The birth of a preterm child has a high family emotional cost. The aim of this study is to assess the quality of life of parents of children aged 5–7 years born prematurely (<1500g).
Participants and methodsThis is a cross-sectional study of a sample of parents of preterm infants admitted to a third level hospital in Spain between 2009 and 2011. Their infants weighed less than 1500g at birth, and were 5–7 years old at the moment of the study. Parents completed the Parental Stress Scale, Family Apgar, Zarit modified scale, and Graffar-Méndez Castellano method (1994). A total of 94 cases were analysed (40 girls and 54 boys).
ResultsAll data passed normality assumptions. Results showed no gender, weight or gestational age differences in our sample on the Zarit modified scale, Parental Stress Scale, or by the Graffar method. Differences between boys and girls were found in the Family Apgar test. Also, the Graffar method and degree of familiar malfunction showed significant results. The parents of preterm children with developmental problems at the time of the study showed significant differences with respect to parents of children without these problems in the Family Apgar test and the Zarit modified scale.
ConclusionsThe possible impact of the birth of a preterm child with less than 1500g of weight is not appreciated between 5 and 7 years of age, except for the differences found in the perception of family functionality and caregiver overload among parents of children with and without developmental alterations.
El nacimiento de un hijo prematuro conlleva un alto coste emocional familiar. El objetivo es valorar la calidad de vida de los progenitores de una cohorte de niños prematuros nacidos con peso menor de 1.500g, cuando estos contaban entre los 5 y los 7 años de edad.
Pacientes y métodosEstudio transversal de encuestas personales a progenitores de niños de entre 5 y 7 años de edad que estuvieron ingresados en un hospital terciario de España entre 2009 y 2011, siendo neonatos, por un peso al nacimiento menor de 1.500g. Se aplicó la escala del estrés parental, test de Apgar familiar, escala de sobrecarga del cuidador de Zarit y cuestionario Graffar. Se analizan 94 casos (40 niñas y 54 niños).
ResultadosTodas las escalas muestran puntuaciones de normalidad. Con la escala de Zarit, del estrés parental y el cuestionario Graffar-Méndez Castellano, los resultados no reflejan diferencias por sexo, peso ni edad gestacional. Encontramos diferencias estadísticamente significativas con el test de Apgar familiar por sexo y entre la puntuación de Graffar y el grado de disfunción familiar. En el momento del estudio, los padres de niños con problemas en el desarrollo presentaban diferencias estadísticamente significativas con los padres de niños sin alteraciones, reflejadas en el test de Apgar familiar y en la escala de Zarit.
ConclusiónLa posible repercusión del nacimiento de un hijo con un peso menor de 1.500g no se aprecia con los test estudiados cuando el niño tiene entre los 5 y 7 años de edad, salvo por las diferencias que se observan en la percepción de la funcionalidad familiar y en la sobrecarga de cuidadores entre los padres de niños con alteraciones en el desarrollo y sin ellas.
The birth of a child at term involves changes in the lives of families and requires a brief period of adjustment for them.1 In contrast, the birth of a very preterm baby can cause a crisis in the family unit. Parents are faced with multiple uncertainties as regards the development of the child at a high emotional cost, with disturbances in several aspects of current and future everyday life.2
The hospitalisation of a newborn is invariably traumatic for a family,3 more so in case of a preterm newborn. The unease endures past discharge, as uncertainties remain regarding future development. Children born preterm benefit from a multidisciplinary follow-up throughout childhood, including early intervention services, and this can have an impact on family dynamics. The presence in the household of a member that requires special care is stressful and may undermine the stability of the family unit, affecting its other members, especially the main caregiver, who bears a heavier emotional burden with deleterious repercussions on his or her physical and psychological well-being.1
There are multiple studies on the subject of preterm birth and its short-, medium- and long-term consequences in children, but few studies have analysed family functioning and stress in the families of children born preterm.3,4
The aim of our study was to evaluate the quality of life of parents in a cohort of infants born with very low birth weight (birth weight <1500g), assessing parental stress levels, the overburdening of caregivers and family functioning, also analysing the potential influence of socioeconomic factors.
