Behavioural disorders and learning disabilities are often recognised in <1500g or <32 weeks very low birth weight (VLBW) infants. There is very limited data in the Spanish population.
ObjectiveTo determine the presence of psychosocial disorders in preterm infants at 6 years of age, as assessed by the strength and difficulties (SDQ) questionnaire, in comparison to a reference population. To set a cut-off value to use SDQ as a screening tool for attention deficit hyperactivity disorder (ADHD) in the preterm child.
Participants and methodsA prospective observational study was conducted on premature children assessed at 6 years of age using the SDQ. Perinatal variables, neurodevelopment, and diagnosis of ADHD, according to the DSM-5, were collected.
ResultsA total of 214 children who met all the requirements, were included. When compared with the reference population they had significantly higher scores in emotional symptoms, in peer relationships, and in the total score of the test. The hyperactivity scale and the total test score are good predictors of a diagnosis of ADHD, with an area under the ROC curve of 0.83 (95% CI: 0.76–0.90) for hyperactivity, and 0.87 (95% CI: 0.80–0.93) for the total score. The scores for hyperactivity and the total test, from which the screening for ADHD could be considered positive would be ≥6 and ≥13 respectively, and a combination of hyperactivity ≥5 and total score ≥12.
ConclusionsPreterm children are at higher risk of emotional and peer relationship problems than those born full term. The SDQ test could be used for ADHD screening.
Los trastornos del comportamiento y del aprendizaje se describen con frecuencia en <1.500g o <32 semanas (RNMBP/MP). Se dispone de muy poca información en población española.
ObjetivoIdentificar los problemas psicosociales de los RNMBP/MP mediante la aplicación del test Strength and Difficulties Questionnaire (SDQ) a los 6 años y comparar los resultados con los de una población de referencia. Establecer los puntos de corte para el uso del SDQ como cribado del trastorno por déficit de atención e hiperactividad (TDAH) en RNMBP/MP.
Participantes y métodosEstudio prospectivo observacional en RNMBP/MP evaluados a los 6 años con SDQ. Se recogen variables perinatales, neurodesarrollo y diagnóstico de TDAH mediante DSM-5.
ResultadosSe incluyeron 214 niños con el total de las valoraciones. Comparados con la población de referencia obtuvieron puntuaciones significativamente mayores en síntomas emocionales, relaciones con compañeros y en el total del test. La escala de hiperactividad y la puntuación total se identifican como buenos predictores del diagnóstico de TDAH, con un área bajo la curva ROC de 0,83 y 0,87, respectivamente. Las puntuaciones que consiguen una adecuada sensibilidad para el cribado de TDAH son ≥6 para la escala de hiperactividad y ≥13 para la puntuación total del test, y una puntuación combinada ≥5 en hiperactividad junto con un total ≥12.
ConclusionesLos RNMBP/MP presentan más frecuentemente problemas emocionales y de relación que sus compañeros nacidos a término. El test SDQ podría utilizarse como una prueba de cribado para el TDAH.
