropia and redness in the right eye. The girl reported conjunctival hyperaemia, hyperlacrimation and photophobia in the right eye (RE) lasting six months, for which she had sought care in other health care facilities in the past and received a diagnosis of allergic conjunctivitis.
On ophthalmologic examination, she exhibited amaurosis in the RE, which did not perceive light, a fact that had not been noticed by either the patient or her family, with normal visual acuity in the left eye. Slit-lamp biomicroscopy revealed band keratosis, with multiple thick keratic precipitates in the middle and lower third of the cornea and grade 3+ cells and flare. She also had a white cataract with 360° synechiae (Fig. 1). The intraocular pressure was 3mmHg (normal range, 11–21mmHg). Since a fundus examination was not possible due to the presence of the cataract, the patient underwent an ultrasound examination of the eye that revealed no abnormalities in the vitreous body or posterior chamber.
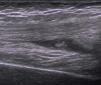
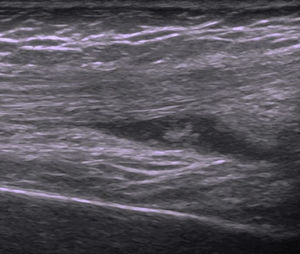
A diagnosis of cataract and acute uveitis was made and treatment with topical corticosteroids initiated, and the patient was referred to paediatric rheumatology for assessment. During the anamnesis, the patient did not report any joint pain or systemic symptoms or any relevant personal or family history. The physical examination revealed a mild synovial fluid leak in the right knee that was painless and did not impair mobility, which was confirmed by ultrasonography (Fig. 2). The results of the antinuclear antibody test (ANA) were negative, and the patient received a diagnosis of ANA-negative oligoarticular JIA.
The patient was given intra-articular steroid injections in the affected knee and methotrexate (15mg/m2/week) via the subcutaneous route in addition to the ongoing topical ophthalmologic treatment. Seven months after achieving resolution of the ophthalmologic and articular symptoms, the patient underwent surgery to break the irido-crystalline synechiae and remove the cataract by phacoemulsification and aspiration due to the hardness of the lens core. Ten days after the surgery, the patient exhibited a visual acuity of 0.05 in the RE.
The most frequent form of JIAU is chronic anterior uveitis (CAU), characterised by the presence of cells (Tyndall effect) and proteins (flare) in the anterior chamber and the formation of goniosynechiae. Unlike acute HLA-B27-associated anterior uveitis, which manifests with red eye, pain and photophobia, CAU does not usually manifest with ophthalmologic symptoms, as had been the case in our patient.
Before the association between JIA and uveitis became known, it was not uncommon for uveitis to be the main cause of morbidity in patients with oligoarticular JIA, and in fact JIAU continues to be one of the main causes of vision loss in developed countries.2 For this reason, it is recommended that all patients with JIA undergo screening for uveitis within one month from diagnosis and every three to twelve months thereafter, based on their risk of developing it.3
The risk factors for developing JIAU include clinical variables (age of less than 6 years at onset and duration of symptoms of less than four years) and especially laboratory variables (positive ANA test).
Juvenile idiopathic arthritis-associated uveitis usually develops in the first four to six years following diagnosis, although it can predate arthritis in 10% to 15% of patients,4 as was the case in our patient, or many years after. The course of ophthalmologic disease is independent of the course of arthritis. The possible ophthalmologic complications of JIAU include cataracts, band keratopathy or glaucoma,5 and even blindness in up to 10% of patients,6 which develops in those who do not respond to treatment and long after the onset.
Our patient illustrates the need to remain aware that CAU is usually asymptomatic and that its most common aetiology is JIA, as she had been seen at different levels of care in the months previous to her visit to the emergency department, and the delay in the diagnosis had consequences. It also underscores the need to appropriately coordinate paediatric ophthalmologic and rheumatology services so that comprehensive treatment can be initiated with the least possible delay.
Please cite this article as: Rubio San Simón A, Ortueta Olartecoechea A, Barral Mena E, Tejada Palacios P, de Inocencio Arocena J. Amaurosis unilateral como síntoma inicial de artritis idiopática juvenil. An Pediatr (Barc). 2017;86:352–353.