Patients and methodsThe study presented here was conducted in the framework of a larger project known as “Influences of somatometric parameters in the neuropsychological outcomes of infants born with weights of less than 1500g”. It was carried out in a city in northern Spain between February 2016 and May 2017. The interviews were held at a referral university hospital whose catchment area encompasses the entire autonomous region of Asturias.
It was a cross-sectional descriptive study with collection of data by means of personal interviews with the parents of children born between 2009 and 2011 with birth weights of less than 1500g that were hospitalised as newborns in our hospital. We conducted the interviews when the children were aged 5–7 years during the checkups performed in the context of the aforementioned larger project.
The inclusion criteria were parents of a child born preterm with a birthweight of less than 1500g between 2009 and 2011. We excluded the families of newborns that died.
We contacted the parents of children that met the criteria (n=147) through a letter that invited them to participate. The appointment for the assessment was scheduled by telephone. We informed all participants of the objectives and protocol of the study. Each family received a signed statement where we committed to safeguard the confidentiality of the data.
Participating parents signed an informed consent form by which they allowed us to measure some aspects of quality of life in terms of the stress in the household, the overburdening of caregivers and the socioeconomic level of the family. We then proceeded to administer the following tests, which had been previously validated:
- -
Parenting stress scale5: scale used to measure parental levels of stress caused by parenting. There are 2 versions, a full one and an abridged one. In our study, we used the abridged version adapted to the Spanish population, comprising 12 items.6 Some of the items were positive items (2, 5, 6, 7, 8, 9 and 10) and were scored on a Likert scale from 1 (completely disagree) to 5 (completely agree) and others were negative items (1, 3, 4, 11 and 12) scored in reverse: the answer “completely disagree” was given 5 points and the answer “completely agree” 1 point. The total score ranged between 5 and 60 points, with higher scores indicating greater stress levels in families.
- -
Family Apgar score7: it reflects how family members perceive the overall level of functioning of the family unit. It assesses 5 basic parameters of family function that are considered essential (adaptation, partnership, growth, affection and resolve) by means of Likert scales with values ranging from 0 (never) to 4 (almost always). The total score ranges between 0 and 20 points; a total score of 17–20 points indicates normal family functioning, a score of 16–13 points mild dysfunction, a score of 10–12 moderate dysfunction, and a score below 10 points severe dysfunction.
- -
Caregiver burden interview developed by Zarit,8 Spanish validated adaptation9: assesses subjective feelings of burden in caregivers of elderly patients with senile dementia. It has been used previously in other studies of children born preterm,10 adapting it for the purpose by eliminating the items that do not apply to the population of interest, with final selecting 11 out of the 22 original items by expert consensus. Items are scored on a Likert scale with values ranging from 0 (never) and 4 (nearly always). There are three categories of burdening based on the score (no overburdening [0–12 points], mild overburdening [13–17 points] and severe overburdening [18–44 points]).
- -
Graffar scale11: measures socioeconomic status based on 5 variables: occupation of the head of household (defined as the parent with the highest-level occupation), maternal educational attainment, household income, living conditions in the home and state of the neighbourhood of residence. The results are divided into 5 classes based on the total score: class I, upper (score, 5–9); class II, upper-middle (score, 10–13); class III, middle (score, 14–17); class IV, lower-middle (score, 18–21); class V, lower (score, 22–25).
We analysed the collected data with a statistics software application. In the descriptive analysis, we summarised quantitative variables using the mean and the corresponding 95% confidence intervals and the range, and qualitative variables by means of frequencies. Since we obtained the data through the use of scales, we chose to use nonparametric tests to make comparisons, comparing quantitative variables using the median and interquartile range by means of the Mann–Whitney U and Kruskal–Wallis tests and qualitative variables by means of the chi square test. We used the Spearman correlation coefficient to assess the correlation between variables. For all tests, we defined statistical significance based on an alpha level of 5%.
We conducted the study in adherence with the principles of good clinical practice and current laws after obtaining the approval of the Research Ethics Committee of the Autonomous Region of Asturias.