It is well known that children born preterm with weights of less than 1500g (very low birth weight [VLBW]) or before 32 weeks’ gestation (very preterm [VPT]) may experience cognitive impairment, cerebral palsy or blindness,1 the incidence of which has been decreasing thanks to advances in medicine. However, at the same time, there is a growing body of evidence on the presence of other impairments in learning, behaviour and emotional regulation, which may develop in up to 1/3 of children born with VLBW/VPT, but there are no widespread validated tools for their detection in this population.2,3
The most frequently reported psychiatric sequelae in these patients is attention-deficit hyperactivity disorder (ADHD), with a prevalence that is double that found in children born at term, with a predominance of the inattentive type, and an influence in prevalence of other factors, such as the socioeconomic level of the household.2,4 Many studies in the literature have also described an increased prevalence of autism spectrum disorders (with a predominance of difficulties in social communication and interaction as opposed to stereotyped behaviours), and the presence of anxiety and depression in up to 8% of children born with VLBW/VPT.5,6 These disorders, combined with an increased risk of motor and cognitive impairments in the VLBW/VPT population, lead to impaired academic performance in these patients, with the proportion needing academic support and special education exceeding that in their peers born to term by 10% and 17%, respectively, which constitutes a significant social and economic burden.7
An early diagnosis allowing intervention in the early stages of many of these psychosocial disorders may result in better outcomes, with improvement of social skills and academic performance.8,9 Thus, a screening programme ought to be established for the detection of these disorders, as has been done for ADHD in the general population in countries such as the United Kingdom.8,10 There are numerous tests for the early detection of behavioural and psychosocial problems; one of the most widely used is the strengths and difficulties questionnaire (SDQ), a simple instrument validated for the overall assessment of behavioural, social and emotional problems.11
For all the reasons noted above, the main objective of our study was to detect emerging psychosocial problems in children born with VLBW/VPT through the administration of the SDQ at age 6 years, and to compare the results with those in a reference population of children born at term. We also established cut-off points for the use of the SDQ for screening of ADHD in children born with VLBW/VPT.
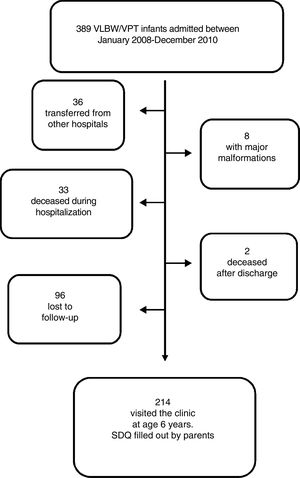
Materials and methodsStudy sampleWe included children born with VLBW/VPT that had been followed up until at least age 6 years in a clinic devoted specifically to the follow-up of children born preterm. We excluded infants transferred from other health care facilities, patients with major congenital malformations, newborns that died in the delivery room or during the follow-up through age 6 years and children lost to follow-up in that period. Fig. 1 shows a flow chart of the inclusion of patients in the study.
We calculated the sample size taking as reference the study by Barriuso-Lapresa et al.12 to detect differences in the total score of the SDQ with a power of 90% and an alpha level of 0.05. We estimated that we needed to include 207 patients.
We included 214 children born with VLBW/VPT that had been followed up until age 6 years and whose parents filled out the questionnaire.
We conducted the study in a level III-C neonatal unit that manages approximately 120 VLBW/VPT patients a year, with approximately 500 admissions to neonatal intensive care per year.
Study designWe conducted a prospective observational cohort study.
InstrumentsThe SDQ version for parents includes 25 items, each with 3 possible answers: not true (0 points); somewhat true (1 point) and certainly true (2 points). It assesses dimensions or domains of mental health: emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems and prosocial behaviour. The points in each dimension are added to obtain a score that ranges from 0 to 10, with higher scores reflecting poorer outcomes except in the prosocial behaviour dimension, which goes in reverse. The addition of the scores of the first 4 dimensions (leaving out the prosocial behaviour dimension, which is scored in reverse) produces the total difficulties score of the SDQ, which ranges from 0 to 40, with higher scores representing a poorer mental health.11,12 In our study, the questionnaire was always filled out by a parent during the visit while the neonatologist assessed the child. A previous study that analysed the reliability of the total score of the parents’ version of the SDQ found Cronbach α values of 0.77–0.82 and McDonald's omega values of 0.87–0.90.13
We assessed the severity of intraventricular haemorrhage applying the Papile classification (with 4 grades) and neurodevelopment at age 2 years by means of the Bayley II scale.14,15
Study protocolThe children included in the study were managed in a programme for the specific follow-up of children born with VLBW/VPT. This programme includes a routine series of scheduled checkups that are performed in every child regardless of clinical status. One of the tests included in this framework is the administration to all parents of the SDQ when the child is about 6 years of age. We compared the SDQ scores in our sample of children born preterm in our hospital with the scores of a control group of children born to term aged 6 years, which we obtained from a large population-based study conducted in Spain that used the SDQ version for parents.12
As a secondary objective, we collected data on perinatal and follow-up variables in the population of children born preterm.
