Acute bronchiolitis (AB) is a viral infection that causes annual outbreaks, in the case of Spain, with the epidemic season starting approximately in October of one year and ending in March or April the following year.1 The nonpharmacological interventions implemented on the Spanish population as a result of the coronavirus 2019 (COVID-19) pandemic were responsible, at least in part, for a decrease in the incidence of childhood infectious diseases2, including AB.3,4 In May 9, 2021, the government of Spain declared the end of the state of alarm, which was followed by a progressive de-escalation of the preventive measures implemented until that time. This could have led to the re-emergence of different viral agents involved in the pathogenesis of AB, as described in other geographical areas.5
In an extension of a previous study3 and in the framework of the same research project, the Spanish Collaborative Study for the Care of Infants Hospitalised with Acute Bronchiolitis (known by the acronym of its Spanish name, ECEALHBA), we conducted a substudy with the aim of determining whether there was a resurgence of AB cases in the form of an outbreak after the state of alarm was lifted, and to compare the outbreaks in different epidemic seasons, in addition to the frequency of hospitalization, grouped in different periods based on the pandemic.
We collected data on the cases of AB that required admission prospectively from April 16 to August 31, 2021 on the same study variables and applying the same inclusion criteria.3 Thus, we analysed all cases of AB over 6 epidemic seasons, 2015–2016 to 2020–2021. We established 3 study periods based on 2 key dates: (1) Prepandemic period (P1), from September 1, 2015 to March 15, 2020 (declaration of state of alarm); (2) COVID-19 pandemic during state of alarm (P2), from March 15, 2020 to May 9, 2021 (end of state of alarm), and (3) COVID-19 pandemic after lifting of state of alarm (P3), from May 9, 2021 to the end of data collection.
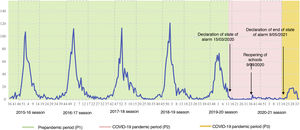
A total of 4809 infants with a median age of 2.4 months (interquartile range, 1.4–4.5) and a median length of stay (LOS) of 4.4 days (standard deviation, 2.7), of who 384 (8.0%) required admission to the intensive care unit (ICU). The epidemic seasons before the pandemic took place in the typical time of year, the winter months, while in the 2020–2021 season, during the pandemic, it took place in the summer months and was shorter and less severe compared to preceding seasons (Table 1A and Fig. 1).
Weeks that the epidemic season started, ended and peaked, and its duration. Total admissions in the 6 epidemic seasons under study.
| Season/characteristics | Start of season | End of season | Season peak | Duration of season | Admissions per season |
|---|---|---|---|---|---|
| 2015–16 | Week 47 (5) | Week 15 (4) | Week 1 (107) | 21 weeks (793) | 891 |
| 2016–17 | Week 45 (10) | Week 13 (7) | Week 1 (112) | 21 weeks (889) | 1013 |
| 2017–18 | Week 43 (5) | Week 18 (5) | Week 52 (82) | 28 weeks (896) | 928 |
| 2018–19 | Week 44 (4) | Week 24 (3) | Week 1 (109) | 33 weeks (960) | 995 |
| 2019–20 | Week 47 (10) | Week 12 (4) | Week 1 (105) | 18 weeks (656) | 767 |
| 2020–21 | Week 22 (2) | Week 34 (0) | Weeks 28 and 29 (18) | 13 weeks (153) | 215 |
| Average epidemic season profilea | Week 45 (6.8) | Week 16 (4.6) | Week 1 (103) | 24 weeks (838.8) | 961.8 |
The numbers in parentheses correspond to the cases requiring hospital admission in the corresponding week or weeks.
Start of season: week from which the increase in hospital admissions became noticeable and progressive until reaching the epidemic peak.
End of season: the week after the peak at which the number of admissions was the same or fewer than the number at the week identified as the start of the season.
Graphic representation of the total admissions due to bronchiolitis in the 16 participating hospitals during the 6 epidemic seasons under study.
The rectangles with a dashed border indicate the bounds of the epidemic seasons, from week 45 (first of November) to week 16 (third of April). These are average bounds obtained from our data. For further information, see Table 1A.
The most common profile of infants admitted to hospital during P2 compared to P1 and P3 was male sex, older age, negative for respiratory syncytial virus (RSV), with a shorter LOS and not requiring admission to the ICU. However, when we compared infants admitted during P3 (the period with the summer outbreak) with those admitted in P1 (period with typical winter outbreaks), these differences were not significant (Table 1B).