ResultsOf the 181 infants born with weights of less than 1500g admitted to our hospital in the 3 years under study, 34 died before discharge. Of the other 147, the parents of 94 (63.9%) agreed to participate in this study, while the parents of 53 did not (we were unable to contact the parents of 26, the parents of 7 refused to participate, the parents of 16 initially agreed but then did not engage further, 2 children were in the Child Welfare System of the Principality of Asturias and we chose not to include them, 1 child had leukaemia and the mother of 1 other child came to the interview but then declined to fill out the instruments for the assessment of quality of life). Five percent of children had parents that reported being separated at the time of the study, and 27.5% of the children were only children.
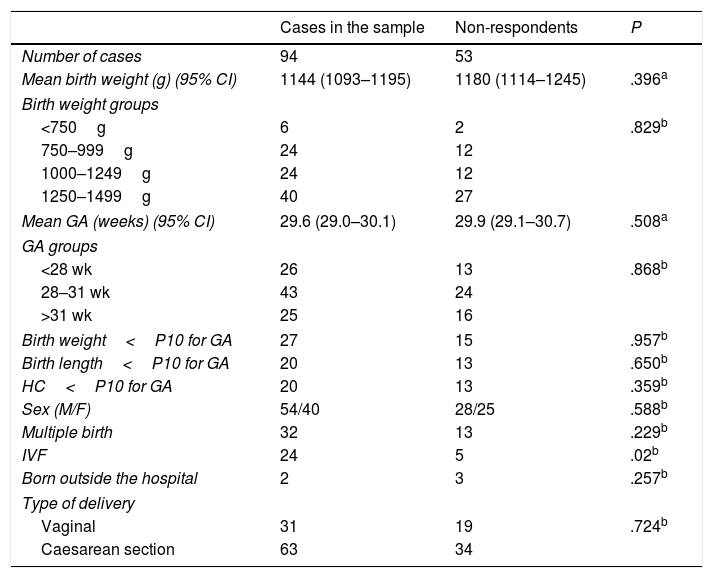
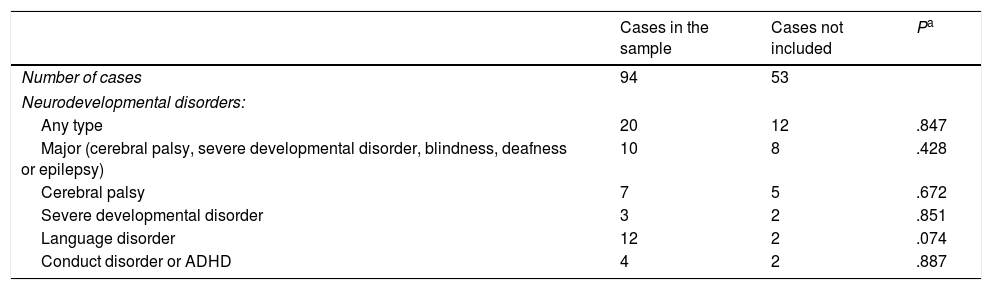
When we compared the children that were surveyed and those whose parents declined participation (non-respondents), we did not find statistically significant differences in the neonatal variables under study (birth weight, gestational age, sex, type of delivery, twin pregnancy, Apgar score at birth and diseases diagnosed at discharge) except in the history of in vitro fertilisation. We also found no differences between these groups in the frequency of specific developmental disorders. Tables 1 and 2 show the most important characteristics of the cases under study and of non-respondents. Table 3 shows the overall data obtained with the different instruments by gestational age group.
Comparison of birth weight, gestational age, sex of child and type of delivery in cases included in the study versus parents of survivors that did not participate (non-respondents).
| Cases in the sample | Non-respondents | P | |
|---|---|---|---|
| Number of cases | 94 | 53 | |
| Mean birth weight (g) (95% CI) | 1144 (1093–1195) | 1180 (1114–1245) | .396a |
| Birth weight groups | |||
| <750g | 6 | 2 | .829b |
| 750–999g | 24 | 12 | |
| 1000–1249g | 24 | 12 | |
| 1250–1499g | 40 | 27 | |
| Mean GA (weeks) (95% CI) | 29.6 (29.0–30.1) | 29.9 (29.1–30.7) | .508a |
| GA groups | |||
| <28 wk | 26 | 13 | .868b |
| 28–31 wk | 43 | 24 | |
| >31 wk | 25 | 16 | |
| Birth weight<P10 for GA | 27 | 15 | .957b |
| Birth length<P10 for GA | 20 | 13 | .650b |
| HC<P10 for GA | 20 | 13 | .359b |
| Sex (M/F) | 54/40 | 28/25 | .588b |
| Multiple birth | 32 | 13 | .229b |
| IVF | 24 | 5 | .02b |
| Born outside the hospital | 2 | 3 | .257b |
| Type of delivery | |||
| Vaginal | 31 | 19 | .724b |
| Caesarean section | 63 | 34 | |
CI, confidence interval; F, female; GA, gestational age; HC, head circumference; IVF, in vitro fertilisation; M, male; P10, 10th percentile.