Lastly, we assessed the use of the SDQ for screening of ADHD. For this purpose, children underwent an assessment for ADHD through an interview with one of the 2 child psychiatrists in our hospital, who diagnosed ADHD based on the DSM-5 criteria, currently considered the reference for diagnosis of this disorder due to the high interrater reliability observed for each item and for the overall diagnosis.16,17 We referred children that reported symptoms of hyperactivity or inattention to the psychiatrist for assessment.
The follow-up of the children included in the study adhered to the customary protocol. They did not undergo any additional tests or assessments nor had additional appointments for the purpose of the study. The study was approved by the clinical research ethics committee of our hospital.
Statistical analysisWe compared the scores in the SDQ in the sample under study and the control group with the nonparametric Mann–Whitney U test, as the data did not follow a normal distribution, analysing the differences in the median and interquartile range. We defined statistical significance as a P-value of less than 0.05. The analysis was performed with the software IBM SPSS Statistics version 20. To assess the discriminatory power of the hyperactivity score and the total score in relation to the diagnosis of ADHD, we computed receiver operating characteristic (ROC) curves. To assess the usefulness of the questionnaire to screen for ADHD, we calculated the sensitivity, specificity and positive and negative likelihood ratios – with their 95% confidence intervals – of the SDQ using lower-than-usual cut-off points.
ResultsTable 1 summarises the perinatal characteristics in the neonatal and follow-up periods of the sample under study.
Clinical characteristics of the sample.
| Mean age (years) | 5.91±0.73 |
| Male sex (%) | 53.7% |
| Mean gestational age (weeks) | 29.32±2.92 |
| Mean birth weight (g) | 1203.51±377.70 |
| Birth weight below 10th percentile (%) | 23.4% |
| Presence of neonatal intraventricular haemorrhage (IVH) and grade (%) | No IVH: 74.3%IVH I: 12.6%IVH II: 6.1%IVH III: 5.1%IVH IV: 1.4% |
| Neonatal ventriculomegaly and classification (%) | No ventriculomegaly: 72%Ventriculomegaly grade I: 18.7%Ventriculomegaly grade II: 6.5%Ventriculomegaly grade III: 2.8% |
| Neonatal intraparenchymal lesions and classification (%) | No parenchymal lesions: 76.2%Hyperechogenicity: 15%Infarction: 4.2%Leukomalacia: 1.9%Another type: 2.8% |
| Bayley II mental developmental index at age 2 years | 98.46±15.17 |
| Developmental impairments at age 4 years (%) | 7.9% |
| Motor impairments at age 4 years (%) | 5.1% |
| Behavioural problems and subtypes at age 4 years (%) | Normal: 62.6%Hyperactive/impulsive: 19.7%Dependent/withdrawn: 13.1%Other: 4.6% |
| Language delay at age 4 years (%) | 4.6% |
| Deafness at age 4 years (%) | 2.4% |
Table 2 presents the results of comparing the SDQ scores of the children born preterm included in our study and of the reference population.12 We found statistically significant differences in the comparison of means for the presence of emotional symptoms, relationships with peers and the total score.
Median and interquartile range of the scores in each scale and the entire SDQ in children born preterm with a weight of less than 1500g or before 32 weeks’ gestation and in the control group, compared by means of the Mann–Whitney U test.
| VLBW/VPT group | Control group of children born at term12 | P | |
|---|---|---|---|
| Emotional symptoms | 2 (1–4) | 1 (0–3) | =.0173 |
| Hyperactivity | 5 (3–7) | 5 (3–7) | =.8614 |
| Conduct | 2 (1–3) | 2 (1–3) | =.5751 |
| Peer relationships | 1 (0–3) | 1 (0–3) | =.0436 |
| Prosocial behaviour | 9 (8–10) | 9 (8–10) | =.7502 |
| Total SDQ | 11 (7–16) | 9 (6–13) | <.001 |
SDQ, strengths and difficulties questionnaire; VLBW/VPT: born with very low birth weight <1500g or very preterm before 32 weeks’ gestation.