Comparison of clinical and demographic characteristics of infants admitted with a diagnosis of acute bronchiolitis in the 3 periods under study.
| Variable | Prepandemic (P1) (n = 4580) | Pandemic (P2) (n = 70) | Pandemic (P3) (n = 159) | P |
|---|---|---|---|---|
| Sex, male (n = 2790) | 2664 (58.2%) | 50 (71.4%) | 76 (47.8%) | .002 |
| Nationality, Spanish (n = 4047) | 3850 (84.7%) | 58 (82.9%) | 139 (87.4%) | .565 |
| Age group | ||||
| Newborn (n = 562) | 535 (11.7%) | 7 (10.0%) | 20 (12.6%) | |
| Infant ≤ 3 months (n = 2283) | 2194 (47.9%) | 20 (28.6%) | 69 (43.4%) | .007 |
| Infant > 3 month (n = 1964) | 1851 (40.4%) | 43 (61.4%) | 77 (44.0%) | |
| LOS group | ||||
| ≤3 days (n = 2122) | 2008 (43.8%) | 43 (61.4%) | 71 (44.7%) | .014 |
| >4 days (n = 2687) | 2572 (56.2%) | 27 (38.6%) | 88 (55.3%) | |
| Aetiological investigation, yes (n = 4609) | 4382 (95.7%) | 68 (97.1%) | 159 (100%) | .001 |
| RSV | ||||
| Not tested (n = 202) | 198 (4.3%) | 3 (4.3%) | 1 (0.60%) | |
| Positive (n = 2977) | 2841 (62%) | 9 (12.9%) | 127 (79.9%) | <.001 |
| Negative (n = 1630) | 1541 (33.6%) | 58 (82.8%) | 31 (19.5%) | |
| Admission to ICU, admitted (n = 384) | 366 (8.0%) | 0 (0%) | 18 (11.3%) | .001 |
ICU, intensive care unit; LOS, length of stay; RSV, respiratory syncytial virus.
The numbers in parentheses correspond to the percentage of the category over the total in each group or period into which the admissions due to bronchiolitis were classified.
Our data evince a resurgence of AB cases in the population of central and eastern Spain, unexpectedly, in the summer months, in the 2020-2021 epidemic season, 3 weeks after the lifting of the state of alarm. A similar phenomenon had also been described in geographical areas in the southern hemisphere, with a resurgence of respiratory infections by RSV in November and December 2020, which correspond to the summer in these areas, after the de-escalation of measures implemented to contain the pandemic.5 This resurgence has also been described in other regions of the northern hemisphere.6
In this study, the LOS and the proportion of cases with detection of RSV that required admission to the ICU were greater during the pandemic compared to previous seasons. In our study, we only found a slight increase in the proportion of admission to the ICU in P3 (11.3%) compared to P1 (8%), with no overall differences in LOS (Table 1B).
These findings evince the importance of social distancing, hand hygiene and mask use, among other measures, for effective prevention of the spread of the viruses involved in the annual outbreaks of AB.
At the time of this writing, in November 2021, the members of the ECEALHBA research project have already been noticing, in their recent daily clinical practice, what appears to be an earlier start of the 2021–2022 epidemic season in addition to an increase in severity, virulence and younger age of affected patients. Confirming these perceived trends and attempting to identify the underlying causes of these particularities are among the future research objectives of the ECEALHBA project.
Rius-Peris JM; Maraña Pérez AI; Cueto Calvo E. Hospital Virgen de la Luz. Cuenca, Spain.
Marcilla Vázquez C; Pareja León M. Hospital General de Albacete. Albacete, Spain.
Molini Menchón N; Lucas-García J. Hospital General de Castellón. Castellon, Spain.
Felipe Almira E; Sequí-Canet JM. Hospital Francisco Borja. Gandía, Valencia, Spain.
Silvestre Beneyto R; Olmos García JM; Escrivá Tomás P. Hospital Virgen de los Lirios. Alcoy, Alicante, Spain.
Pantoja-Martínez J; Povo Martín S. Hospital de La Plana. Villarreal, Castellon, Spain.
Caballero Mora FJ. Hospital Santa Bárbara. Puertollano, Ciudad Real, Spain.
García Maset L; Coret Sinisterra A. Hospital de Sagunto. Sagunto, Valencia, Spain.
Castillo Ochando F; Garrido MJ. Hospital de Villarrobledo. Villarrobledo, Albacete, Spain.
Edo Tena A; Rabasco Álvarez L. Hospital de Vinarós. Vinarós, Castellon, Spain.
Moya Díaz-Pintado MT. Hospital Virgen de Altagracia. Manzanares, Ciudad Real, Spain.
Cardete Pascual I; García Candel S; Amat Madramany A. Hospital de La Ribera. Alzira, Valencia, Spain.
Moreno López M. Hospital de Tomelloso. Tomelloso, Ciudad Real, Spain.
Pons Morales S. Hospital Dr. Peset. Valencia, Spain.
Vicent Castelló MC; Sánchez Sánchez A; Rivera Figueiras AM; Herrero Galiana A; González de Dios J. Hospital General de Alicante. Alicante, Spain.
García-Peris M; Domingo Pla A; Devesa Jover P. Hospital Lluís Alcanyís. Xátiva. Valencia, Spain.
Appendix 1 details the members of the ECEALHBA project research group.
Please cite this article as: Rius-Peris JM, Marcilla Vázquez C, Molini Menchón N, Felipe Almira E, Silvestre Beneyto R, en representación del Grupo Investigador Proyecto ECEALHBA. Resurgimiento de los casos de bronquiolitis aguda tras la declaración del final del estado de alarma. An Pediatr (Barc). 2022;96:544–547.