Comparison of developmental disorders between cases included in the study and survivors not included in the study (non-respondents).
| Cases in the sample | Cases not included | Pa | |
|---|---|---|---|
| Number of cases | 94 | 53 | |
| Neurodevelopmental disorders: | |||
| Any type | 20 | 12 | .847 |
| Major (cerebral palsy, severe developmental disorder, blindness, deafness or epilepsy) | 10 | 8 | .428 |
| Cerebral palsy | 7 | 5 | .672 |
| Severe developmental disorder | 3 | 2 | .851 |
| Language disorder | 12 | 2 | .074 |
| Conduct disorder or ADHD | 4 | 2 | .887 |
ADHD, attention-deficit hyperactivity disorder.
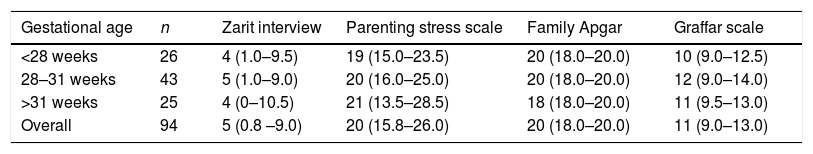
Comparison of the scores in the different tests performed (Zarit caregiver burden interview, parenting stress scale, family Apgar score and Graffar scale) by gestational age group.
| Gestational age | n | Zarit interview | Parenting stress scale | Family Apgar | Graffar scale |
|---|---|---|---|---|---|
| <28 weeks | 26 | 4 (1.0–9.5) | 19 (15.0–23.5) | 20 (18.0–20.0) | 10 (9.0–12.5) |
| 28–31 weeks | 43 | 5 (1.0–9.0) | 20 (16.0–25.0) | 20 (18.0–20.0) | 12 (9.0–14.0) |
| >31 weeks | 25 | 4 (0–10.5) | 21 (13.5–28.5) | 18 (18.0–20.0) | 11 (9.5–13.0) |
| Overall | 94 | 5 (0.8 –9.0) | 20 (15.8–26.0) | 20 (18.0–20.0) | 11 (9.0–13.0) |
No statistically significant differences by gestational age group (Kruskal–Wallis test). Comparisons were made using the median (with the interquartile range).
Of the 94 children included in the study, 20 had received a diagnosis of a developmental problem by the time of the study (21.2%): language disorder in 12, childhood cerebral palsy in 7, behavioural problems in 4, learning disorders in 4, attention-deficit hyperactivity disorder in 4 and autism spectrum disorder in 3.
Parental stress variableThe median score in the parenting stress scale was 20 points (interquartile range, 15.75–26). We did not find differences based on sex (female, 19 points; male, 21.5 points; P=.147), birth weight (BW) group (BW≤1000g, 18 points; BW>1000g, 20.5 points; P=.09), or gestational age group (P=.532). We also did not find a significant linear correlation between parental stress and BW (P=.084), or parental stress and gestational age (P=.173).