Table 3 compares the total SDQ scores based on specific perinatal, follow-up and sonographic characteristics. In our sample, the prevalence of ADHD was of 15.4%, with a higher risk in children born very preterm at or before 28 weeks’ gestation (OR, 2.54; 95% CI, 1.19–5.40).
Difference in the total SDQ score (mean±standard deviation) based on the characteristics of patients included in the sample, obtained by means of the Student t test.
| Total SDQ | Difference between means (95% CI) | P | |
|---|---|---|---|
| Sex | |||
| Male (n=115) | 12.03±6.17 | 1.66 (0.01–3.32) | <.05 |
| Female (n=98) | 10.36±5.99 | ||
| Birth weight | |||
| 1000g (n=62) | 13.34±5.43 | 2.93 (1.1–4.7) | =.01 |
| >1000g (n=151) | 10.40±6.12 | ||
| Gestational age | |||
| <28 weeks (n=61) | 12.08±5.12 | 1.15 (−0.67–2.98) | =.21 |
| ≥28 weeks (n=152) | 10.93±6.28 | ||
| Gestational age VLBW/VPT with weight adequate for gestational age | |||
| <28 weeks (n=58) | 12.06±5.16 | 2.05 (0.25–3.86) | <.03 |
| ≥28 weeks (n=105) | 10.00±5.82 | ||
| Small for gestational age | |||
| Adequate weight (n=163) | 10.74±5.66 | 2.19 (0.25–4.13) | <.03 |
| Low weight (n=50) | 12.94±7.18 | ||
| IVH | |||
| No IVH (n=159) | 10.71±6.05 | 2.14 (0.27–4.01) | <.03 |
| IVH (n=55) | 12.85±6.11 | ||
| IVH 1 and 2 | |||
| No IVH (n=159) | 10.71±6.05 | 1.89 (−0.24–4.01) | =.8 |
| IVH I and II (n=40) | 12.60±6.32 | ||
| IVH 3 and 4 | |||
| No IVH (n=159) | 10.71±6.05 | 2.93 (0.19–6.25) | <.05 |
| IVH III (n=14) | 13.64±5.86 | ||
| BMDI at age 2 years | |||
| BMDI<85 (n=30) | 13.60±6.14 | 2.84 (0.41–5.28) | <.03 |
| BMDI≥85 (n=165) | 10.75±6.22 | ||
BMDI, Baily mental developmental index; IVH, intraventricular haemorrhage; SDQ, strengths and difficulties questionnaire; VLBW/VPT, born with very low birth weight <1500g or very preterm before 32 weeks’ gestation.
A total of 33 patients received a diagnosis of ADHD. Table 4 compares the scores in the SDQ of patients with and without ADHD. We found that the scores in the hyperactivity scale and the entire SDQ were higher in patients with ADHD compared to those without ADHD.
Differences in the hyperactivity scale and total SDQ scores (mean±standard deviation) between patients with and without a diagnosis of ADHD, obtained by means of the Student t test.
| No ADHD(n=181) | ADHD(n=33) | Difference between means (95% CI) | P | |
|---|---|---|---|---|
| Hyperactivity score | 4.24±2.51 | 7.55±2.11 | 3.30 (2.38–4.22) | <.01 |
| Total SDQ score | 10.01±5.49 | 18.12±4.77 | 8.11 (6.10–10.12) | <.01 |
ADHD, attention-deficit hyperactivity disorder; SDQ, strength and difficulties questionnaire.