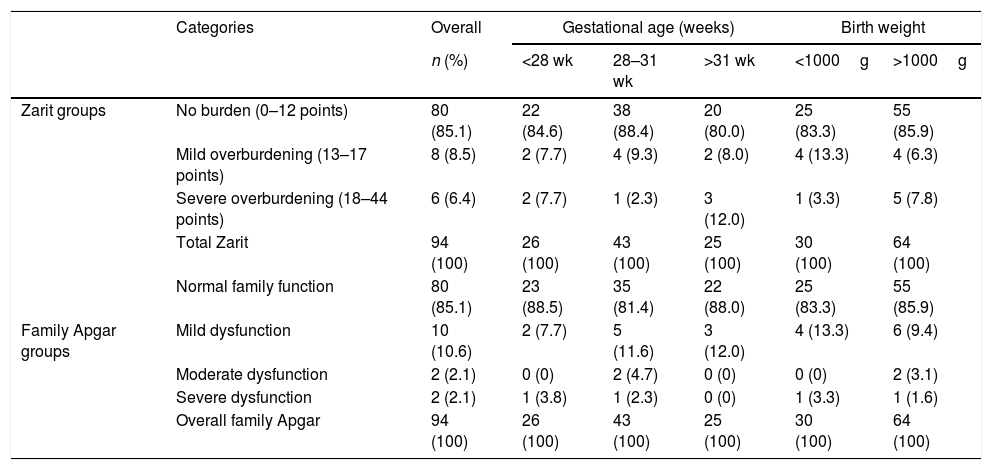
Overburdening of caregivers variableThe median score obtained with the Zarit caregiver burden interview was of 5 points (interquartile range, 0.75–9). When we distributed the values into the corresponding categories, we found no burden (0–12 points) in 80 cases (85.1%), mild overburdening (13–17 points) in 8 cases (8.5%) and severe overburdening (18–44 points) in 6 cases (6.4%).
We did not find differences in feelings of overburdening based on the sex of the child (female, 5.5 points versus male, 4 points; P=.615), nor an association between these two qualitative variables (P=.844).
When we compared overburdening based on gestational age and birth weight, we did not find statistically significant differences between groups (Table 4). We also found no linear correlation between gestational age and the overburdening variable (P=.946) or between birth weight and overburdening (P=.549).
Caregiver overburdening (Zarit caregiver burden interview) and family functioning (family Apgar score) by gestational age and birth weight.
| Categories | Overall | Gestational age (weeks) | Birth weight | ||||
|---|---|---|---|---|---|---|---|
| n (%) | <28 wk | 28–31 wk | >31 wk | <1000g | >1000g | ||
| Zarit groups | No burden (0–12 points) | 80 (85.1) | 22 (84.6) | 38 (88.4) | 20 (80.0) | 25 (83.3) | 55 (85.9) |
| Mild overburdening (13–17 points) | 8 (8.5) | 2 (7.7) | 4 (9.3) | 2 (8.0) | 4 (13.3) | 4 (6.3) | |
| Severe overburdening (18–44 points) | 6 (6.4) | 2 (7.7) | 1 (2.3) | 3 (12.0) | 1 (3.3) | 5 (7.8) | |
| Total Zarit | 94 (100) | 26 (100) | 43 (100) | 25 (100) | 30 (100) | 64 (100) | |
| Normal family function | 80 (85.1) | 23 (88.5) | 35 (81.4) | 22 (88.0) | 25 (83.3) | 55 (85.9) | |
| Family Apgar groups | Mild dysfunction | 10 (10.6) | 2 (7.7) | 5 (11.6) | 3 (12.0) | 4 (13.3) | 6 (9.4) |
| Moderate dysfunction | 2 (2.1) | 0 (0) | 2 (4.7) | 0 (0) | 0 (0) | 2 (3.1) | |
| Severe dysfunction | 2 (2.1) | 1 (3.8) | 1 (2.3) | 0 (0) | 1 (3.3) | 1 (1.6) | |
| Overall family Apgar | 94 (100) | 26 (100) | 43 (100) | 25 (100) | 30 (100) | 64 (100) | |
The differences by gestational age and birth weight groups were not statistically significant (chi square).
Data given as n (%).
The median family Apgar score was 20 points (interquartile range, 18–20). We found no statistically significant differences in the score between BW groups (BW≤1000g, 20 points; BW>1000g, 18 points; P=.218) or between gestational age groups (P=.252) (Table 4).
We found significant differences based on the sex of the child (female, 18 points vs male, 20 points; P=.032). However, we did not find a statistically significant association between the sex of the child, on one hand, and the different categories of the Apgar score categories (P=.216), birth weight (P=.669) or gestational age (P=.718), on the other.
Socioeconomic level variableThe median score in the Graffar scale was 11 points (interquartile range, 9–13). We found no differences based on sex (11 points in both groups; P=.610), birth weight category (10 vs 11 points; P=.530), or gestational age group (P=.09).
Relationship between the different variables under studyWe did not find an association between socioeconomic status group and the overburdening categories (P=.643). We found no differences in the parenting stress scale score between socioeconomic status categories (P=.333).
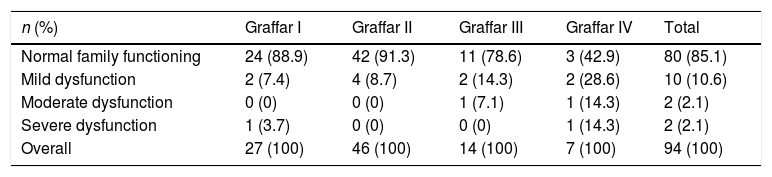
We did find an association between socioeconomic status and the categories of family functioning (P=.025): the highest scores in the socioeconomic level instrument (corresponding to the lower class) occurred in the most dysfunctional families (Table 5).
Association between socioeconomic score (Graffar scale) and family functioning (family Apgar score) categories.
| n (%) | Graffar I | Graffar II | Graffar III | Graffar IV | Total |
|---|---|---|---|---|---|
| Normal family functioning | 24 (88.9) | 42 (91.3) | 11 (78.6) | 3 (42.9) | 80 (85.1) |
| Mild dysfunction | 2 (7.4) | 4 (8.7) | 2 (14.3) | 2 (28.6) | 10 (10.6) |
| Moderate dysfunction | 0 (0) | 0 (0) | 1 (7.1) | 1 (14.3) | 2 (2.1) |
| Severe dysfunction | 1 (3.7) | 0 (0) | 0 (0) | 1 (14.3) | 2 (2.1) |
| Overall | 27 (100) | 46 (100) | 14 (100) | 7 (100) | 94 (100) |
Chi square, P=.025.
Relationship between analysed scales and developmental outcomes in children
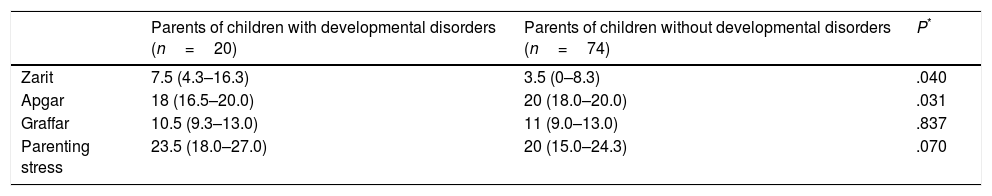
Table 6 shows the comparison of the group of parents with children with developmental disorders at the time of the interview and the group of parents of children with normal development. We found statistically significant differences between the groups in the variables of caregiver overburdening and family functioning.
Comparison of the different variables under study (Zarit caregiver burdening interview, parenting stress scale, family Apgar score and Graffar scale) based on the sequelae present in children at the time of the survey.
| Parents of children with developmental disorders (n=20) | Parents of children without developmental disorders (n=74) | P* | |
|---|---|---|---|
| Zarit | 7.5 (4.3–16.3) | 3.5 (0–8.3) | .040 |
| Apgar | 18 (16.5–20.0) | 20 (18.0–20.0) | .031 |
| Graffar | 10.5 (9.3–13.0) | 11 (9.0–13.0) | .837 |
| Parenting stress | 23.5 (18.0–27.0) | 20 (15.0–24.3) | .070 |
In families with separated parents, 80% of children born preterm exhibited developmental disorders, and these families were the most dysfunctional.
DiscussionThe preterm birth of a child is a traumatic event for families. Many studies have described how parents experience high levels of stress and feelings of powerlessness in the face of this event.1,12,13
However, our findings suggest that this stress resolves over time, since by the time children had turned 5–7 years the parenting stress scores were normal. None of these scores were out of the normal range, which suggests that the passage of time allowed the resolution of the initial problems that emerged at the time of the birth.