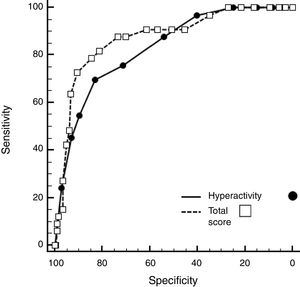
Fig. 2 presents the ROC curves of the hyperactivity scale and the total score of the SDQ in relation to the diagnosis of ADHD. In both cases, the area under the curve demonstrates a good correlation with the diagnosis of ADHD, with a 95% confidence interval, of more than 0.75 for both. When it came to the total SDQ score, the area under the curve was greater (0.87) compared to the hyperactivity scale score (0.83), although the difference between the two was not statistically significant (0.043; P=.26). The association was weaker for the rest of the scales in the questionnaire, with an area under the curve of 0.753 for the conduct scale, 0.751 for the peer relationship scale, 0.65 for the emotions scale and 0.37 for the prosocial behaviour scale.
Table 5 presents the sensitivity, specificity and positive and negative likelihood ratios obtained with the application of different cutoffs in the total score and the hyperactivity score of the SDQ, as well as a combination of both, for screening of ADHD. The scores that achieved an adequate sensitivity for screening of ADHD were 6 or higher in the hyperactivity scale and 13 or higher for the total score, or the combination of a score of 5 or higher in the hyperactivity scale and a total score of 12 or higher.
Sensitivity, specificity and positive and negative likelihood ratios, all with their 95% confidence intervals, for the detection of ADHD obtained with the application of different cut-off points in the hyperactivity scale score, the total SDQ score and a combination of both.
| Sensitivity | Specificity | LR+ | LR− | n (%) | |
|---|---|---|---|---|---|
| Hyperactivity≥3 | 1 (0.98–1) | 0.24 (0.18–0.31) | 1.33 (1.22–1.45) | 0 | 169 (79) |
| Hyperactivity≥4 | 0.97 (0.89–1) | 0.40 (0.32–0.47) | 1.63 (1.42–1.82) | 0.08 (0.01–0.52) | 140 (65) |
| Hyperactivity≥5 | 0.88 (0.75–1) | 0.54 (0.46–0.61) | 1.95 (1.56–2.35) | 0.22 (0.09–0.57) | 112 (52) |
| Hyperactivity≥6 | 0.76 (0.59–0.91) | 0.71 (0.64–0.78) | 2.64 (1.95–3.56) | 0.34 (0.18–0.63) | 77 (35) |
| Hyperactivity≥7 | 0.70 (0.52–0.86) | 0.83 (0.77–0.88) | 4.07 (2.75–6.02) | 0.36 (0.22–0.62) | 54 (25) |
| Total SDQ≥11 | 0.91 (0.79–1) | 0.56 (0.49–0.64) | 2.11 (1.73–2.57) | 0.16 (0.05–0.47) | 108 (50) |
| Total SDQ≥12 | 0.91 (0.79–1) | 0.61 (0.54–0.68) | 2.35 (1.90–2.91) | 0.15 (0.05–0.44) | 100 (46) |
| Total SDQ≥13 | 0.88 (0.75–1) | 0.70 (0.63–0.77) | 2.95 (2.28–3.81) | 0.17 (0.07–0.44) | 83 (39) |
| Total SDQ≥14 | 0.87 (0.75–1) | 0.73 (0.66–0.80) | 3.31 (2.52–4.36) | 0.16 (0.07–0.42) | 77 (36) |
| Total SDQ≥15 | 0.81 (0.67–0.96) | 0.81 (0.75–0.87) | 4.36 (3.09–6.14) | 0.23 (0.11–0.46) | 61 (28) |
| Hyperactivity≥3+total SDQ≥12 | 0.90 (0.79–1) | 0.63 (0.55–0.70) | 2.46 (1.97–3.06) | 0.14 (0.05–0.43) | 97 (45) |
| Hyperactivity≥4+total SDQ≥12 | 0.87 (0.75–1) | 0.66 (0.59–0.73) | 2.65 (2.08–3.38) | 0.19 (0.07–0.46) | 89 (41) |
| Hyperactivity≥5+total SDQ≥12 | 0.81 (0.67–0.96) | 0.71 (0.64–0.78) | 2.85 (2.15–3.77) | 0.26 (0.12 –0.53) | 79 (37) |
| Hyperactivity≥5+total SDQ≥13 | 0.78 (0.63–0.94) | 0.76 (0.69–0.82 | 3.32 (2.42–4.55) | 0.29 (0.14–0.54) | 69 (32) |
n (%): absolute frequency and percentage of children that reached the cutoff.