The assessment of the overburdening of caregivers (Zarit interview) did not seem to show considerable overburdening in the sample under study, contrary to the evidence found by other authors.14 We also did not find significant parental stress levels with the use of the scale, an aspect that has been debated in previous studies.3,15
When we assessed family functioning by means of the family Apgar score, we found that all families but 3 had a normal score, contrary to previous published evidence that reflected that greater parental stress had a negative impact on family functioning.3 That said, if families do not exhibit great levels of stress, a normal level of functioning would be expected.
When we analysed the socioeconomic status with the Graffar scale, we did not find significant associations in the comparison of neonatal and socioeconomic factors to the levels of stress and burdening. On this subject, some authors have suggested that the socioeconomic and educational level of parents could be a mediating factor between preterm birth and parental stress.3 Since most of the families in our study were middle class, we would not have expected to find evidence of this association. What we did find, however, is that the most dysfunctional families corresponded to the lowest socioeconomic levels.
When it came to the scores obtained using different instruments, we also did not find statistically significant differences based on gestational age, birth weight or sex of the child. We only found a significant difference, although of little clinical relevance, in the family Apgar score between the parents of boys and the parents of girls, which we consider irrelevant and without explanation, as the size was small (difference of 1.1 points) and the difference disappeared when we performed a quantitative analysis of different groups.
The most salient findings involved the comparison of the responses of parents with children that had received diagnoses of developmental disorders compared to children that had no such diagnoses, as we found differences in family functioning and caregiver overburdening, which were statistically significant but may not be clinically relevant.
It is important to take into account that one of the main limitations of our study was the lack of a control group. Furthermore, since participation was voluntary and depended on the availability of families, we may have missed cases with other factors involved in parenting stress and caregiver overburdening. There may also be a response bias in socioeconomic aspects differentiating respondents from non-respondents, although this is not something we were able to assess, as we had no means to know the current situation of parents that did not participate. Another limitation was the sample size, which determined the type of analysis that could be done. A larger sample would have allowed us to perform a multivariate analysis, analysing neonatal characteristics and other possible effect-modifying variables.
In future studies, it would be interesting to perform a longitudinal follow-up of stress levels in the family at different time points since birth with a prospective design, as the uncertainty revolving around the future development of the child, which may affect the responses of parents, is inversely proportional to age. Another interesting subject for analysis would be the assessment of attachment and stress outcomes, as has been done in previous studies.16
In short, based on the findings of our study, it seems that as time passes, and specifically by the time children reach an age between 5 and 7 years, the experience of having a child that was born preterm with a birth weight of less than 1500g no longer has an impact on family dynamics However, there are 2 particular aspects deserving attention: the presence of developmental disorders in the child and the socioeconomic level of the family. In the first case, there are statistically significant differences in family functioning and overburdening of caregivers. In contrast, the socioeconomic level of the family has an impact on family functioning, with dysfunctional family patterns corresponding to families with lower socioeconomic status.
In light of these findings, it appears that families with low socioeconomic status require more support after the child is discharged to prevent overburdening of the caregiver and potential family dysfunction.
FundingThis project was financially possible thanks to the Grants for Clinical and Epidemiological Research in Paediatrics given by the Fundación Ernesto Sánchez Villares in year 2016, of which Leticia Alcántara-Canabal was a recipient (Project 05/2016); a grant from the Secretariat of Research, Development and Innovation of the Government of Spain (PSI2017-83893-R) and the Severo Ochoa predoctoral grant programme, which gave a grant to Cristina Fernández-Baizán through the Council of Culture and Sports of the Principality of Asturias, Spain (PA-17-PF-BP16090).
Conflicts of interestThe authors have no conflicts of interest to declare.
This study was possible thanks to the efforts of the entire team and especially to the disinterested participation of the families of children born preterm.
Please cite this article as: Alcántara-Canabal L, Martínez-Pérez L, Gutiérrez-Alonso S, Fernández-Baizán C, Méndez M. Calidad de vida de los padres de escolares nacidos prematuros con peso menor de 1.500 gramos. An Pediatr (Barc). 2019;91:151–157.
Previous presentation: This study was presented as a poster with a short oral communication and entered the competition for awards at the XXVI Congreso de Neonatología y Medicina Perinatal/VI Congreso de Enfermería Neonatal, September 27–29, 2017, Zaragoza, Spain.