ADHD, attention-deficit hyperactivity disorder; LR−, negative likelihood ratio; LR+, positive likelihood ratio; SDQ, strength and difficulties questionnaire.
The administration of the SDQ in a large sample of Spanish children born with VLBW/VPT at age 6 years revealed a significantly larger number of psychosocial problems compared to the frequency found in a reference population of children born to term.12 We mainly found differences in the emotional dimension and in the relationships with peers. We also propose cut-off points for the use of the SDQ in patients born preterm as a tool for screening ADHD during childhood. We did not find any references in the Spanish medical literature on the use of the SDQ in children born preterm, and the data from international studies is scarce.18,19
Our findings were consistent with those of other studies conducted in children born preterm using more complex assessment tools (Child Behavior Checklist or the Swanson, Nolan and Pelham scale) that have identified difficulties in interpersonal relationships, inattention or anxiety as the most frequent problems.20–23 One aspect we ought to highlight in our findings was the lack of a statistically significant difference between groups in the hyperactivity scale, even though it is known that the prevalence of ADHD is greater in children born preterm. One explanation for this finding is the different ADHD subtypes, as only the inattentive type of ADHD is more frequent in children born preterm, as described by Jaekels et al. or Brogan el al.4,24 We did not find significant differences in the conduct scale. However, an article published in the framework of the EPICure study did report statistically significant differences in the conduct scale,3 possibly because the study only included children born very preterm, before 26 weeks’ gestation, which was therefore a very different population from the one evaluated in our study.
Two studies stand out among those performed in other countries using the SDQ for assessment of children born preterm,18,19 both performed in children born preterm before 28 weeks’ gestation or with birth weights of less than 1000g. Elgen19 reported statistically significant differences in all subscales between children born preterm and children born at term, although the difference in the prosocial scale was very small. Fevang18 reported that at age 11, children born preterm were at higher risk of having poorer scores in the hyperactivity/inattention, emotional and peer relationship scales. This latter study only considered 4 subscales, omitting the one on prosocial behaviour. Both studies included only children born very preterm and immature, a population in which the differences are more marked. Nevertheless, our findings were in agreement to those of both studies, as we did find a higher prevalence of emotional disorders and greater difficulties relating to peers compared to children born to term, although the differences in prosocial behaviour were less clear.
Once these disorders are detected, the child must be referred for evaluation by a child and adolescent psychiatrist to establish an accurate diagnosis and appropriate treatment. In many cases, the management of these patients requires a combination of pharmacotherapy and cognitive-behavioural interventions.25
We believe that the use of the SDQ offers some advantages over other instruments, and thus could be easily implemented in follow-up clinics. For example, a study by Goodman et al. suggested that the SDQ could be similar or even better for the detection of inattention and hyperactivity than the Child Behaviour Checklist, which comprises 118 items and requires an interview.26
When it comes to risk factors, the poorer prognosis associated with intraventricular haemorrhage mainly involved grades III and IV. Haemorrhages of grades I or II have also not been identified as a risk factor for these disorders in other studies.27 We also found that low weight for gestational age was associated with a less favourable score in the questionnaire. Other studies that used the SDQ have also found worse scores in the hyperactivity, emotion and conduct scales in children born small for gestational age.28,29 One of the possible explanations for the poorer outcomes in these children are the abnormalities in cerebral development previously described in the literature, such as a reduced volume of cortical grey matter. Patients of the male sex, as previously reported,30 had less favourable scores in the questionnaire. A low score in the Bayley mental developmental index at 2 years of corrected age is a warning sign of an increased risk of future behaviour and socialization problems, although even in the absence of this delay, children born preterm are more likely to develop psychosocial problems.31 Another well-known risk factor for psychosocial problems is a low family socioeconomic status.32
Some studies have been designed to assess the validity of the SDQ for diagnosis of ADHD and have found an adequate sensitivity, especially for the combined type, with a lower sensitivity for the detection of predominantly inattentive or hyperactive ADHD.33 Other authors have also described the correlation of other scales of the questionnaire, other than the hyperactivity scale, with the symptoms of ADHD, such as the behavioural features associated with hyperactivity or the emotional features associated with inattention.34 In our study, we found that patients with an ADHD diagnosis had scores in the hyperactivity scale and the full questionnaire that were significantly different. In addition, based on the results we obtained drawing the ROC curves, there is a significant difference in the accuracy of diagnosis of ADHD between using the score of the hyperactivity scale and the total score, with the latter being more accurate.
When it comes to establishing a cut-off point in the hyperactivity scale and the total SDQ scores to differentiate normalcy, it is important to remember that we are proposing the use of the questionnaire for screening of ADHD, and thus priority should be placed on obtaining high sensitivity values. Thus, based on the results that we present in Table 5, it seems reasonable to suggest the use of a score in the hyperactivity scale of 6 or greater, a total SDQ score of 13 or greater, or a combination of a score of 5 or greater in the hyperactivity scale with a total score of 12 or more points, all of them options for which the sensitivity is of approximately 80% with an acceptable specificity and a positive likelihood ratio of approximately 3. The earliest studies in the literature that used the SDQ in the general population proposed a threshold to define pathology of 16 or greater for the total score and of 7 or greater for the hyperactivity scale but more recent studies, as was the case of our own, have found that lowering these thresholds could achieve significant increases in sensitivity, thus improving the usefulness of this tool for screening purposes.34
The drawback that we found in our study applying the proposed cut-off points is that screening would lead to the referral to psychiatric services of 35–40% of the children in followup. Different cut-off points could be used in each hospital based on the availability of child psychiatry services, thus balancing the benefits of psychiatric assessment with the existing resources. We expect that in upcoming years, thanks to the recent recognition of child psychiatry as a separate specialty in Spain, there will be an increased in the available resources, so that many children born with VLBW/VPT will be able to benefit from specialised care in this field. It is also important to take into account that children that score above the cut-off points that do not ultimately receive an ADHD diagnosis would probably also benefit from a proper psychiatric assessment, as they may have other types of problems (in our study, they mainly were excessive shyness or a dependent personality) requiring specialised care and treatment.
Some of the limitations of our study are the use of a general population as the control group (potential selection bias) and that we did not evaluate the usefulness of the SDQ based on the type of ADHD: inattentive, hyperactive or combined.35 On the other hand, the losses to follow-up by age 6 years are high, which poses another risk of bias in the sample under study.
To conclude, we ought to remark that compared to the reference population, children born with VLBW/VPT scored higher in the SDQ and therefore had more psychosocial problems, especially when it came to emotions and relationships with peers. Furthermore, the questionnaire could be used for screening of ADHD in this population, either using the hyperactivity scale or the total SDQ score. The fact is that we still have much to learn about emotional and behavioural problems in children born with VLBW/VPT, and at present these children are probably not receiving the specialised care that they need.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Bachiller-Carnicero L, García-Soria CE, Piris-Borregas S, Sierra-García P, Torres-Valdivieso MJ, Pallás-Alonso CR. Uso del Strength and Difficulties Questionnaire en prematuros para su evaluación psicosocial y cribado del trastorno por déficit de atención e hiperactividad. An Pediatr (Barc). 2019;91:142–150.